
Suctioning semirigid ureteroscopic lithotomy versus minimally invasive percutaneous nephrolithotomy for large upper ureteral stones: a retrospective study
Introduction
Generally, a stone in the upper ureter larger than 10–15 mm is defined as a large upper ureteral stone (1). According to publications, the treatment modalities for these stones include extracorporeal shock wave lithotripsy (ESWL), transurethral lithotripsy, percutaneous nephrolithotomy (PCNL), retroperitoneal laparoscopic ureterolithotomy (RPLU) and open surgery (2,3). However, the best choice is controversial.
Recommended by European Association of Urology (EAU), ESWL is the first-line choice for upper ureteral stones that do not pass spontaneously; however, for large upper ureteral stones, the stone-free rate (SFR) is lower. Lopes Neto (4) reported that when upper ureteral stones were larger than 10 mm, the stone clearance rate with ESWL was only 35.7%. Although both PCNL and RPLU are associated with the highest success rates for large proximal ureteral calculi, many disadvantages also concern urologists, such as hemorrhage, postoperative pain, longer procedures, and longer hospital stays (4,5). Traditional semirigid ureteroscopic lithotomy (URSL) is more minimally invasive but is usually associated with various problems, especially a low SFR due to stone migration (6). The addition of flexible ureteroscopy as an adjunct to URSL can achieve satisfactory stone clearance; nonetheless, this procedure is costly and vulnerable.
To achieve better treatment outcomes with URSL, several additions and modifications to the procedures used to treat ureteral stones have been made (7-9). Recently, Li (10) and his colleagues reported that a novel semirigid Sotn ureterorenoscope was effective and safe for managing proximal ureteral and renal pelvic stones. In this study, we retrospectively investigated the difference and relative advantages between Sotn-URSL and PCNL in the management of large upper ureteral stones.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/tau-20-1218).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Xiangya Hospital, Central South University (No. 202009124) and informed consent was taken from all the patients.
Patients
After obtaining approval (Proof number: 202009124) from the Ethics Committee of Xiangya Hospital, Central South University, we reviewed the medical records of the patients in our institution between February 2018 and December 2019. The inclusion criteria were a patient age >18 years, stone localization between the lower border of the L4 spine and the ureteropelvic junction, and a longest stone diameter ≥1.5 cm, as revealed by unenhanced computed tomography (CT). The exclusion criteria were anatomic abnormalities of the urinary tract, pregnancy, active urinary tract infection, and a history of any intervention operation on the corresponding ureter.
According to the therapeutic methods, patients were divided into two groups: group 1 (Sotn-URSL) and group 2 [minimally percutaneous nephrolithotomy (mPCNL)]. The surgical choice was made by the patients, who balanced the benefits and risks after discussing the advantages and disadvantages of each procedure, including but not limited to bleeding, infectious complications, ureteral strictures and requirements of multi-session procedures. All relevant detailed demographic and clinical data were collected retrospectively and evaluated. Laboratory data included pre- and postoperative routine complete blood counts, serum creatinine, platelet counts, bleeding, coagulation profiles, and urine bacterial cultures. To control the infection, a sensitive antibiotic was given to the patients with positive cultures at least 5 days before the surgical intervention. In patients with negative baseline urine cultures, levofloxacin was given both 1 day and a half hour before the operation. Plain films of the kidney, ureter, and bladder (KUB), ultrasound scans and unenhanced CT scanning were performed in all patients preoperatively. Enhanced CT was performed when the creatinine value was within the normal range. The most important evaluation indicators were the SFR and complications before discharge. The SFR was defined as no stone fragments or residual fragments <3 mm according to postoperative follow-up KUB or unenhanced CT. Complications were evaluated and classified in accordance with the modified Clavien-Dindo classification system (11). Other indicators included the operation time, hospital stay after surgery, and stone migration ratio. The operation time was defined as the period from satisfactory anesthetic effects to completion of the operation.
Surgical procedures
All procedures were performed by the same urologist (Dr. HC) under general anesthesia.
Sotn-URSL
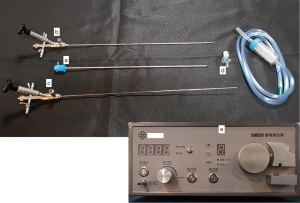
The Sotn ureteroscope (Sotn, ShuoTong Medical Co., Ltd., China; Figure 1) is also called the negative-pressure-combined ureteroscope and has five main components: (I) a Sotn ureteral access sheath (Sotn-UAS); (II) a standard ureteroscope; (III) a console ureteroscope; (IV) an adapter; (V) an irrigation and suctioning platform. All the specific parameters of this novel device have been described by Li and his colleagues (10).
