Complete excision of acute necrotic regression of thymoma mimicking an infected mediastinal cyst with mediastinitis using video-assisted thoracoscopic technique
Introduction
Thymomas are rare and demonstrate indolent growth (1). Because all thymoma are considered malignant due to local invasion or dissemination, wide surgical excision, such as total thymectomy without biopsy is the treatment of choice for both diagnosis and therapy (1-3). Ischemic infarction and necrosis may occur in tumors, usually due to outgrowing the nutrient supply (4). Diagnosis is difficult because clinical and radiologic characteristics of acute spontaneous regression of a thymoma are not defined and this process is very unusual (4,5). Herein, we report a case of complete excision of acute necrotic regression of a thymoma mimicking an infected mediastinal cyst with mediastinitis using the video- assisted thoracoscopic surgery (VATS) technique.
Case presentation
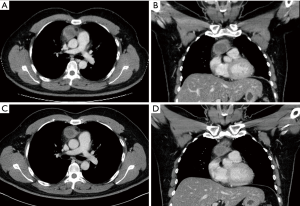
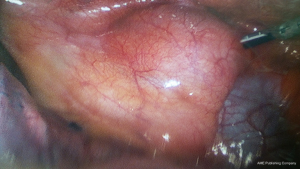
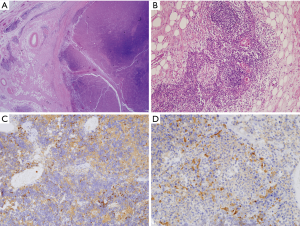
A 43-year-old Korean man was referred to our department for acute infection of a mediastinal cyst with mediastinitis. The patient presented with chest pain and dyspnea four days prior. Initial chest computed tomography (CT) revealed a 4.5 cm × 3.2 cm cystic lesion in the anterosuperior mediastinum. The lesion had a thickened and enhanced wall and infiltrated around tissues. These findings suggested an infected benign mediastinal cyst, such as an infected thymic cyst or abscess, or a ruptured dermoid cyst accompanied by acute mediastinitis (Figure 1A,B). Esophagogram did not show any abnormalities. Because the patient was considered to have an acute infected cyst and surgical excision can be hazardous and incomplete during severe inflammation, conservative treatment including antibiotic therapy was initiated to relieve inflammation. After one week of the conservative treatment, his symptoms were resolved, laboratory findings returned to normal levels, and chest CT showed regression of the cystic lesion and improvement of mediastinitis (Figure 1C,D). The lesion was excised using conventional 3-port VATS with carbon dioxide insufflation. The cyst was slightly adherent to nearby organs and extended from the thymus. Total thymectomy was performed using entirely VATS technique because the cyst was extended from the thymus and pathology was not confirmed (Figure 2). Frozen section was non-diagnostic due to severe necrosis and no identification of viable tumor cells. The final histopathological examination including the immunohistochemistry study revealed that the lesion was a totally necrotic thymoma with an unidentified cell type. There was no capsular invasion by the tumor cells (Figure 3). The patient’s postoperative course was uneventful. He was discharged on the seventh postoperative day without complications. No adjuvant therapy was conducted, and recurrence was not identified six months after surgery.
Discussion
Like this case report, ischemic infarction and necrosis in tumors usually occurs due to outgrowing of the nutrient supply, and spontaneous regression of a thymoma has been also reported (4). However, the diagnosis of spontaneous regression in thymoma is difficult because the clinical and radiologic characteristics are not defined and this process is extremely unusual (2,5).
Because the patient in our case was considered to have an acute infected cyst and surgical excision can be hazardous and incomplete during acute inflammation, conservative treatment including antibiotic therapy was initiated to relieve inflammation (1). Because the cystic lesion regressed and inflammation decreased after one week of antibiotic therapy, the lesion was considered an infected thymic cyst or abscess. However, because its pathology was not confirmed and the cyst extended from the thymus, total thymectomy was performed instead of a simple excision. Frozen section was not diagnostic due to severe necrosis. Final histopathology reports including immunohistochemistry revealed that the lesion was a totally necrotic thymoma. The histologic cell type was not identified due to severe necrosis, and there was no capsular invasion by the tumor cells. The overall findings indicated that the lesion was totally necrotic regression of a thymoma with an unidentified cell type. Because it was a complete resection with no capsular invasion by the tumor cells, no adjuvant therapy was conducted.
Because the International Thymic Malignancy Interest Group panel agreed that even type A and AB thymomas have malignant potential, wide surgical excision, including total thymectomy without biopsy, is the treatment of choice for both diagnosis and therapy (1,3). Although the clinical outcomes after a simple excision remain unclear due to its rarity, total thymectomy should also be considered even in spontaneous regression of a thymoma due to its malignant potential (1,3). We suggest that total thymectomy should be considered even if the lesion is suspected to be a benign thymic cyst or abscess because there are cystic thymomas and acute spontaneous regression of a thymoma is also possible (2).
In conclusion, this is a rare case report of acute totally necrotic regression of a thymoma. We describe why total thymectomy using VATS should be considered, even among patients with a benign appearing thymic cyst or abscess.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Girard N. Thymic epithelial tumours: from basic principles to individualised treatment strategies. Eur Respir Rev 2013;22:75-87. [Crossref] [PubMed]
- Carter BW, Benveniste MF, Madan R, et al. ITMIG Classification of Mediastinal Compartments and Multidisciplinary Approach to Mediastinal Masses. Radiographics 2017;37:413-36. [Crossref] [PubMed]
- Wu J, Fang W, Chen G. The enlightenments from ITMIG Consensus on WHO histological classification of thymoma and thymic carcinoma: refined definitions, histological criteria, and reporting. J Thorac Dis 2016;8:738-43. [Crossref] [PubMed]
- Fukui T, Taniguchi T, Kawaguchi K, et al. Spontaneous regression of thymic epithelial tumours. Interact Cardiovasc Thorac Surg 2014;18:399-401. [Crossref] [PubMed]
- Li X, Han X, Sun W, et al. Preoperative misdiagnosis analysis and accurate distinguish intrathymic cyst from small thymoma on computed tomography. J Thorac Dis 2016;8:2086-92. [Crossref] [PubMed]


