Medical thoracoscopy in China—the present status and the future
Introduction
Unexplained exudative pleural effusion after repeated thoracentesis are frequent causes for referral for diagnostic evaluation. However, the differential diagnosis of pleural effusions sometimes represents a considerable challenge. About 20–40% of patients with pleural effusion remain undiagnosed despite pleural fluid analysis and closed biopsy (1,2), and medical thoracoscopy (MT) is well established to increase the diagnostic yield in these cases (1,3). MT refers to a minimally invasive procedure to inspect and perform a biopsy of the pleural space, as well as to perform therapeutic interventions, in a nonintubated patient under local anesthesia. This procedure can be traced back to nearly one hundred years ago in developed countries (4), but it remains a novel technology in developing countries, such as China. MT was not popularized for the management of pleural diseases until the 1980s, and even not available in some Chinese primary hospitals until now. Notably, over the past two decades, MT has been developed very rapidly in China, and has gradually become the first-choice for diagnosis pleural biopsy instead of video-assisted thoracoscopic surgery (VATS). Numbers of studies have all shown that compared with VATS, MT is highly sensitive and safe for diagnosing and treatment of pleural diseases, and also cost-effective. In this review, we analyze available studies on MT in China, and estimate the present status, the challenges, and future perspective of MT, with the goal of highlighting this procedure to more pulmonologists all around the country.
Medical thoracoscopy, the present status in China
Diagnostic and therapeutic utility in pleural diseases
Malignant pleural effusion (MPE)
Malignant pleural effusion is defined as the cytology or pleural biopsy specimen revealed underlying malignancy. As regards MPE, MT is often recommended when both pleural fluid cytology and closed pleural biopsy fail to yield a diagnosis (5).
Numerous series in China have reported that MT is a sensitive and safe procedure for diagnosing MPE, however, none of the studies is prospective randomized trails. Generally, the diagnostic accuracy of MT is around 90% without serious complications, and the main benefits of MT in MPE are diagnosing pleural metastasis by guided biopsy under direct vision and providing large amounts of tissue to allow histologic confirmation (6,7).
Recently, Wang et al. analyzed the accuracy and outcome of MT in the diagnosis of 833 patients with pleural effusion, which is the largest series to date, and found that malignancies were the most common causes of undiagnosed PEs (8). There were totally 342 (41.1%) patients diagnosed as MPE after MT. The most frequent cause of malignant PE was lung cancer (67.8%), followed by secondary carcinoma (11.7%), mesothelioma (10.2%), and lymphoma (2.9%). However, it is notable that the original malignancies in 25 patients (7.3%) with malignant PE could not be identified.
Yang et al. analyzed endoscopic features of the pleura of pathologically determined MPE, and showed that multiple nodules, solitary nodule, pleural thickening and adhesions, ulcer or pleural congestion could be seen under thoracoscopy (6). Larger nodules, heterogeneous pleural thickening or congestion are more common in MPE than TPE, which could be looked as malignant signatures under MT (9).
Treatment for MPE is palliative and focuses on safe, efficacious, and cost-effective symptom relief. Treatment options include fluid drainage and pleurodesis via thoracostomy or with thoracoscopic assistance (10), and pleurodesis remains the best method to control reaccumulation of the pleural effusion (11). The use of MT talc poudrage has been shown a safe and effective method for the treatment of MPE (7,12), and superior to talc slurry via a normal chest drain in some studies (13). MT for the talc poudrage is advantageous in that it allows optimal preparation of the pleural surface and homogeneous pleurodesis under visual control, as well as the shorter duration of pleural effusion controlling and hospital stay (13).
Furthermore, Xia et al. performed a meta-analysis to evaluate the efficacy and safety of talc pleurodesis in the management of MPE (14). They showed the success rate of talc pleurodesis was significantly higher than that of control therapies (P=0.035) with similar adverse events, and thoracoscopic talc poudrage was more effective than bedside talc slurry (P=0.026). Hence, thoracoscopic talc poudrage pleurodesis should be performed in patients with MPE (14).
