
Surgical correction of a previously operated juvenile idiopathic scoliosis with crankshaft phenomenon: an illustrative case report
Introduction
Crankshaft phenomenon after posterior fusion for scoliosis is a well-known entity that has been initially described by Dubousset in 1973 (1) where he noticed progression of scoliotic deformity in the setting of stable posterior spinal fusion in younger patients with paralytic scoliosis. It was named so because it appeared that the spine gradually rotated along the length of the fusion because of the continued anterior spinal growth. It was later on also described after the use of Harrington rods (2) and in posteriorly fused congenital and idiopathic scoliosis patients (3).
Crankshaft is defined as an increase in the Cobb angle >10°, or the Mehta angle RVAD (rib-vertebra angle difference) >10°, or any decrease in the apex-rib thoracic distance, or increase in the vertebral apical lumbar translation (4,5). Risks factors include immaturity consisting of patients classified in Risser 0 to 2 and particularly in those with open triradiate cartilage of the acetabulum and large residual deformity (6).
Incidence of crankshaft phenomenon decreased during the past decades because of better indications in young patients (avoiding fusion in the immature spine with open triradiate cartilage, using conservative treatment such as brace until the final fusion age is reached, performing surgery with the use of growth-friendly systems such as growing rods or more recently vertebral body tethering) and also since the advent of pedicle screws that can help maintain a deformity correction by traversing all 3 columns and stopping simultaneously the posterior but also the anterior spinal growth. However, in some cases, if the patient is still immature and the pedicle screws are not properly reaching the vertebral body anteriorly, crankshaft phenomenon may occur.
The case of a young female adolescent is presented; she has been complaining of chronic thoracic deformity with unleveled shoulders and coronal imbalance 3 years after she underwent corrective surgery for scoliosis. Surgical management and its steps are thoroughly illustrated which has not been seen before in the literature. We present the following case in accordance with the CARE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-31/rc).
Case presentation
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parents or legal guardians for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
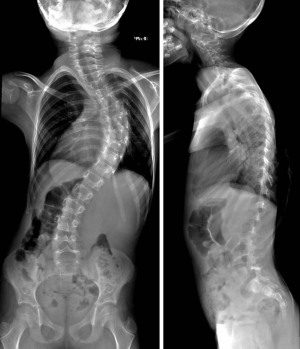
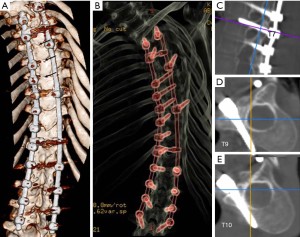
An 11-year-old girl has been complaining of a progressively increasing hump in her back with waists and shoulders asymmetry during the past 6 months. Three years prior to presentation, at the age of 8, she underwent in another institution posterior correction and fusion from T3 to L3 for a right thoracic juvenile idiopathic scoliosis with a Cobb angle of 60° (Figure 1). After the initial correction to 30° (Figure 2), follow-up X-rays revealed a progressive increase of the scoliosis angulation with the onset of a coronal malalignment mainly at the cervicothoracic junction. Physical exam at the time of presentation revealed a prominent shoulder blade on the right side, with waists asymmetry, unleveled shoulders, and head shift toward the left side (Figure 3) but a completely normal neurological assessment. Full spine anteroposterior X-ray revealed a long right thoracolumbar scoliosis of 70° with the proximal screw pulled out from the rod on the right side and an increased rotation at the apical levels as demonstrated by the screws’ direction to the right side, RVAD was 27° (Figure 4). Lateral view showed an acceptable sagittal alignment with normal sagittal vertical axis and pelvic tilt, however the thoracic pedicle screws above T8 seemed to have an unusual upward direction, in addition, the rods that were previously in kyphosis seem to be rather flat (Figure 4). CT scan with 3D reconstruction confirmed posterior fusion between the apical vertebras (Figure 5A) with many thoracic pedicle screws that either presented an ascending direction (above T8, Figure 5B,5C) or were divergent not reaching the vertebral body anteriorly (below T8, Figure 5D,5E). MRI ruled out any congenital anomaly.


