
99mTc-sulphur colloid lymphoscintigraphy and SPECT/CT in multiple primary lung cancer with chylothorax twice postoperatively
Introduction
Chylothorax is an uncommon complication of thoracic surgery, which is characterized by accumulation of chylous lymphatic fluid in the pleural cavity. Single-photon emission computed tomography with computed tomography (SPECT/CT) technology has evolved for evaluating chylothorax in recent years (1,2). Multiple primary lung cancer (MPLC) refers to two or more primary cancers in different sites of one or both lungs and can be classified as synchronous or metachronous (3,4). We herein report for the first time a rare case of synchronous MPLC with two chylothoraxes.
Case presentation
A 62-year-old man was admitted to our hospital for the assessment of nodules that were detected on chest radiography during a routine health check-up. He was a nonsmoker and denied symptoms including the presence of hoarseness, cough and dyspnea. Physical examination revealed normal breath sounds. Laboratory findings were within normal limits. Chest CT showed two obvious soft masses in the left upper lobe (LUL) and right upper lobe (RUL), measuring 2.0 cm × 2.0 cm and 2.5 cm × 2.0 cm, respectively. The edge of the right lesion was uneven and appeared lobulated on CT. The density of left one was different from that of the surrounding lung tissue, but the blood vessel texture could still be clearly observed. The patient refused CT-guided biopsy for both masses, and bronchoscopy was negative. As diagnosis was not established through imaging and considering the age and pulmonary function of the patient, surgery was scheduled twice, with a two-month interval. The patient was first subjected to right upper lobectomy with lymph node dissection (groups 2, 4, 7, 9, 10 and 11), and left upper lobectomy with lymph node dissection (groups 4, 5, 6, 7, 9, 10 and 11) was performed two months later using video-assisted thoracic surgery (VATS). Both lesions were pathologically adenocarcinomas, and the patient was diagnosed with synchronous multiple primary lung cancer, according to the Martini and Melamed criteria (5).
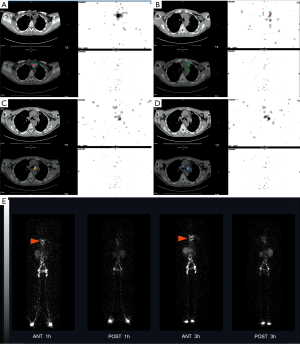
The patient had a chylothorax after the first surgery, with the triglyceride level of 260 mg/dL. The color of the pleural effusion was white, with the volume of 200 mL/day for 3 days, and conservative treatment was arranged for the patient. After the second surgery, postoperative persistent pleural effusion (approximately 300 mL/day for 5 days) raised a suspicion of chyle leaking again in this patient. The triglyceride level was 200 mg/dL, and the color of the pleural effusion was also white. Whole-body lymphoscintigraphy was performed in the anterior and posterior positions at 1 h and 3 h after injection of 99mTc-sulfur colloid into the subcutaneous regions of the bilateral dorsum pedis. Regional SPECT/CT of the thorax was performed, which revealed abnormal tracer accumulation in the left upper mediastinum beside the trachea, left side of the aorta and above the tracheal bifurcation (Figure 1A,B,C,D). Planar images showed abnormal tracer accumulation in the left hemithorax (Figure 1E). The patient felt well after conservative treatment, and the left-sided pleural effusion was shown to have disappeared on chest X-ray at the time of hospital discharge.
Discussion
Postsurgical chylothorax is relatively common (1.4–2.3% after lung resection), but two chylothoraxes in one patient, who was diagnosed with synchronous multiple primary lung cancer, are rare (6). The causes of chylothorax are grouped into several classes, as follows: tumor, trauma, idiopathic, and miscellaneous (7). It has been assumed that congenital malformation or inherent weakness may be present in cases without malignant or infectious disruption of the duct. Lymphoscintigraphy is now a common method of assessing lymphatic circulation, and it is a cheaper, faster and less invasive technique than lymphangiography (1,7,8). Recent rare case reports have revealed the accurate location of some tumors or lymph nodes using SPECT/CT (1,2,7,9), while using 99mTc-dextran lymphoscintigraphy and SPECT/CT may be more efficient than using 99mTc-sulfur colloid, as reported by Xia et al. Our patient clearly demonstrated the value of SPECT/CT, in addition to lymphoscintigraphy, for anatomical examination, providing a good definition of lymphatic leakage in the patient. Therefore, lymphoscintigraphy should be combined with SPECT/CT for the evaluation of all patients with suspected postoperative chylothorax.
Acknowledgments
We greatly appreciate the assistance of the staff of the Department of Thoracic Surgery, West-China Hospital, Sichuan University, and thank them for their efforts.
Funding: The Science and Technology Project of the Health Planning Committee of Sichuan (No.19PJ242) Sichuan Province Science and Technology Support Program (No.2020JDKP0023) Chengdu science and technology Support Program (No.2019-YFYF-00090-SN).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/qims-20-1205). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics committee board of West China Hospital and we have obtained patient’s consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Xia X, Shao F, Hu F, He Y, Cao W. (99m)Tc-dextran Lymphoscintigraphy SPECT/CT unveil the hidden leakage site in recurrent chylothoraxes. Ann Thorac Surg 2020;110:e465-7. [Crossref] [PubMed]
- Hou G, Jiang Y, Jing H, Xu W, Xu K, Chen L, Li F, Cheng W. Usefulness of 99mTc-ASC lymphoscintigraphy and SPECT/CT in the evaluation of rare lymphatic disorders: Gorham-Stout disease, lymphangioma, and lymphangioleiomyomatosis. Medicine 2020;99:e22414 [Crossref] [PubMed]
- Nie Y, Wang X, Yang F, Zhou Z, Wang J, Chen K. Surgical Prognosis of Synchronous Multiple Primary Lung Cancer: Systematic Review and Meta-Analysis. Clin Lung Cancer. 2020; Epub ahead of print. [Crossref] [PubMed]
- Chen TF, Xie CY, Rao BY, Shan SC, Zhang X, Zeng B, Lei YY, Luo HH. Surgical treatment to multiple primary lung cancer patients: a systematic review and meta-analysis. BMC Surg 2019;19:185. [Crossref] [PubMed]
- Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg 1975;70:606-12. [Crossref] [PubMed]
- Reisenauer JS, Puig CA, Reisenauer CJ, Allen MS, Bendel E, Cassivi SD, Nichols FC, Shen RK, Wigle DA, Blackmon SH. Treatment of Postsurgical Chylothorax. Ann Thorac Surg 2018;105:254-62. [Crossref] [PubMed]
- Momose M, Kawakami S, Koizumi T, Yoshida K, Kanda S, Kondo R, Kadoya M. Lymphoscintigraphy using technetium-99m HSA-DTPA with SPECT/CT in chylothorax after childbirth. Radiat Med 2008;26:508-11. [Crossref] [PubMed]
- Bae JS, Yoo RE, Choi SH, Park SO, Chang H, Suh M, Cheon GJ. Evaluation of lymphedema in upper extremities by MR lymphangiography: Comparison with lymphoscintigraphy. Magn Reson Imaging 2018;49:63-70. [Crossref] [PubMed]
- Weiss M, Schwarz F, Wallmichrath J, Baumeister R, Frick A, Bartenstein P, Rominger A. Chylothorax and chylous ascites. Clinical utility of planar scintigraphy and tomographic imaging with SPECT/CT. Nuklearmedizin 2015;54:231-40. [Crossref] [PubMed]