Tuberculous pleural effusion (TPE)
Tuberculous pleural effusion remains a frequent form of extrapulmonary tuberculosis, particularly among HIV-positive individuals (15,16). In addition, tuberculosis is the most common cause of exudative effusions in areas with a high prevalence of tuberculosis (2,16). Diagnosis of TPE depends on the demonstration of mycobacterium tuberculosis in the pleural fluid or pleura tissue, or demonstration of caseating granulomas in the pleura (15,17). However, differentiating TPE from the many other causes of lymphocytic pleural effusions is often challenging. Because the conventional methods, such as the direct examination of pleural fluid by Ziehl-Neelsen staining, culture of the pleural fluid, and blind pleural biopsy, are not always helpful, more invasive procedures like thoracoscopy or thoracotomy are needed to perform differential diagnosis.
So far there is still lack of prospective randomized study to value the feasibility and safety of MT in the diagnosis of TPE. Wang et al. retrospectively analyzed a total of 333 patients who were eventually confirmed to suffer from TPE via MT, which is the first study to validate the high diagnosis yield and safety of MT for the management of TPE (8). Under thoracoscopy, they observed pleural nodules in 69.4%, pleural adhesion in 66.7%, hyperemia in 60.7%, pleural plaques in 6.0%, ulcer in 1.5% of patients with tuberculous pleurisy. Pleural biopsy revealed the presence of mycobacterium tuberculosis in the pleura tissue or/and demonstration of caseating granulomas in the pleura in 330 (99.1%) patients (8).
Similarly, Jiang et al. described the view appearance of tuberculous lesions in pleura and investigated the role of visual diagnosis in TPE under MT. The visual diagnosis of TPE was made according to the 5 types, as follows: necrosis, diffuse military nodules, single or multiple pleural nodules, hyperemic, edematous and thickened pleura, and pleura adhesions (18). The authors reported their preliminary diagnosis of TPE with these visual findings before the histology results coming out, and revealed the diagnosis efficiency was up to 93.41%. Hence, they emphasized the experience of the medical thoracoscopists for the high efficiency of the visual diagnosis (19).
In addition, He et al. evaluated a diagnostic flow chart applying MT, adenosine deaminase (ADA) and T-SPOT.TB in order to accurate diagnosis of TPE at Shandong Provincial Chest Hospital. This perspective study showed that the sensitivity and specificity of the diagnosis flow chart were 96.4% and 96.3%, indicating the flow chart had high sensitivity and excellent specificity for diagnosing TPE (20).
There are also some studies investigated the roles of MT in the treatment of TPE. Although simple aspiration or chest tube drainage is still commonly applied for treatment of TPE, the introduction of MT has led to other choices for TPE treatment. Shu et al. showed that compared with conventional thoracentesis repeatedly, MT with closed thoracic drainage in the treatment of TPE not only reduced the days for controlling pleural fluid and temperature, but also resulted in less rate of pleural adhesion, encapsulated effusion and pleural thickening (21). In addition, both Shu’s (22) and Shan’s (23) studies revealed that MT combined with urokinase injection can control pleural effusion more satisfactory, with improved lung function, lessening pleural thickening and adhesion, as well as similar complications.
Recently, Yu et al. conducted a retrospective study and analyzed the safety and efficacy of MT combined with streptokinase, in the treatment of multiloculated and organized TPE, which was the largest series to date with a total of 430 cases with TPE (24). It was reported that MT was a safe and successful method in treating multiloculated and organized TPE, which showed significant efficacy in the two groups but free-flowing effusion (24).
Undiagnosed pleural effusion
Unexplained exudative pleural effusion after repeated thoracocentesis are frequent causes for referral for diagnostic evaluation. However, the differential diagnosis of pleural effusions sometimes represents a considerable challenge. Approximately 25–40% of the pleural effusions remain undiagnosed after thoracocentesis and/or closed pleural biopsies (2,25).
