Mitral valve repair versus replacement in elderly patients: a systematic review and meta-analysis
Introduction
Mitral valve repair (MVP) is the procedure of choice in adult patients with mitral valve disease, especially mitral insufficiency, as it has been shown to offer superiority over mitral valve replacement (MVR) in various clinical settings (1). Because of the demographic changes worldwide and a greater incidence of mitral valve disease, the elderly population constitutes an increasing proportion of patients referred for mitral valve surgery (2). A number of disorders may damage the valve in older patients, such as degeneration, ischemia, and rheumatic heart disease, resulting in mitral valve stenosis or regurgitation. Although it is generally accepted that surgical treatment should be implemented even in elderly patients, there remains debate regarding whether MVP produces the equivalent benefits as in younger population (3).
Despite the advantages over MVR, in the elderly patients, MVP is less commonly performed when comparing with younger patients. According to the data from Medicare beneficiaries’ database, less than 50% of elderly patients with mitral valve disease underwent MVP, and older age could predict a higher possibility of MVR (4). This reflects the perception that MVP may be associated with longer operative time and more complicated procedures. Besides, the long-term survival benefit after MVP is often believed to be attenuated in the elderly because of their shorter life expectancy. There is also a notion that elderly patients have more friable or calcified valvular tissues and poor left ventricular function as compared to younger patients, making repair technically more challenging, thus precluding the satisfaction of valve repair and increasing the risk of reoperation (5,6).
Although the outcomes following mitral valve surgery in older patients have improved significantly in recent years (7), it is still unclear which surgical approach should be performed preferentially. Moreover, innovative transcatheter mitral interventions are increasingly used to treat mitral valve disease (8) and, thus, should be evaluated against the outcomes of optimal surgical treatment. There are limited studies, however, regarding the efficacy of MVP vs. MVR in the elderly population, and their results are inconsistent. We, therefore, carried out a systematical review and meta-analysis to determine the optimum surgical treatment for mitral valve disease in elderly patients.
Methods
Search strategy
This study was conducted following the guidance of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement (9). We systematically searched databases of PubMed, the Cochrane Library, and Scopus through February 2017 to identify eligible publications, using the search terms as follows: “mitral valve repair”, “mitral valve replacement”, and “elderly” or “older” or “octogenarian”. Moreover, the reference lists of all retrieved articles were also checked for inclusion of potentially relevant studies.
Eligibility criteria
To be included, the studies should meet all of the following requirements: (I) clinical trials or observational studies that compared MVP vs. MVR in patients aged 70 years or older; (II) with more than ten patients in either the MVP or MVR group; (III) have reported the early and late outcomes we focused on. All articles were limited to those involving human subjects and published in English. Reviews, editorials, duplications, abstracts, conference presentations, and expert opinions were excluded. In addition, the technique of MVP was not established and prevailed prior to 2000, and the outcomes in those eras were not as good as the current data. Therefore, we also discarded the studies that were published before 2000.
Data abstraction and quality assessment
In general, two reviewers (X Shang and R Lu) independently extracted the study information, including study author, publication year, study period and design, location, inclusion criteria of age, sample size, follow-up duration, and patients’ characteristics. Early outcomes in this meta-analysis were 30-day mortality, duration of postoperative hospital stay, and postoperative complications. Late outcomes included 1- and 5-year survival and reoperation during follow-up. Methodological quality of included studies was evaluated using Newcastle-Ottawa Scale (NOS), with the following three main aspects: study group selection, comparability between groups, and ascertainment of outcomes (10). A study with a NOS score of 7 or higher was regarded as of high quality. Any disagreements in data collection and quality evaluation were settled by consensus between the two reviewers or discussion with a third reviewer (M Liu).
Statistical methods
In the present study, categorical endpoints were reported as risk ratios (RRs) with corresponding 95% confidence intervals (CIs), while continuous outcomes were presented as weighted mean differences (WMDs). We calculated the pooled estimates using random effects model with DerSimonian-Laird method. Heterogeneity across studies was investigated by the Cochran Q test with a significant level of P<0.1. In addition, we used the I2 statistic to quantify the heterogeneity, with an I2 value >50% indicating substantial heterogeneity. Sensitivity analyses were performed by omitting each study in sequence. Publication bias was assessed by visual inspection of funnel plots and further confirmed by Egger’s test. All data analyses were carried out using Review Manager 5.3 (RevMan, The Nordic Cochrane Center, The Cochrane Collaboration, 2012, Copenhagen, Denmark) and STATA 12.0 software (Stata Corp, College Station, TX, USA), and a two-sided P value of <0.05 was considered statistically significant.