Sotn-URSL was performed in the lithotomy position. First, the UAS was connected to the standard ureteroscope and inserted into the lower end of the stone. If the ureteroscope was unsuccessful in reaching the stone because of ureteral stenosis or kinking, a 6F double-J stent was inserted, and the second procedure was performed 2 weeks later. Second, the ureteroscope was disconnected and removed. The adapter with the dust container was connected to the UAS. The console ureteroscope was connected to the UAS with the assistance of an adapter. The other side of the dust container was connected to a suctioning system. The adapter was adjusted in real time by the surgeon to control negative pressure and prevent stone migration. The stone was fragmented with a holmium:YAG laser using a 200-µm laser fiber with an energy of 12–20 W at 20 Hz. The interspace between the shaft of the console ureteroscope and the UAS was enough to ensure continuous outflow by vacuum suctioning; furthermore, large fragments could be sucked out following the slow recession of the console ureteroscope. If stone migration occurred, flexible ureteroscopy was used with the Sotn-UAS. After fragmentation, a 6F double-J stent was routinely placed and was removed 2–4 weeks later.
mPCNL
This procedure was performed as previously described (12). Patients were placed in the lithotomy position, and a 5F ureteral catheter was inserted into the ipsilateral ureter. Then, the patient was rotated to the prone position. Ultrasound-guided percutaneous puncture was made by the urologist with an 18-gauge puncture needle that was pushed into the upper or middle renal calyx. The track was formed using Amplatz dilators until an 18F peel-away sheath was placed in the tract. An 8.0/9.8F rigid ureteroscope was used when the smaller tract was dilated. The stone was fragmented with a holmium:YAG laser using a 400-µm laser fiber with an energy of 30–40 W at 20 Hz. After fragmentation, the ureteral catheter was removed, and a 6F stent was inserted in an antegrade fashion. Subsequently, a 16F Foley catheter was inserted into the collecting system as a nephrostomy tube if significant bleeding was observed intraoperatively.
Statistical analyses
All calculations were performed using SPSS 22.0 statistical software. The continuous or categorical data are expressed as the mean ± standard deviation (SD) or percentile and frequency, as appropriate. Categorical variables were analyzed by the Chi-squared test (or Fisher’s exact test), and continuous variables were analyzed by independent-sample t-test. Differences were considered statistically significant at P<0.05 in all tests.
Results
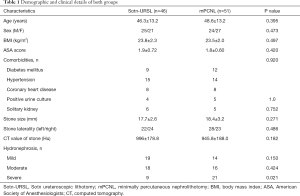
Forty-six patients were treated with Sotn-URSL, and 51 were treated with mPCNL. The details of the patient and disease characteristics are presented in Table 1. There was no statistically significant difference between the groups in terms of age, sex ratio, stone laterality, stone size, body mass index (BMI), CT value, comorbidity, or American Society of Anesthesiology (ASA) grade (P>0.05). However, a significant difference was observed in severe hydronephrosis (P=0.021), which may largely be due to case selection bias.
Full table
The designated procedure failed in three patients in the Sotn-URL group because it was difficult to reach the stone location. One of these patients then underwent mPCNL successfully after asking for his deputy’s opinion. The other two patients were treated with secondary Sotn-URL 4 weeks after placing the double-J stent. In the mPCNL group, one patient experienced failure because of ureteral kinking, and the stone was removed by retroperitoneal ureterolithotomy. The mean operation time was slightly longer in the mPCNL group (52.9±8.0 min) than in the Sotn-URSL group (50.5±5.9 min), but this difference did not reach statistical significance (P=0.106). Additionally, the mean hospital stay after surgery was significantly shorter in the Sotn-URSL group (1.4±0.6 vs. 2.3±0.7; P<0.001). Stone migration took place in three procedures in the Sotn-URSL group, and then the fragment was managed by f-URL through the Sotn-UAS. The cases that required f-URL management were categorized as having residual stones. A total of 67.4% (31/46) of patients in the Sotn-URSL group and 72.5% (37/51) in the mPCNL group received non-contrast CT (P=0.580), and the remaining patients received KUB in the two groups. The SFR after 1 month in the Sotn-URSL group was 89.1% (41/46), which was lower than that in the mPCNL group (50/51, 98%); however, there was no significant difference between the two groups (P=0.098).
