Robotic-assisted thoracoscopic right upper lobe sleeve resection
Introduction
Sleeve lobectomy is indicated for centrally located lung cancer as an alternative to pneumonectomy. It has mainly been performed by thoracotomy because of the complexity of airway reconstruction. With new technical advances and more experience gained in video-assisted thoracic surgery (VATS), sleeve lobectomy performed by VATS has been reported, but its suitability is limited by its lack of depth perception and maneuverability. The robotic-assisted technology with 3D visibility and mechanical wrists which enable more bend and rotation than the human hand, has made these complex procedures safer and easier, especially in the reconstruction of airways. Through the video presented here (Figure 1), we will report our experience of a robotic-assisted thoracoscopic right upper sleeve lobectomy.
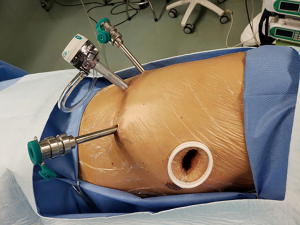
Anesthesia, posture and incision option
This patient was treated with double-lumen endotracheal intubation, general anesthesia, intraoperative single-lung ventilation, and placed in contralateral decubitus position, with the upper extremities in flexion and holding a pillow. The operating bed was adjusted to turn the torso into a slight upward-folding position in order to passively widen the intercostal space. Da Vinci surgery completed lobectomy and systemic lymph node dissection through the arms and auxiliary port. These were the positions of the ports (Figure 2): the camera port was generally in the axillary midline at the 7th intercostal space. The left and right arms were located in the same horizontal plane as the camera port, and the distance between the arms was around 8 to 10 cm to facilitate overall motion and to reduce the direct collision of arms that would interfere with smooth surgery. The auxiliary port was in the 4th intercostal space at the anterior axillary line.
Surgical technique
The camera was inserted through trocar at the targeted position. After examining the thoracic cavity to ensure no extensive adhesion, carbon dioxide was pumped to ensure clear vision and to accelerate residual gas discharging in the lungs. Then the two arms were put into position, and the bedside arm system was docked. Generally, the right arm carried the cautery hook, and the left arm carried the Cadiere forceps. We started with exposing the entire right main bronchus by cutting the posterior pleura with the cautery hook. The subcarinal lymph nodes were removed from the intermediate bronchus, and separated from the esophagus with Cadiere forceps. En bloc resection of station seven and eight lymph nodes were performed by exposing the left main bronchus and carina. The horizontal fissure was divided to expose the upper lobar bronchus and intermediate bronchus by dissecting the lymph nodes around them. The upper lobar bronchus and intermediate bronchus were cut with the cautery hook, guaranteeing negative margins by frozen pathology examination. The bronchial stump was lifted by the assistant with the oval forceps, and the upper pulmonary artery was exposed clearly after the bronchus detached, which greatly increased the operation space. The tunnel technique was employed in dissecting the horizontal fissure with an endo-stapler after the apical anterior segmental artery was divided and the surrounding lymph nodes were removed. After this, the artery and vein were thoroughly divided, and cut off by endo-stapler. The right upper lobe resection was now finished. During the dissection of the superior mediastinal lymph nodes, the pleura between the arch of the azygos vein and the right main bronchus was opened, followed by the dissection of the station 4 lymph nodes among the bronchus and superior vena cava. Superior mediastinal lymph nodes were dissected en bloc off the superior vena cava, arch of the azygos vein, and trachea. The anastomosis was performed through two running Prolene suture 3-0. The continuity of the suture was guaranteed by tying the two sutures through a double knot. In this step, the right arm carried the needle holder, instead of the cautery hook. The suture was started from the caudal corner of the pars cartilaginea to the pars membranacea, toward the anterior bronchial wall. The tension of the suture was assessed at each step. Once concluded, the integrity of the anastomosis was checked through irrigation. Apical and basal drainage tubes were each individually placed before complete hemostasis and stitching of the incision.
Comments
After the first case of minimally invasive sleeve lobectomy conducted by VATS was reported in 2002 (2), a series of cases were reported during the following 10 years (3-7), addressing comparable morbidity, mortality, and survival rate of VATS sleeve lobectomy and thoracotomy. The main technical challenges of minimally invasive sleeve resection are the bronchial anastomosis and steep learning curve of the procedure (8).
Recently, the da Vinci robotic surgical system has come of age. Here, we present the advantages of this surgical system, in terms of depth perception and higher quality images from the binocular camera over the classic 2-dimensional VATS. In addition, the ability of flexible movement and rotation in an additional four degrees of freedom of the robotic instruments offers a wide range of maneuvers during operation. Moreover, the robotic system can improve precision by tremor filtration and elimination of the fulcrum effect, thus reducing the risk of human error. All the above cumulative improvements, which enable precision resection and accurate stitching, ultimately result in a safer thoracic surgical approach (9). Importantly, the novel surgical system also simplifies some difficult procedures in classic VATS, such as suturing and knot tying (10).