All the previous published data demonstrated MT appears to be an efficacious and safe procedure in the diagnosis of undiagnosed pleural effusions. Wang et al. reported a total of 868 patients with pleural effusion of unknown etiology to be applied with semi-rigid MT, the overall diagnostic efficiency of MT was 92.6%, and malignancies (41.1%) were the most common causes, followed by tuberculous PE (40.0%), bacterial infection (8.4%), chylothorax (1.4%), and other exudates (Table 1) (26). These results were consistent with Jiang’s published data in 2013, which was the largest series to date with a total of 2,380 patients (27). They found that the positive diagnostic rate of MT was as high as 96.8%, and only 76 patients remained undiagnosed after that (27).
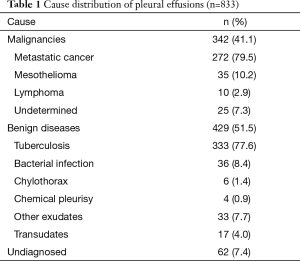
Full table
On the other hand, there were still some undiagnosed patients even after MT. So what should we do for these? Wang et al. recommended that a wait-and-see approach should be justified for the undiagnosed pleural effusions even after MT, unless repeated thoracentesis suggests a progressive pleural disease (26). Recently, the other retrospective case-note study evaluated the long-term outcome of patients with exudative effusions, which were performed with MT at least once. The results showed that the overall diagnostic value of the first and the second MT for MPE were 84.09% and 88.64%, respectively; for TPE were 86.36% and 100%, respectively. The authors addressed the value of long-term follow up for the “idiopathic pleuritis”, because the definitive diagnosis had been changed up to 68% of these patients during the follow-up period (28).
Pleural mesothelioma
The diagnosis of mesothelioma is not straightforward. The pleural fluid cytology is nonspecific, and only reliable in experienced centers. Most patients ultimately require invasive such as needle biopsy, or medical thoracoscopy to facilitate histological examination as gold standard for diagnosis (29). There were few studies performing the value of MT in pleural mesothelioma. Gao et al. reported that the diagnostic yield of MT was 100%, and patients were treated by pleurodesis under MT, so it can be used to diagnose and treat pleural mesothelioma at the same time (30). Jiang assessed the diagnostic value of MT in 52 cases of unknown origin pleural mesothelioma, compared with percutaneous needle biopsy of pleura. The results showed there was significant difference of the diagnostic rate between MT (100%) and needle biopsy (23.1%), so MT was an effective measure and should be the first choice in the diagnostic of pleural mesothelioma (31).
Chen et al. reported that 25 pleural mesothelioma patients (83.3%, 25/30) were diagnosed through medical thoracoscopy. Thoracic lesions manifested as nodules of diffuse distribution on the diaphragmatic pleura and parietal pleura. They emphasized that MT can make an early diagnosis and rigid thoracoscopy is recommended to perform to obtain adequate biopsies when thinking of malignant pleural mesothelioma (32).
Spontaneous pneumothorax
Spontaneous pneumothorax (SP) can be treated by various methods, ranging from observation or chest tube drainage to bullectomy or pleurectomy (33). MT has been gradually applied to treat patients with recurrent and primary SP. The advantage of MT is that it permits a minimally invasive, safe and effective procedure not only to treat the SP episodes but also to prevent recurrence. There is only one prospective randomized study to compare the difference between MT and simple chest tube drainage for the treatment of SP. It showed that MT treatment has shorter chest tube lengths (3.5 vs. 6.4 d) and lower recurrence (7% vs. 39%) when compared with tube drainage only (19). Some other retrospective studies also recommended procedure to obliterate pleural space by talc powder spray (18,34), chemical (silver nitrate) (18) or mechanical pleurodesis. The minor complications were transient fever and chest pain after talc powder spray (18).