According to the Clavien-Dindo classification, postoperative pain requiring analgesic therapy was observed in 3 and 11 patients in the Sotn-URSL and mPCNL groups, respectively (grade I, P=0.044). No significant difference was seen for other grade I complications, such as fever or vomiting. Postoperative fever requiring antibiotic therapy was observed in 3 and 2 patients in the Sotn-URSL and mPNL groups, respectively, and blood transfusion owing to a significant drop in hemoglobin was observed in 3 patients in the mPCNL group (grade II). These differences did not reach statistical significance (P=0.666, 0.244, respectively). Additionally, there was no significant difference between preoperative and postoperative serum creatinine in Sotn-URSL (85.2±24.4 vs. 81.0±21.3 µmol/L; P=0.87) or mPCNL group (89.9±25.1 vs. 87.8±23.0 µmol/L; P=0.67). No other complications from grade III to V were documented in the present study. The operative characteristics of both groups were listed in Table 2.

Full table
Discussion
Sotn-URSL has recently been reported as a safe and effective surgical method to treat renal and upper ureteral stones (10). Our study compared the safety and validity of Sotn-URSL and mPCNL in treating upper ureteral stones larger than 15 mm and discovered that there was no significant difference in terms of the SFR between Sotn-URSL and mPCNL; however, mPCNL was associated with a higher risk of postoperative complications and a longer hospital stay after surgery.
URSL through the natural human tract has been widely used to manage ureteral stones because of its minimal invasion and rapid recovery. However, a single URSL procedure usually fails to reach a satisfactory SFR. Preminger et al. reported that the success rate of URSL in treating upper ureteral calculi was only 77% (13). For upper ureteral calculi larger than 15 mm, traditional URSL faces multiple difficulties. For example, the calculi may escape to the pelvis or renal calyx, requiring additional f-URL (14), which is more costly to patients. Too many stone fragments will impact surgical vision and easily lead to secondary damage (15). Perfusion liquid cannot return effectively, and excessive intraoperative pressure will lead to postoperative pyrexia and even sepsis (16).
With the development of science and technology, f-URL has been widely used to manage renal calculi less than 20 mm (5). However, large upper ureteral calculi usually lead to hydronephrosis. When calculi return to the kidney, especially with severe hydronephrosis, stone fragments can barely be removed even after the use of f-URL (17). When Sotn-URSL is used, because of the relatively large space between the console ureteroscope and UAS as well as the balance between perfusion and negative-pressure suctioning, calculi can be attached to the end of the UAS to avoid calculus escape. Additionally, small stone fragments can also be suctioned out while relatively larger fragments are removed when withdrawing the ureteroscope, which is helpful for keeping a clear surgical view and improving the SFR (10). Moreover, in the current study, the SFR of Sotn-URSL (89.1%) was slightly higher than that of the previous study (86.5%) on Sotn-URSL reported by Li et al. (10), which may be largely attributed to the exclusion of patients with ipsilateral renal stones, and some of the inconsistency is also partly caused by the varied stone burden in different studies.
Since the introduction of PCNL in the 1970s, this technology has fundamentally changed the treatment of nephrolithiasis and is achieving constant improvements. A meta-analysis showed that mPCNL had better validity and safety than URL in treating impacted proximal ureteral calculi (18). Currently, PCNL has been recommended as the first treatment option for renal or upper ureteral calculi larger than 2 cm (5). The literature has shown that the success rate of PCNL in treating upper ureteral calculi larger than 15 mm is between 85% and 100% (19). According to our experience, because we usually use 18F mPCNL, almost all ureteral calculi above L4 can be managed through this method, except for a few challenging cases due to severe hydronephrosis or severe ureteral distortion. In this study, the PCNL group had an SFR of 98%, and 15 patients in this group had calculi whose largest diameter was larger than 2 cm; these were successfully removed. While the overall SFR of Sotn-URSL was 89.1%, the current study indicated that Sotn-URSL achieved similar treatment results to PCNL.
A large number of studies (19-21) have shown that URSL apparently has a shorter surgical time and a shorter postoperative hospitalization time than PCNL. We discovered that the overall surgical time of Sotn-URSL was the same as that of mPCNL, but the lithotripsy time of Sotn-URSL was longer than that of mPCNL. One possible explanation could be the use of 200-µm fibers with relatively smaller energy. Additionally, Garofalo et al. (22) demonstrated that tubeless PCNL significantly reduced postoperative pain assessment scores and shortened the hospitalization length. In our experience, we checked the tract by the end of mPCNL. If no obvious bleeding was observed, nephrostomy was not performed. The wide application of enhanced recovery after surgery (ERAS) technology in the perioperative period of mPCNL also shortened postoperative hospitalization. However, it was still significantly longer than that of Sotn-URSL.