Considering the nature of the deformity, the fact that it has been steadily worsening with the diagnosis of crankshaft phenomenon after scoliosis surgery, and also the fact that the triradiate cartilage was closed, the patient was managed surgically through a posterior-only approach with implants removal, correction of the pedicle screws trajectories, posterior column osteotomies at the apical levels and instrumentation from T1 to L4 (from the most tilted vertebra above the construct, to the lowest stable vertebra in relation to the center sacral vertical line below the construct).
The patient was installed in a prone position, on 4 cushions. Multimodal intraoperatively neuromonitoring was used during the whole procedure.
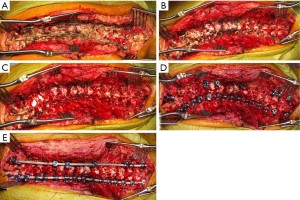
The operative field was exposed from T1 to L4; a posterior cutaneous midline incision was made over the previous scar. The spine was exposed subperiosteally, going laterally to the transverse processes. Previous implants were identified (4.5 mm rod), with important scar tissues and posterior fusion could be seen at the apical thoracic levels (Figure 6A). The rods and screws were all removed (Figure 6B) and resection of the inferior articular processes at all levels was performed bilaterally to provide maximum flexibility to the spine. In addition, posterior column osteotomies were performed at 6 levels between T4 and T10 in order to completely release the posterior fusion (Figure 6C). The free-hand technique for pedicle screws placement from T1 to L4 was then applied (consecutive on the left and skipped on the right, Figure 6D), entry point and direction of the screws were rectified in order to have a sufficient grip inside the vertebral bodies. In order to correct the deformity, cantilevering of the spine with 1 prebended 5.5 mm cobalt-chrome rod on the left concave side was first performed, completed by other correction techniques including compression, distraction and in situ bending. The rod was completely secured and a contralateral rod was then placed and secured to complete the construct (Figure 6E). After freshening of the bony bed, autologous grafts were inserted to cover the maximum surface. Operative time was 270 minutes, total blood loss was 1,000 mL.
The patient could walk on day 1 with assistance from a physical therapist and no orthosis. She was discharged on day 7.
Postoperative 3D reconstructed CT scan confirmed satisfactory screws position and coronal correction of the deformity (Figure 7). Significant improvement of the gibbosity and the shoulders and waists symmetry could be noticed during the 9 months follow-up visit (Figure 8).


The regular postoperative X-rays showed a maintained correction of the scoliosis with angulation of 11° and a satisfactory sagittal alignment (Figure 9). The patient showed a continued satisfactory clinical and radiological results at 3 years.

Discussion
In the skeletally immature patient (open triradiate cartilage and Risser 0), the crankshaft phenomenon is thought to occur secondary to continued growth of the anterior elements of the spine after solid posterior spinal fusion, and it leads to progressive deformity in three planes, sagittal, coronal and axial (7). However, it was demonstrated, through a histologic evaluation of the Risser grade, that considerable residual growth activity can occur in patients up to Risser Grade 4, therefore longitudinal spinal growth alone may not be the only cause of crankshaft phenomenon (8).
Our patient was previously operated with open triradiate cartilage, and the continued anterior growth with an increasing deformity in 3 dimensions could be clearly seen on the X-rays with: increase of the Cobb angle to a higher degree than the preoperative one and proximal screw pull-out on the convex right side (convex lengthening) in the coronal plane, flattening of the rods in the sagittal plane, and increased rotation at the apical levels as demonstrated by the screws direction to the right side in the axial plane.
Literature shows rates between 5% and 97% in the development of crankshaft phenomenon after instrumented posterior arthrodesis in such immature population (9-11). In a retrospective study by Kesling (4), crankshafting was seen in 15% of the 54 patients (children before the pubertal growth spurt) that underwent posterior spinal arthrodesis for congenital scoliosis, and there was a positive correlation with earlier surgery and larger (>50°) curves. In another study by Roberto (12), 28% of the 86 immature patients (Risser 0 or 1) who underwent posterior spinal fusion for idiopathic scoliosis showed curve progression of more than 10° after surgery (mainly patients with open triradiate cartilage).
In order to detect the occurrence of crankshaft, Sanders (13) assessed changes in Cobb measurements, rib vertebral angle difference changes, and rotational changes. He found that the changes in the rib vertebral angle difference, rather than a change in Cobb angles, were the most sensitive method in assessing crankshaft phenomenon. In fact, it was demonstrated that an increase in Cobb angle measurements is not a reliable indicator of a crankshaft effect (14). Our patient showed significant values for both parameters which helped confirming the crankshaft diagnosis.