Comparing diagnostic yield of medical thoracoscopy and pleural needle biopsy
Although MT has been shown to be highly successful in the diagnosis of pleural lesions, it remains an operative procedure requiring local anesthesia and hospital stay, and thus needs inherent cost for training and equipment (35). Closed pleural needle biopsy was still the first choice for pleural lesions by the current guideline (35), which including image-guided pleural biopsies and blind pleural biopsies. As a matter of fact, none of them has been used widely in many hospitals in China until now. The definitive diagnostic rate of pleural effusions had been very low before MT was introduced in China.
There were several studies compared the diagnostic yield of MT and closed pleural biopsy in pleural diseases, especially in TPE or MPE. Generally. MT remains superior to closed pleural biopsy in etiologic diagnosis of pleural effusion, with 88.9% (487/548) vs. 61.7% (171/277), which was the largest population study to date (36). The situation was similar in TPE with a lower rate (84% vs. 52%, P<0.05) (37). Importantly, there were more significant differences of positive diagnostic rate in malignant lesions between MT and blind pleural needle biopsy, especially for malignant mesothelioma (38). MT has the advantage of obtaining a greater amount of tissue, which may be relevant when the diagnosis is in doubt or when there is a need to obtain anti-TB drug sensitivity profiling. MT also allows the simultaneous opportunity to break down adhesions and drain the effusion in a controlled fashion (37,38).
Actually, it has been pointed out that in patients with only pleural fluid appearance on CT scan and in those who may have benign pleural pathologies other than TB, the primary method of diagnosis should be medical thoracoscopy (39). In future, prospective studies are needed to compare the sensitivity and the cost-effectiveness of these two methods in the setting of pleural malignancy and TB.
Comparing diagnostic yield of rigid thoracoscopy and semirigid thoracoscopy
MT can be performed using the rigid thoracoscopy or the semirigid thoracoscopy. A semirigid thoracoscopy combining the features of rigid thoracoscopy and flexible bronchoscopy has been available since its first report in 1998 (20). It was reported that the decisions to choose semirigid or rigid thoracoscopy depends on the extent of the adhesions found on imaging. Although the yield was similar wherever a biopsy could be performed with the semirigid device, it may be better to resort to the rigid instrument of adhesions presented or suspected (40). Contrary to the situation in developed countries, there is not any published prospective randomized trail comparing the two instruments, just only one retrospective study compared the diagnostic value between them in 98 patients with pleural effusion, and found rigid thoracoscopy has similar etiological diagnosis to semirigid thoracoscopy in undiagnosed pleural effusion (62.0% vs. 63.2%, P=0.927), but looks like better diagnostic value in MPE (87.8% vs. 100%, P=0.576) (41). Due to the small sample size, a larger study is required to define the usefulness of the two instruments and the choice of a particular thoracoscope in different subsets of subjects.
Comparing diagnostic yield of bronchoscope instead of medical thoracoscopy
In the earlier stage, some physicians have described the experiences of pleural biopsy using fiberoptic bronchoscopy as a flexible MT in the investigation of pleural disease. The unfamiliarity of the pulmonary physician with the rigid thoracoscope has led to this situation. Chen et al. explored the application of electronic bronchoscope replacing MT in 52 patients with undiagnosed pleural effusion, and reported that the diagnosis rate was 92.31% (48/52) with fewer complications (42). Similarly, Liu et al. evaluated the diagnostic value of electronic bronchoscope replacing MT in 133 patients, and reported the overall diagnostic rate was 86.4%. For MPE and TPE, the diagnostic efficiency of electronic bronchoscope was 98.4% and 80.3%, respectively (43).
At the same time, the problems of using fiberoptic bronchoscopy have already been described, the biopsies may be difficult to obtain and are sometimes inadequate to confirm a visual impression of malignancy (44). The results nowadays suggest that the fiberoptic bronchoscopy is less suitable and MT superior with larger biopsy specimens and better yield (44).