Results
Study search
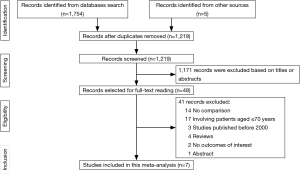
The study selection process was summarized in Figure 1. In general, of the initial 1,759 publications, 1,171 were excluded based on the titles or abstracts. The remaining 48 articles were selected for full-text reading, of which 41 reports that failed to meet the eligibility criteria were eliminated. Consequently, seven observational studies (11-17) that were published from 2004 to 2016 were included in our meta-analysis.
Baseline characteristics
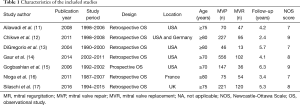
The study characteristics were exhibited in Table 1. Briefly, of the included observational studies, 6 were retrospective and 1 was prospective. These included data on a total of 1,809 patients with mitral valve disease, of which 1,342 patients receiving MVP and 467 undergoing MVR. Among the included studies, 4 were from USA, 2 were from Europe, and the remaining 1 was conducted in both USA and Europe, with the mean or median follow-up durations ranging from 2.4 to 6.3 years. The mean age of patients was 79 years, and men accounted for 51% of the total patients. Other patients’ characteristics were shown in Table S1. Quality assessment showed a NOS score of 7 or higher for all studies, indicating the presence of high methodological quality.
Full table

Full table
Early outcomes
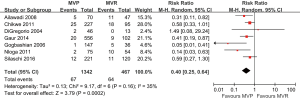
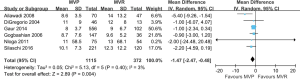
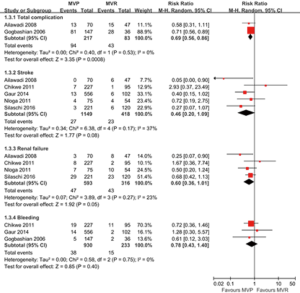
The 30-day mortality was 5.0% in the MVP group and 13.7% in the MVR group, with no evidence of substantial heterogeneity across studies (I2=35%, P=0.16). Compared with MVR, surgery with MVP was associated with a significantly decreased 30-day mortality in elderly patients (RR: 0.40, 95% CI: 0.25–0.64, P<0.001; Figure 2). The duration of postoperative hospital stay (days) was also shortened following MVP (WMD: −1.47, 95% CI: −2.47–−0.48, P=0.004; Figure S1). In addition, there was a reduction in total postoperative complications in patients receiving MVP than those undergoing MVR (RR: 0.69, 95% CI: 0.56–0.86, P<0.001; Figure S2). Among the complications, stoke and renal failure were nominally lower in the MVP than in the MVR groups (RR: 0.46, 95% CI: 0.20–1.09, P=0.08 and RR: 0.60, 95% CI: 0.36–1.01, P=0.05, respectively), while there was no difference in terms of bleeding between these two strategies.
Late outcomes
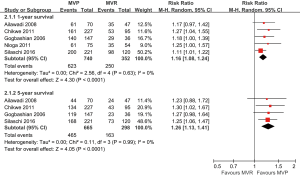
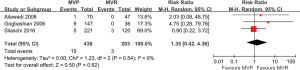
The meta-analytic results of late survivals were shown in Figure 3. The 1-year survival rate was 84.2% and 71.0% in the MVP and MVR groups, respectively, with no evident heterogeneity across studies (I2=0%, P=0.63). Pooling data indicated that MVP was related to a significantly improved 1-year survival (RR: 1.16, 95% CI: 1.08–1.24, P<0.001). Likewise, the 5-year survival rate was 69.9% in the MVP group and 54.7% in the MVR group, without considerable heterogeneity among studies (I2=0%, P=0.99). Meta-analytic pooling demonstrated that the 5-year survival was higher in patients treated with MVP than those treated with MVR (RR: 1.26, 95% CI: 1.13–1.41, P<0.001). However, the risk of reoperation during follow-up was similar between MVP and MVR (RR: 1.35, 95% CI: 0.42–4.36, P=0.62; Figure S3).