Crankshaft phenomenon may be prevented by combining anterior and posterior fusion in immature patients (5,15,16). But after the advent of pedicle screws, several studies demonstrated that the use of segmental pedicle screw instrumentation traversing the 3 columns of the spine and making it stiff, can help in maintaining correction in skeletally immature patients during their growth precluding the need for a complementary anterior fusion (17-19). They demonstrated that in patients with open triradiate cartilage, hybrid instrumentation cannot successfully avoid the occurrence of a crankshaft phenomenon postoperatively, whereas consecutive or interval pedicle screw construct is more efficient in this manner (19). Also, an experimental study on immature canine models showed that the use of a posterior intrapedicular spinal construct proved sufficient to overcome the anterior growth centers preventing lordosis from occurring, thus thwarting the essential processes responsible for the development and worsening of deformity without a complementary anterior surgical approach (20).
However, another study showed that posterior spinal fusion alone with pedicle screws could not completely control all 3 columns of the spine during growth and was associated with curve progression in a significantly greater proportion of patients with open triradiate cartilage compared with anterior-posterior spinal fusion (21). Also, a study by Papin (22) showed that although a significant 3D correction can be obtained after posterior instrumentation and fusion in AIS, a significant loss of correction and an increase in spinal length occur in the years following surgery, suggesting that a Crankshaft phenomenon may be an important factor altering the long-term 3D correction after posterior instrumentation of the spine for idiopathic scoliosis.
In the case of our patient, multiple factors could be identified for the occurrence of the crankshaft phenomenon: immature age below 10-year, Risser 0, open triradiate cartilage, and pedicle screws not properly reaching the vertebral body especially at the apex of the deformity leading to a posterior fusion while the anterior growth remained.
Crankshaft phenomenon often requires revision surgery. In a series of 638 pediatric spinal deformity patients (23), 50 cases required revision surgeries for decompensation, pseudarthrosis and crankshaft phenomenon (8 patients), which consisted of posterior column osteotomies and combined anterior-posterior fusion. But despite the latter surgical strategy being a viable option, our patient could be correctly managed with a posterior-only approach without the necessity of opening the thorax or abdomen.
Literature has been globally scarce about crankshaft phenomenon during the past 2 decades, being cited in only 54 articles with few discussing its proper treatment and no illustrative case reports, and this condition remains challenging when it comes to its surgical management. The current report illustrated the management of such rare spinal deformity surgery complication. Despite previous posterior surgery with fusion at the surgical site, revision through the same posterior approach with the use of multiple posterior column osteotomies could address the deformity without the need for an anterior approach or a more aggressive correction technique and with satisfactory long-term results.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-31/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-31/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parents or legal guardians for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dubousset J. Récidive d'une scoliose lombaire et d'un bassin oblique après fusion précoce: le phénomène du villebrequin. Proceedings of Groupe d'Etude de la Scoliose, Paris, France 1973:62-7.