Complications of medical thoracoscopy
MT is a safe procedure when performed by a trained physician, which has been elucidated in almost all related clinical studies. Complications are few, with reported rates of between 0.4% and 44.1%. These include chest pain (24.9–44.1%), subcutaneous emphysema (8.0%), postoperative fever (5.3%), minor bleeding (4.6%), hypotension (0.5%), re-expansion pulmonary edema (0.5%) and empyema (0.4%) (Table 2) (26,45). In other reports, the overall complication rates for MT are 6.8–15.80% (46,47); however, most are minor and do not prolong hospital stay (26,45,46). There are not any reports of mortality rates with MT in published series in China to date.
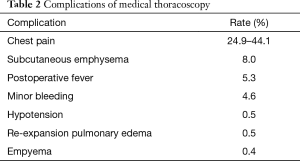
Full table
New challenges in medical thoracoscopy: fluorescence thoracoscopy
Conventional MT was performed with white light, and sometimes the endoscopic appearance of pleural diseases could be misleading. Recently, Wang et al. evaluated the diagnostic value of autofluorescence imaging during MT. The results showed autofluorescence was superior to white light, with a high sensitivity of 92.8% and negative predictive value of 76.8%, and was more useful to detect microlesions and delineate the pathologic margins (48,49).
Future perspectives of medical thoracoscopy
Despite medical thoracoscopy is gradually a standard procedure for diagnosis and treatment of pleural diseases in China nowadays, few randomized trials have been done to assess the diagnostic value and treatment superiorities compared with traditional methods or other subjects. Most of the results mentioned in this review are retrospective studies or observational series. More prospective, randomized clinical trials are therefore needed to define the diagnostic accuracy and safety of MT in pleural diseases in China.
It should be mentioned although MT has proven to be the most reliable diagnosis tool in the workup of patients with pleural diseases, with a definitive diagnosis in more than 95%. However, even after diagnostic MT, a clear diagnosis was not established in 62 (7.4%) patients, and the pleuritis was subsequently defined as “nonspecific” (26). Undoubtedly, the follow-up of nonspecific pleuritis is an important clinical problem, because several studies showed among these patients, 8.3–18% were eventually diagnosed with MPE, usually malignant pleural mesothelioma, during long-term follow-up (50,51). However, on which there was only one retrospective report has been published in China (28). Future research should target these areas of length and methods to determine the best follow-up protocols for these undiagnosed pleural effusion even after MT.
Autofluorescence has been used during MT, and received a higher sensitivity and negative predictive value for pleural diseases compared with white light. Nowadays, narrow band imaging (NBI) was applied to pleuroscopy for detecting malignant lesions by assessing vascular patterns of the pleura, and was found to be useful to detect irregular vascular patterns suggesting malignant lesions, especially for flat lesions (52). Further investigations are needed to determine the role of these new technologies available in clinical practice, which improves visualization of additional lesions under MT.
Conclusions
At present, MT has become a standard procedure instead of VATS to determine the aetiology of pleural effusion, with smaller wounds, less pain, less cost and shorter hospital stay (53). From the above studies we can definitely conduct that MT is widely used well in our country, not only in the diagnosis of undiagnosed exudative pleural effusions, but also in the management of pleural diseases, such as TPE, MPE and spontaneous pneumothorax. We believe that there will be more and more procedures being performed by MT, and MT training will be available in various levels of hospitals in China. It is noteworthy that few prospective clinical trials, lack of standard protocols or routine follow-up of MT are current problems for diagnosis and management in pleural effusion in China.
Meanwhile, we must keep in mind that MT remains an invasive procedure requiring training and careful patient selection. For example, MT should refer to procedures in patients who do not have pleural adhesion, because extensive adhesion will cause absent pleural spaces for MT. It is recommended routine ultrasound examination is performed prior to MT to evaluate the presence of a pleural space or not (53). However, what degree of adhesions is insufficient for MT? How do we deliver the best care for patients with pleural conditions, with selecting MT, VATS, or other pleural procedures? Future research should target these areas of variation to determine the best practice protocols of MT.