Postoperative hemorrhage amounts to 14–24% of all patients managed by PCNL, among whom 0.8% need interventional embolization (23), which severely affects the safety of PCNL. Many studies reported that multiple tracts, staghorn stone, thick parenchyma and diabetes mellitus were independent risk factors of hemorrhage secondary to PCNL (24,25). In this study, the PCNL group had no patients requiring interventional embolization, but there were three patients experiencing blood transfusion after the operation. We found that these patients shared characteristics in thick parenchyma with mild hydronephrosis, and there were two cases in which the tract was not located in the fornix of renal calyx. Moreover, we considered the risk of bleeding as a potential disadvantage of mPCNL. Infection is another common complication associated with lithotripsy; in some severe cases, it may even cause life-threatening urine-derived sepsis that is close to high intraluminal pressure (16). We believe that the appropriate perioperative use of antibiotics and intraoperative pressure control are key measures to prevent this fatal complication.
In the current study, Sotn-URSL group has the advantages over mPCNL group in terms of the shorter hospital stay after surgery and less postoperative pain requiring analgesic therapy, and there was no significant difference between two groups regarding mean duration of surgery, SFR and other complications. In spite of it, the procedure should be tailored to those patients with upper ureteral stones larger than 15 mm. Considering the hemorrhage needing transfusion or even embolization as the potential complications for PCNL (16), patients with anatomic or functional solitary kidney were recommended for Sotn-URSL. On the other hand, mPCNL might be a preferential choice for patients with a history of ureteral strictures or distortion.
The limitation of the study is that it was a retrospective study. The surgical method choice impacted the study results to some extent. On the other hand, it lacked further assessment of long-term complications, especially postoperative ureteral strictures, despite that the injury of ureteral mucosa was not observed during the procedure of Sotn-URSL. Taken together, further well-designed studies with long-term follow-up are needed to confirmed the results of the current study.
Conclusions
In conclusion, the current study indicated that there was no significant difference in the safety or validity between Sotn-URSL and mPCNL for upper ureteral stones larger than 15 mm; however, Sotn-URSL had advantages over mPCNL in terms of a lower postoperative bleeding risk and a shorter postoperative hospitalization time. Therefore, we consider that both mPCNL and Sotn-URSL are suitable for upper ureteral stones with a diameter of >15 mm.
Acknowledgments
Funding: The present study was supported by the National Natural Science Foundation of China 81770705 (to HC).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/tau-20-1218
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tau-20-1218
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau-20-1218). The authors have no conflicts of interest to declare.
Ethical statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Xiangya Hospital, Central South University (No. 202009124) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhang Y, Yu CF, Jin SH, et al. A prospective comparative study between minimally invasive percutaneous nephrolithotomy in supine position and flexible ureteroscopy in the management of single large stone in the proximal ureter. Urology 2014;83:999-1002. [Crossref] [PubMed]
- Türk C, Petřík A, Sarica K, et al. EAU Guidelines on interventional treatment for urolithiasis. Eur Urol 2016;69:475-82. [Crossref] [PubMed]
- Zhao C, Yang H, Tang K, et al. Comparison of laparoscopic stone surgery and percutaneous nephrolithotomy in the management of large upper urinary stones: a meta-analysis. Urolithiasis 2016;44:479-90. [Crossref] [PubMed]
- Lopes Neto AC, Korkes F, Silva JL, et al. Prospective randomized study of treatment of large proximal ureteral stones: extracorporeal shock wave lithotripsy versus ureterolithotripsy versus laparoscopy. J Urol 2012;187:164-8. [Crossref] [PubMed]
