Factors influencing the decision to pursue immediate breast reconstruction after mastectomy for breast cancer
Introduction
Breast cancer is the most common cancer in women and the second most common cancer worldwide. In 2013 approximately 14,000 patients in the Netherlands were diagnosed with breast cancer, which is almost 30% of all cancer patients in the Netherlands (1). The cornerstone of breast cancer treatment is surgery in which mastectomy is still required, or the patients preferred option, in one third of all breast cancer patients (2,3). Breast reconstruction can be performed at the time of mastectomy, immediate breast reconstruction (IBR) using autologous tissue or implants (4). The cosmetic outcome of IBR is superior to mastectomy (5). Literature has proven good psychosocial outcome and quality of life in patients who underwent IBR (2,4,6,7). A study conducted by Al-Ghazal et al. showed that patients who underwent IBR showed less psychological distress than patients who underwent delayed breast reconstruction (8). Furthermore, studies have shown that IBR is oncologically safe as local recurrence incidence following IBR is comparable to that after mastectomy (5,9-14). This led to increasing IBR in the United States. In 2000, 12.9% of all mastectomies performed in the United States were combined IBR, increasing to 36.3% in 2009 (15). The United Kingdom Association of Breast Surgery recommends that any patient in which IBR is oncologically safe should have the possibility to choose for IBR (16). Dutch guidelines state IBR has a slight preference instead of delayed reconstruction and that every patient considered for mastectomy has to be informed about reconstructive options (17). However, despite the evidence and recommendations, almost two thirds of the mastectomies are still performed without IBR. We asked ourselves if there are elements in the pre-operative process that could facilitate or impede the choice for IBR. The major objective of this study was to investigate the decision-making process on whether or not a patient undergoes immediate reconstruction after mastectomy. In this study we focused on the role of patient as well as the role of the breast surgeon.
Methods
We investigated all electronic patient files of women diagnosed with DCIS or invasive carcinoma between 2010 and 2013, and underwent a mastectomy at the Canisius Wilhelmina Breast Center in Nijmegen, the Netherlands. Patients who underwent prophylactic mastectomy were excluded. IBR is defined as mastectomy and reconstruction performed on the same day. Surgeons who saw the patients were dedicated breast surgeons and plastic surgeons.
The following patient variables were scrutinized: age, diabetes, family breast cancer history, smoking habits, body mass index (BMI). We considered a BMI as normal as it was <25 kg/m2. Overweight was defined as a BMI between 25 and 30 kg/m2, and obesity was defined as a BMI equal or more than 30 kg/m2.
Our primary outcome measure was whether or not a patient received information about the decision making process regarding immediate reconstruction during mastectomy. We searched for any documentation in the electronic patient file of patients who did not undergo IBR about the reason for refraining from this procedure. Medical issues detected by the doctors were noted as well as personal restraints from patients. Patients were contacted by telephone when written documentation about IBR was poor or equivocal.
All data management and analysis were performed using SPSS 20.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were presented in numbers and percentages. The chi-square test was used to compare percentages between two groups (IBR and no IBR). Continuous variables, such as age and BMI, were presented as means. Groups were compared by performing the independent-samples t-test. In order to evaluate independent predictors for IBR, variables with a P value below 0.05 were further tested with a logistic regression. A P value <0.05 was considered as significant.
Results
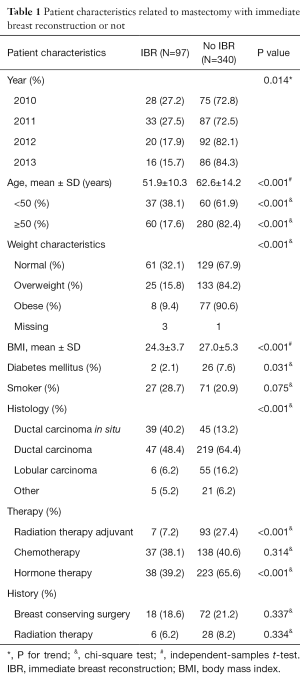
Out of 437 mastectomies, IBR was performed in 97 patients (22%). Patient characteristics are summarized in Table 1. The majority of IBR were tissue expanders (88; 89.8%), followed by deep inferior epigastric perforator free flap (5; 5.1%) and primary implants (4; 4.1%). Between 2010 and 2013, the incidence of IBR was declining (P=0.014).