Acknowledgements
Funding: This work was supported in part by grants from National Natural Science Foundation of China (No. 81272591 and No. 81470274).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Maskell NA, Butland RJ, Pleural Diseases Group, et al. BTS guidelines for the investigation of a unilateral pleural effusion in adults. Thorax 2003;58 Suppl 2:ii8-17. [Crossref] [PubMed]
- Poe RH, Israel RH, Utell MJ, et al. Sensitivity, specificity, and predictive values of closed pleural biopsy. Arch Intern Med 1984;144:325-8. [Crossref] [PubMed]
- Rahman NM, Ali NJ, Brown G, et al. Local anaesthetic thoracoscopy: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii54-60. [Crossref] [PubMed]
- Oldenburg FA Jr, Newhouse MT. Thoracoscopy. A safe, accurate diagnostic procedure using the rigid thoracoscope and local anesthesia. Chest 1979;75:45-50. [Crossref] [PubMed]
- Light RW. Diagnostic principles in pleural disease. Eur Respir J 1997;10:476-81. [Crossref] [PubMed]
- Yang GY, Wang GL, Chen LZ, et al. Diagnostic value of Medical thoracoscopy in malignant pleural effusion. Journal of Clinical Pulmonary Medicine 2012;09:1650-1. [Article in Chinese].
- He WG, Zhao ZW, Zeng J, et al. Medical thoracoscopy in the diagnosis and treatment of malignant pleural effusion. Guangdong Medical Journal 2010;31:1844-6. [Article in Chinese].
- Wang Z, Xu LL, Wu YB, et al. Diagnostic value and safety of medical thoracoscopy in tuberculous pleural effusion. Respir Med 2015;109:1188-92. [Crossref] [PubMed]
- Xiao SH, Lin JS, Liu B, et al. Difference between tuberculosis pleurisy and malignant pleural tumor under thoracoscope. China Journal of Endoscopy 2011;17:1039-42. [Article in Chinese].
- West SD, Davies RJ, Lee YC. Pleurodesis for malignant pleural effusions: Current controversies and variations in practices. Curr Opin Pulm Med 2004;10:305-10. [Crossref] [PubMed]
- de Campos JR, Vargas FS, de Campos Werebe E, et al. Thoracoscopy talc poudrage: A 15-year experience. Chest 2001;119:801-6. [Crossref] [PubMed]
- Zhang W, Wang GF, Zhang H, et al. Medical thoracoscopic tale pleurodesis for malignant pleural effusion: an analysis of 27 cases. Beijing Da Xue Xue Bao 2008;40:600-2. [Article in Chinese]. [PubMed]
- Luo BQ, Xue KY, Wu XM, et al. Efficacy analysis of medical thoracoscopic pleurodesis in the treatment of patients with malignant pleural effusion. Journal of Clinical Pulmonary Medicine 2013;18:690-2. [Article in Chinese].
- Xia H, Wang XJ, Zhou Q, et al. Efficacy and safety of talc pleurodesis for malignant pleural effusion: A meta-analysis. PLoS One 2014;9:e87060. [Crossref] [PubMed]
- Gopi A, Madhavan SM, Sharma SK, et al. Diagnosis and treatment of tuberculous pleural effusion in 2006. Chest 2007;131:880-9. [Crossref] [PubMed]
- Light RW. Update on tuberculous pleural effusion. Respirology 2010;15:451-8. [Crossref] [PubMed]
- Diacon AH, Van de Wal BW, Wyser C, et al. Diagnostic tools in tuberculous pleurisy: A direct comparative study. Eur Respir J 2003;22:589-91. [Crossref] [PubMed]
- Jiang SJ, Shang JQ, Wang LS, et al. The diagnostic and therapeutic value of thoracoscopy in refractory or recurrent pneumothorax. Chinese Journal of Practical Internal Medicine 2002;22:427-8. [Article in Chinese].