Sensitivity analysis and publication bias
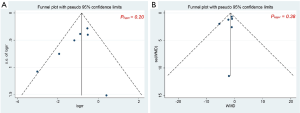
Exclusion of each study in sequence had no influence on the overall results of 30-day mortality, duration of postoperative hospital stay, and 1- and 5-year survivals. The funnel plots for 30-day mortality and duration of postoperative hospital stay were visually symmetrical (Figure S4) with P values of Egger’s test =0.20 and 0.38, respectively, suggesting the absence of publications bias. For other outcomes, publication bias test was not performed due to the limited number of included studies.
Discussion
Few studies have explored the comparison between MVP and MVR among the aging population. The present meta-analysis pooling available data demonstrated that compared with MVR, MVP was associated with a significantly lower 30-day mortality, with shorter duration of postoperative hospital stay and less postoperative complications. In addition, the 1- and 5-year survival rates have improved after MVP, with no difference regarding reoperation events during follow-up.
Our findings are consistent with a previous meta-analysis, which showed that MVP was correlated with improved early outcomes as compared to MVR in elderly patients (18). In that study, only four clinical studies were included, totaling 402 patients with mitral valve disease. The present work additionally included four observational studies and excluded studies prior to 2000, with nearly 4.5-fold increase in sample size, thus offering more reliable insights into the optimal mitral surgical procedures in older patients. In contrast, some studies of the aging population have reported similar long-term survival between MVP and MVR. For instance, a previous retrospective study (19) revealed that the 5-year survival of patients aged 60 years or older was not remarkably higher in patients undergoing MVP than those undergoing MVR (36% vs. 33%, P=0.34). However, the study cohort was historical involving patients treated between 1984 and 1997. Given the overall prolonged life expectancy and the improved perioperative management in cardiac surgery (20), MVP should have led to more favorable outcomes currently. In the present study, we did not specially explore the potential factor accounting for the improved outcomes after MVP; however, they can be summarized from the other available evidence. First of all, MVP allows better preservation of normal mitral or subvalvular apparatus than MVR that is important for ventricular contraction, thereby improving left ventricular function and remodeling (21-23). In addition, it has been suggested that there are fewer thromboembolic events and life-threatening hemorrhages in patients with MVP than those with MVR (24), thus reducing the deaths from these causes.
Because of the rapid demographic changes and the high prevalence of mitral valve disease in the elderly population, our findings are of great clinical importance. Older patients are often considered as poor candidates for MVP owning to the difficulty of repair and the conception that they may not tolerate a longer cardiopulmonary bypass time for achieving an adequate repair (14). However, out data suggest that both early and late outcomes have improved with MVP, certainly when compared with MVR, pointing towards that MVP should be the preferred procedure for mitral valve surgery in the elderly group of patients. In addition, the available treatment strategies for mitral valve disease is developing rapidly towards interventional strategies to repair or replace the mitral valve with aims to reduce the surgical trauma and to improve outcomes, particularly in the elderly patients (8). However, new techniques to be introduced into clinical practice should have to be measured against the optimum conventional treatment, such as MVP in our study.
There are several limitations that should be acknowledged in our work. Firstly, all included studies are designed as prospective or retrospective observational studies with relatively small sample size, which may increase the risk of selection bias and reduce the statistical power for some complications. Secondly, because of insufficient data, we cannot perform stratified analyses by some important confounders, such concomitant surgical procedures and prosthesis for replacement. Furthermore, data in the present meta-analysis were obtained from studies conducted in USA or Europe. Thus, generalization of our findings to other populations should be used with caution.
Conclusions
Taken together, our meta-analysis shows that MVP is associated with significantly improved early and late outcomes as compared to MVR in the elderly patients. However, these findings should be considered within the observational nature of current evidence. Future larger studies, or perhaps randomized trials, are required to enhance the benefit of MVP vs. MVR in the aging population.
Acknowledgements
Funding: This work was supported by grants from the National Key Research and Development Program of China to Nianguo Dong (grant No. 2016YFA0101103).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: All analyses were based on previously published studies, thus no ethical approval and patient consent are required.
References
- Nishimura RA, Vahanian A, Eleid MF, et al. Mitral valve disease--current management and future challenges. Lancet 2016;387:1324-34. [Crossref] [PubMed]
- Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study. Lancet 2006;368:1005-11. [Crossref] [PubMed]
- Ghoreishi M, Dawood MY, Gammie JS. Mitral valve surgery in elderly patients with mitral regurgitation: repair or replacement with tissue valve? Curr Opin Cardiol 2013;28:164-9. [Crossref] [PubMed]
- Vassileva CM, Mishkel G, McNeely C, et al. Long-term survival of patients undergoing mitral valve repair and replacement: a longitudinal analysis of Medicare fee-for-service beneficiaries. Circulation 2013;127:1870-6. [Crossref] [PubMed]
- Gillinov AM, Blackstone EH, Nowicki ER, et al. Valve repair versus valve replacement for degenerative mitral valve disease. J Thorac Cardiovasc Surg 2008;135:885-93, 893.e1-2.