- Mousavi Bahar SH, Amirhassani S, Nouralizadeh A, et al. Percutaneous nephrolithotomy versus laparoscopy in the management of large proximal ureteral stones: the experience of two different settings. Urol J 2019;16:448-52. [PubMed]
- Torricelli FC, Monga M, Marchini GS, et al. Semi-rigid ureteroscopic lithotripsy versus laparoscopic ureterolithotomy for large upper ureteral stones: a meta-analysis of randomized controlled trials. Int Braz J Urol 2016;42:645-54. [Crossref] [PubMed]
- Cabrera FJ, Preminger GM, Lipkin ME. Antiretropulsion devices. Curr Opin Urol 2014;24:173-8. [Crossref] [PubMed]
- AlSmadi JK, Li X, Zeng G. Use of a modified ureteral access sheath in semi-rigid ureteroscopy to treat large upper ureteral stones is associated with high stone free rates. Asian J Urol 2019;6:217-21. [Crossref] [PubMed]
- Du C, Song L, Wu X, et al. A study on the clinical application of a patented perfusion and suctioning platform and ureteral access sheath in the treatment of large ureteral stones below L4 level. Int Urol Nephrol 2019;51:207-13. [Crossref] [PubMed]
- Li K, Liao Z, Lin T, et al. A novel semirigid ureterorenoscope with vacuum suctioning system for management of single proximal ureteral and renal pelvic stones: an initial experience. J Endourol 2018;32:1154-9. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Chen HQ, Zeng F, Qi L, et al. Percutaneous nephrolithotomy in patients with scoliosis: our institutional experience. Urolithiasis 2013;41:59-64. [Crossref] [PubMed]
- Preminger GM, Tiselius HG, Assimos DG, et al. Guideline for the management of ureteral calculi. J Urol 2007;178:2418-34. [Crossref] [PubMed]
- Turkan S, Ekmekcioglu O, Irkilata L, et al. Is semi-rigid ureteroscopy sufficient in the treatment of proximal ureteralstones? When is combined therapy with flexible ureteroscopy needed? Springerplus 2016;5:30. [Crossref] [PubMed]
- Barbour ML, Raman JD. Incidence and predictors for ipsilateral hydronephrosis following ureteroscopic lithotripsy. Urology 2015;86:465-71. [Crossref] [PubMed]
- Jiang JT, Li WG, Zhu YP, et al. Comparison of the clinical efficacy and safety of retroperitoneal laparoscopic ureterolithotomy and ureteroscopic holmium laser lithotripsy in the treatment of obstructive upper ureteral calculi with concurrent urinary tract infections. Lasers Med Sci 2016;31:915-20. [Crossref] [PubMed]
- Chen HQ, Chen ZY, Zeng F, et al. Comparative study of the treatment of 20-30 mm renal stones with miniaturized percutaneous nephrolithotomy and flexible ureterorenoscopy in obese patients. World J Urol 2018;36:1309-14. [Crossref] [PubMed]
- Gao ZM, Gao S, Qu HC, et al. Minimally invasive percutaneous nephrolithotomy improves stone-free rates for impacted proximal ureteral stones: a systematic review and meta-analysis. PLoS One 2017;12:e0171230 [Crossref] [PubMed]
- Bozkurt IH, Yonguc T, Arslan B, et al. Minimally invasive surgical treatment for large impacted upper ureteral stones: ureteroscopic lithotripsy or percutaneous nephrolithotomy? Can Urol Assoc J 2015;9:E122-5. [Crossref] [PubMed]
- Wang Y, Zhong B, Yang X, et al. Comparison of the efficacy and safety of URSL, RPLU, and MPCNL for treatment of large upper impacted ureteral stones: a randomized controlled trial. BMC Urol 2017;17:50. [Crossref] [PubMed]
- Li H, Na W, Li H, et al. Percutaneous nephrolithotomy versus ureteroscopic lithotomy for large (>15 mm) impacted upper ureteral stones in different locations: is the upper border of the fourth lumbar vertebra a good indication for choice of management method? J Endourol 2013;27:1120-5. [Crossref] [PubMed]
- Garofalo M, Pultrone CV, Schiavina R, et al. Tubeless procedure reduces hospitalization and pain after percutenous nephrolithotomy: results of a multivariable analysis. Urolithiasis 2013;41:347-53. [Crossref] [PubMed]
- Ganpule AP, Shah DH, Desai MR. Postpercutaneous nephrolithotomy bleeding: aetiology and management. Curr Opin Urol 2014;24:189-94. [Crossref] [PubMed]
- Kukreja R, Desai M, Patel S, et al. Factors affecting blood loss during percutaneous nephrolithotomy: prospective study. J Endourol 2004;18:715-22. [Crossref] [PubMed]
- Li Z, Wu A, Liu J, et al. Risk factors for hemorrhage requiring embolization after percutaneous nephrolithotomy: a meta-analysis. Transl Androl Urol 2020;9:210-7. [Crossref] [PubMed]