- Li QM. Efficacy analysis of medical thoracoscopy in the treatment of recurrent pneumothorax. China Foreign Medical Treatment 2013;32:81-2. [Article in Chinese].
- He Y, Zhang W, Huang T, et al. Evaluation of a diagnostic flow chart applying medical thoracoscopy, adenosine deaminase and T-SPOT.TB in diagnosis of tuberculous pleural effusion. Eur Rev Med Pharmacol Sci 2015;19:3563-8. [PubMed]
- Liu H, Wei CZ, Lv J, et al. Medical thoracoscopy with closed thoracic drainage in the diagnosis and treatment of tuberculous pleural effusion. Journal of Minimally Invasive Medicine 2008;3:422-4. [Article in Chinese].
- Shu JK, Liu L, Zhang JQ, et al. Application of Medical Thoracoscopy in the Diagnosis and Treatment of Tuberculous Encysted Pleural Effusion. Journal of Kunming Medical University 2014;35:123.
- Shan WY, Tian L, Zhang GH, et al. Clinical research of medical thoracoscopy combined with urokinase injection in the Treatment of encapsulated tuberculous pleural effusion. Journal of Taishan Medical College 2015;36:615-7. [Article in Chinese].
- Xiong Y, Gao X, Zhu H, et al. Role of medical thoracoscopy in the treatment of tuberculous pleural effusion. J Thorac Dis 2016;8:52-60. [PubMed]
- Prakash UB, Reiman HM. Comparison of needle biopsy with cytologic analysis for the evaluation of pleural effusion: Analysis of 414 cases. Mayo Clin Proc 1985;60:158-64. [Crossref] [PubMed]
- Wang XJ, Yang Y, Wang Z, et al. Efficacy and safety of diagnostic thoracoscopy in undiagnosed pleural effusions. Respiration 2015;90:251-5. [Crossref] [PubMed]
- Jiang SJ, Mu XY, Zhang S, et al. The diagnostic value of medical thoracoscopy for unexplained pleural effusion. Zhonghua Jie He He Hu Xi Za Zhi 2013;36:337-40. [Article in Chinese]. [PubMed]
- Xu J, Liu CF, Han X, et al. The diagnostic value of medical thoracoscopy for pleural effusion with unknown origin and the clinical significance of follow-up. Zhonghua Jie He He Hu Xi Za Zhi 2014;37:64-6. [Article in Chinese].
- Husain AN, Colby TV, Ordonez NG, et al. Guidelines for pathologic diagnosis of malignant mesothelioma: A consensus statement from the international mesothelioma interest group. Arch Pathol Lab Med 2009;133:1317-31. [PubMed]
- Gao XL, Chen ZX, Guo JQ, et al. Medical thoracoscopy for diagnosis and treatment of pleural mesothelioma. China Journal of Endoscopy 2005;11:30-2. [Article in Chinese].
- Jiang SJ, Shang JQ, Su LL, et al. The diagnostic value of thoracoscopy in pleural mesothelioma. Tumor 2003;23:143-4. [Article in Chinese].
- Chen WH, Zhang XL, Dai HP, et al. Clinicopathological characteristics and prognosis of malignant pleural mesothelioma. Zhonghua Jie He He Hu Xi Za Zhi 2013;36:825-8. [Article in Chinese]. [PubMed]
- MacDuff A, Arnold A, Harvey J, et al. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-31. [Crossref] [PubMed]
- Kong H, Yang RA, Zhao S. Thoracoscope pleurodesis treat for recurrent pertinacious pneumatothorax. China Journal of Endoscopy 2002;8:21. [Article in Chinese].
- Hooper C, Lee YC, Maskell N, et al. Investigation of a unilateral pleural effusion in adults: British thoracic society pleural disease guideline 2010. Thorax 2010;65 Suppl 2:ii4-17. [Crossref] [PubMed]
- Xu Z, Lin KX, Yao W, et al. Diagnostic value of medical thoracoscopy for pleural effusion with unknown origin: report of 548 cases. Journal of Third Military Medical University 2014;36:2211-5. [Article in Chinese].