- Lee CS, Nachemson AL. The crankshaft phenomenon after posterior Harrington fusion in skeletally immature patients with thoracic or thoracolumbar idiopathic scoliosis followed to maturity. Spine (Phila Pa 1976) 1997;22:58-67. [Crossref] [PubMed]
- Murphy RF, Mooney JF 3rd. The Crankshaft Phenomenon. J Am Acad Orthop Surg 2017;25:e185-93. [Crossref] [PubMed]
- Kesling KL, Lonstein JE, Denis F, et al. The crankshaft phenomenon after posterior spinal arthrodesis for congenital scoliosis: a review of 54 patients. Spine (Phila Pa 1976) 2003;28:267-71. [Crossref] [PubMed]
- Pizones J, Alvarez-González P, Sánchez-Mariscal F, et al. Prognostic factors of the crankshaft phenomenon in patients with scoliosis and open triradiate cartilage. Is the double approach the solution? Rev Esp Cir Ortop Traumatol 2013;57:170-7. [Crossref] [PubMed]
- Shufflebarger HL, Clark CE. Prevention of the crankshaft phenomenon. Spine (Phila Pa 1976) 1991;16:S409-11. [Crossref] [PubMed]
- Sanders JO, Little DG, Richards BS. Prediction of the crankshaft phenomenon by peak height velocity. Spine (Phila Pa 1976) 1997;22:1352-6; discussion 1356-7. [Crossref] [PubMed]
- Noordeen MH, Haddad FS, Edgar MA, et al. Spinal growth and a histologic evaluation of the Risser grade in idiopathic scoliosis. Spine (Phila Pa 1976) 1999;24:535-8. [Crossref] [PubMed]
- Dubousset J, Herring JA, Shufflebarger H. The crankshaft phenomenon. J Pediatr Orthop 1989;9:541-50. [Crossref] [PubMed]
- Sponseller PD, Betz R, Newton PO, et al. Differences in curve behavior after fusion in adolescent idiopathic scoliosis patients with open triradiate cartilages. Spine (Phila Pa 1976) 2009;34:827-31. [Crossref] [PubMed]
- Hamill CL, Bridwell KH, Lenke LG, et al. Posterior arthrodesis in the skeletally immature patient. Assessing the risk for crankshaft: is an open triradiate cartilage the answer? Spine (Phila Pa 1976) 1997;22:1343-51. [Crossref] [PubMed]
- Roberto RF, Lonstein JE, Winter RB, et al. Curve progression in Risser stage 0 or 1 patients after posterior spinal fusion for idiopathic scoliosis. J Pediatr Orthop 1997;17:718-25. [Crossref] [PubMed]
- Sanders JO, Herring JA, Browne RH. Posterior arthrodesis and instrumentation in the immature (Risser-grade-0) spine in idiopathic scoliosis. J Bone Joint Surg Am 1995;77:39-45. [Crossref] [PubMed]
- Delorme S, Labelle H, Aubin CE. Is Cobb angle progression a good indicator in adolescent idiopathic scoliosis? Spine (Phila Pa 1976) 2002;27:E145-51. [Crossref] [PubMed]
- Dohin B, Dubousset JF. Prevention of the crankshaft phenomenon with anterior spinal epiphysiodesis in surgical treatment of severe scoliosis of the younger patient. Eur Spine J 1994;3:165-8. [Crossref] [PubMed]
- Lapinksy AS, Richards BS. Preventing the crankshaft phenomenon by combining anterior fusion with posterior instrumentation. Does it work? Spine (Phila Pa 1976) 1995;20:1392-8. [Crossref] [PubMed]
- Burton DC, Asher MA, Lai SM. Scoliosis correction maintenance in skeletally immature patients with idiopathic scoliosis. Is anterior fusion really necessary? Spine (Phila Pa 1976) 2000;25:61-8. [Crossref] [PubMed]
- Sarlak AY, Atmaca H, Buluç L, et al. Juvenile idiopathic scoliosis treated with posterior arthrodesis and segmental pedicle screw instrumentation before the age of 9 years: a 5-year follow-up. Scoliosis 2009;4:1. [Crossref] [PubMed]
- Tao F, Zhao Y, Wu Y, et al. The effect of differing spinal fusion instrumentation on the occurrence of postoperative crankshaft phenomenon in adolescent idiopathic scoliosis. J Spinal Disord Tech 2010;23:e75-80. [Crossref] [PubMed]
- Kioschos HC, Asher MA, Lark RG, et al. Overpowering the crankshaft mechanism. The effect of posterior spinal fusion with and without stiff transpedicular fixation on anterior spinal column growth in immature canines. Spine (Phila Pa 1976) 1996;21:1168-73. [Crossref] [PubMed]
- Sponseller PD, Jain A, Newton PO, et al. Posterior Spinal Fusion With Pedicle Screws in Patients With Idiopathic Scoliosis and Open Triradiate Cartilage: Does Deformity Progression Occur? J Pediatr Orthop 2016;36:695-700. [Crossref] [PubMed]
- Papin P, Labelle H, Delorme S, et al. Long-term three-dimensional changes of the spine after posterior spinal instrumentation and fusion in adolescent idiopathic scoliosis. Eur Spine J 1999;8:16-21. [Crossref] [PubMed]
- Yagi M, King AB, Kim HJ, et al. Outcome of Revision Surgery in Pediatric Spine Deformity Patients. Spine Deform 2013;1:59-67. [Crossref] [PubMed]