Sleeve lobectomy conducted by a robotic surgical system was first reported by Doctor Schmid in 2011 (11). Presently, our robotic surgery team, with the experience of more than 20 consecutive cases, combine the advantages of a minimally invasive procedure with the precision of the robotic dissection and suture, especially in the reconstruction of airways. Nevertheless, nowadays in China, the application of a robotic surgical system also has some potential drawbacks. For example, the cost of robotic surgery is higher; in our institute, an extra 30,000 RMB (approximately 4,300 USD) would be paid for the robotic surgery. Significantly, one of the disadvantages of robotic surgery is the absence of tactile sense during the entire surgical procedure. After we have finished more than 1,000 robotic surgeries with a single surgeon and the same team, the surgeon, who would then be extensively experienced, could then be able to partially compensate for the lack of haptic feedback via more learned visual observation when suturing and knot tying. The concerns involving minimally invasive surgery reported by M.D. Anderson Cancer Center were noted (12). Despite this, the safety and feasibility of minimally invasive technologies in thoracic surgery, including robotic surgical system, have been proven by many retrospective and prospective studies (13-17). Even so, further prospective studies in this field should also be encouraged to provide further evidence for minimally invasive thoracic surgery.
Acknowledgements
Funding: This work was supported by the Shanghai Hospital Development Center (SHDC12016113).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Huang J, Li C, Jiang L, et al. The video of right upper lobe sleeve resection. Asvide 2019;6:013. Available online: http://www.asvide.com/article/view/29627
- Santambrogio L, Cioffi U, De Simone M, et al. Video-assisted sleeve lobectomy for mucoepidermoid carcinoma of the left lower lobar bronchus: a case report. Chest 2002;121:635-6. [Crossref] [PubMed]
- Mahtabifard A, Fuller CB, McKenna RJ Jr. Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg 2008;85:S729-32. [Crossref] [PubMed]
- Li Y, Wang J. Video-assisted thoracoscopic surgery sleeve lobectomy with bronchoplasty: an improved operative technique. Eur J Cardiothorac Surg 2013;44:1108-12. [Crossref] [PubMed]
- He J, Shao W, Cao C, et al. Long-term outcome of hybrid surgical approach of video-assisted minithoracotomy sleeve lobectomy for non-small-cell lung cancer. Surg Endosc 2011;25:2509-15. [Crossref] [PubMed]
- Agasthian T. Initial experience with video-assisted thoracoscopic bronchoplasty. Eur J Cardiothorac Surg 2013;44:616-23. [Crossref] [PubMed]
- Chen H, Huang L, Xu G, et al. Modified bronchial anastomosis in video-assisted thoracoscopic sleeve lobectomy: a report of 32 cases. J Thorac Dis 2016;8:2233-40. [Crossref] [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy:3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [Crossref] [PubMed]
- LaPietra A, Grossi EA, Derivaux CC, et al. Robotic-assisted instruments enhance minimally invasive mitral valve surgery. Ann Thorac Surg 2000;70:835-8. [Crossref] [PubMed]
- Kitagawa M, Dokko D, Okamura AM, et al. Effect of sensory substitution on suture-manipulation forces for robotic surgical systems. J Thorac Cardiovasc Surg 2005;129:151-8. [Crossref] [PubMed]
- Schmid T, Augustin F, Kainz G, et al. Hybrid video-assisted thoracic surgery-robotic minimally invasive right upper lobe sleeve lobectomy. Ann Thorac Surg 2011;91:1961-5. [Crossref] [PubMed]
- Ramirez PT, Frumovitz M, Pareja R, et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N Engl J Med 2018;379:1895-904. [Crossref]
- Long H, Tan Q, Luo Q, et al. Thoracoscopic Surgery Versus Thoracotomy for Lung Cancer: Short-Term Outcomes of a Randomized Trial. Ann Thorac Surg 2018;105:386-92. [Crossref] [PubMed]
- Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006;244:420-5. [PubMed]
- Walker WS, Codispoti M, Soon SY, et al. Long-term outcomes following VATS lobectomy for non-small cell bronchogenic carcinoma. Eur J Cardiothorac Surg 2003;23:397-402. [Crossref] [PubMed]
- Shigemura N, Akashi A, Nakagiri T, et al. Complete versus assisted thoracoscopic approach: a prospective randomized trial comparing a variety of video-assisted thoracoscopic lobectomy techniques. Surg Endosc 2004;18:1492-7. [Crossref] [PubMed]
- Hennon M, Sahai RK, Yendamuri S, et al. Safety of thoracoscopic lobectomy in locally advanced lung cancer. Ann Surg Oncol 2011;18:3732-6. [Crossref] [PubMed]