- Zhang CR, Lin JC, Zhou H, et al. Analysis of diagnostic value of thoracoscopy and closed pleural biopsy in tuberculous pleuritic. China Journal of Endoscopy 2008;14:837-9. [Article in Chinese].
- Han XM, Tao WH, Wang YL. Diagnostic value comparison of medical thoracoscope and closed pleural biopsy for pleural biopsy. Guangdong Yi Xue 2011;32:903-5. [Article in Chinese].
- Metintas M, Ak G, Dundar E, et al. Medical thoracoscopy vs. ct scan-guided abrams pleural needle biopsy for diagnosis of patients with pleural effusions: A randomized, controlled trial. Chest 2010;137:1362-8. [Crossref] [PubMed]
- Dhooria S, Singh N, Aggarwal AN, et al. A randomized trial comparing the diagnostic yield of rigid and semirigid thoracoscopy in undiagnosed pleural effusions. Respir care 2014;59:756-64. [Crossref] [PubMed]
- Liang Y, Shen N, Zhu H, et al. Diagnostic value of rigid and semirigid thoracoscopy in undiagnosed pleural effusion. Chinese Journal of Minimally Invasive Surgery 2015;15:9-12. [Article in Chinese].
- Chen YH, Zheng LX, Luo W, et al. Application of electronic bronchoscope replacing medical thoracoscopy in diagnosis of undiagnosed pleural effusion. International Journal of Respiration 2013;33:603-4. [Article in Chinese].
- Liu ZG, Wu HQ, Zhang WD, et al. The application of electronic bronchoscope replacing thoracoscope to diagnose unclear causes of pleural effusion. China Journal of Endoscopy 2012;18:85-8. [Article in Chinese].
- Robinson GR 2nd, Gleeson K. Diagnostic flexible fiberoptic pleuroscopy in suspected malignant pleural effusions. Chest 1995;107:424-9. [Crossref] [PubMed]
- Li YP, Peng QZ, Zhong MH, et al. Adverse reactions of thoracoscopy in the diagnosis and treatment of pleural effusion and its prevention (with an analysis of 589 cases). [Article in Chinese] Journal of Clinical Pulmonary Medicine 2015;20:1536-7.40.
- Zhang TM, Huang ZF, Li CL, et al. Adverse reactions of medical thoracoscopy in the diagnosis and treatment of tuberculous pleuris. Journal of Guiyang Medical College 2013;38:169-70. [Article in Chinese].
- Ou QF, Chen HX, Gao L, et al. Adverse events of medical thoracoscopy: an analysis of 216 cases. The Journal of Practical Medicine 2015;31:1382-3. [Article in Chinese].
- Wang F, Wang Z, Tong Z, et al. A pilot study of autofluorescence in the diagnosis of pleural disease. Chest 2015;147:1395-400. [Crossref] [PubMed]
- Wang F, Tong Z. The progress of study and application in Medical Thoracoscopy. Zhonghua Jie He He Hu Xi Za Zhi 2015;38:128-30. [Article in Chinese]. [PubMed]
- Davies HE, Nicholson JE, Rahman NM, et al. Outcome of patients with nonspecific pleuritis/fibrosis on thoracoscopic pleural biopsies. Eur J Cardiothorac Surg 2010;38:472-7. [Crossref] [PubMed]
- Metintas M, Ak G, Cadirci O, et al. Outcome of patients diagnosed with fibrinous pleuritis after medical thoracoscopy. Respir Med 2012;106:1177-83. [Crossref] [PubMed]
- Ishida A, Ishikawa F, Nakamura M, et al. Narrow band imaging applied to pleuroscopy for the assessment of vascular patterns of the pleura. Respiration 2009;78:432-9. [Crossref] [PubMed]
- Medford AR, Bennett JA, Free CM, et al. Current status of medical pleuroscopy. Clin Chest Med 2010;31:165-72. [Crossref] [PubMed]