- Gillinov AM, Cosgrove DM, Blackstone EH, et al. Durability of mitral valve repair for degenerative disease. J Thorac Cardiovasc Surg 1998;116:734-43. [Crossref] [PubMed]
- Biancari F, Schifano P, Pighi M, et al. Pooled estimates of immediate and late outcome of mitral valve surgery in octogenarians: a meta-analysis and meta-regression. J Cardiothorac Vasc Anesth 2013;27:213-9. [Crossref] [PubMed]
- Maisano F, Alfieri O, Banai S, et al. The future of transcatheter mitral valve interventions: competitive or complementary role of repair vs. replacement? Eur Heart J 2015;36:1651-9. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [Crossref] [PubMed]
- Wells GA, Shea B, O'Connell D, et al. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- Ailawadi G, Swenson BR, Girotti ME, et al. Is mitral valve repair superior to replacement in elderly patients? Ann Thorac Surg 2008;86:77-85; discussion 86. [Crossref] [PubMed]
- Chikwe J, Goldstone AB, Passage J, et al. A propensity score-adjusted retrospective comparison of early and mid-term results of mitral valve repair versus replacement in octogenarians. Eur Heart J 2011;32:618-26. [Crossref] [PubMed]
- DiGregorio V, Zehr KJ, Orszulak TA, et al. Results of mitral surgery in octogenarians with isolated nonrheumatic mitral regurgitation. Ann Thorac Surg 2004;78:807-13; discussion 813-4. [Crossref] [PubMed]
- Gaur P, Kaneko T, McGurk S, et al. Mitral valve repair versus replacement in the elderly: short-term and long-term outcomes. J Thorac Cardiovasc Surg 2014;148:1400-6. [Crossref] [PubMed]
- Gogbashian A, Sepic J, Soltesz EG, et al. Operative and long-term survival of elderly is significantly improved by mitral valve repair. Am Heart J 2006;151:1325-33. [Crossref] [PubMed]
- Nloga J, Hénaine R, Vergnat M, et al. Mitral valve surgery in octogenarians: should we fight for repair? A survival and quality-of-life assessment. Eur J Cardiothorac Surg 2011;39:875-80. [Crossref] [PubMed]
- Silaschi M, Chaubey S, Aldalati O, et al. Is Mitral Valve Repair Superior to Mitral Valve Replacement in Elderly Patients? Comparison of Short- and Long-Term Outcomes in a Propensity-Matched Cohort. J Am Heart Assoc 2016;5:e003605. [Crossref] [PubMed]
- Markar SR, Sadat U, Edmonds L, et al. Mitral valve repair versus replacement in the elderly population. J Heart Valve Dis 2011;20:265-71. [PubMed]
- Thourani VH, Weintraub WS, Guyton RA, et al. Outcomes and long-term survival for patients undergoing mitral valve repair versus replacement: effect of age and concomitant coronary artery bypass grafting. Circulation 2003;108:298-304. [Crossref] [PubMed]
- Nicolini F, Agostinelli A, Vezzani A, et al. The evolution of cardiovascular surgery in elderly patient: a review of current options and outcomes. Biomed Res Int 2014;2014:736298. [Crossref] [PubMed]
- Pitarys CJ 2nd, Forman MB, Panayiotou H, et al. Long-term effects of excision of the mitral apparatus on global and regional ventricular function in humans. J Am Coll Cardiol 1990;15:557-63. [Crossref] [PubMed]
- Greenhouse DG, Dellis SL, Schwartz CF, et al. Regional changes in coaptation geometry after reduction annuloplasty for functional mitral regurgitation. Ann Thorac Surg 2012;93:1876-80. [Crossref] [PubMed]
- Candan O, Ozdemir N, Aung SM, et al. Effect of mitral valve repair versus replacement on left ventricular rotational deformation: a study with speckle tracking echocardiography. J Heart Valve Dis 2013;22:651-9. [PubMed]
- Russo A, Grigioni F, Avierinos JF, et al. Thromboembolic complications after surgical correction of mitral regurgitation incidence, predictors, and clinical implications. J Am Coll Cardiol 2008;51:1203-11. [Crossref] [PubMed]