Full table
Factors associated with reduced use of IBR were increasing age (P<0.001) and weight (P<0.001), diabetes mellitus (P=0.031) and adjuvant radiation therapy (P<0.001). Logistic regression analysis showed age above 50 years (OR =0.299; 95% CI: 0.171–0.520, P=0.000), overweight (OR =0.499; 95% CI: 0.286–0.868, P=0.014) and being obese (OR =0.294; 95% CI: 0.129–0.670, P=0.004), and adjuvant radiation therapy (OR =0.165; 95% CI: 0.070–0.385, P=0.000) to be independent predictors for the decision not to perform IBR. Diabetes mellitus and smoking had no influence on the decision to perform IBR.
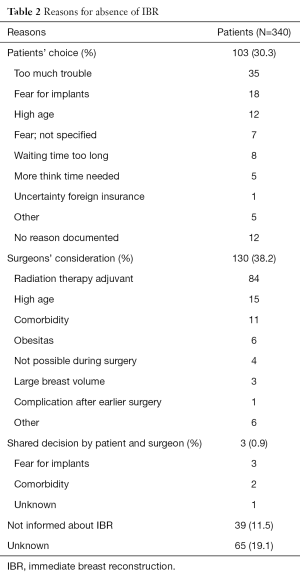
In 215 of 340 patients who did not undergo IBR, reasons for refraining from IBR were insufficiently documented and where therefore contacted by telephone. In 126 cases, the breast surgeon decided not to perform IBR, with adjuvant radiation therapy as main reason (Table 2). In these 84 patients, 61 patients received adjuvant radiation therapy. Almost one third of all patients had decided not to undergo IBR, mainly because they thought it would be too much trouble. Forty two patients visited the plastic surgeon after which 38 patients refused IBR, mainly because they thought it would be too much trouble or waiting time would be too long. In four cases the plastic surgeon decided not to perform IBR because it was not possible during surgery. Thirty nine patients were not informed about IBR and 7 of these patients did regret not being informed. In 65 cases, no information from patients was available since patients were deceased, did not answer the phone or could not remember the conversation with the breast surgeon.
Full table
Discussion
Exploring reasons for not performing IBR, we found poor documentation regarding considerations whether or not to perform IBR in 50% of the mastectomy cases. After calling these patients, we found that almost 10% of all patients were not informed about IBR. In the cases where therapeutic considerations were documented, 38.2% of patients who did not undergo IBR, breast surgeons decided not to offer IBR to the patient. The most common reason for declining IBR was the anticipated need for postoperative radiation therapy. However, almost 30% of these patients eventually did not receive radiation therapy after mastectomy. Multiple studies and reviews showed that post-mastectomy radiation therapy is associated with a higher incidence of complications and implant loss (18-22). Furthermore, literature states that radiation therapy has a negative impact on cosmetic outcome, due to often severe capsular contracture after implant-based reconstruction (21-25). As a result, reconstructed patients with radiation therapy had significantly lower satisfaction with outcome (21,26), psychosocial well-being, sexual well-being and physical well-being (26). On individual basis, however, breast surgeon, plastic surgeon and patient can through a process of proper informed shared decision making, opt for IBR, although the indication for postoperative radiation therapy is present.
In this study we found that IBR tends to be proposed less often to patients with advancing age and higher BMI. These factors, as well as type II diabetes and radiation therapy, are used by the surgical team to assess whether the patient is deemed fit for reconstruction. However, studies show IBR is a safe option in the elderly and age per se should not be a contraindication (27,28). Veronesi et al. showed that IBR is feasible and safe in elderly patients if the overall status of the patient is taken into consideration and pre-existing medical conditions are optimized (18). IBR was also less frequently offered to overweight and obese patients, which is in accordance with other studies. Being overweight or obese is associated with higher complication rate after IBR (23,29-34). Diabetes mellitus and smoking habits were not found to influence the decision to propose IBR. However, diabetes mellitus has shown to be a risk factor for surgical site infections (35) and skin necrosis (33,34) after breast surgery and is associated with poorer outcome after IBR (36). Studies show that smoking habits are associated with higher incidence of skin necrosis (33,34) and surgical site infections (37).
From the reasons why patients themselves, or their family, decline IBR, fear for complications or the difficulty to oversee the impact are often heard. In these cases, proper information will have been discussed, nevertheless, reassurance should be given. Especially since patients underestimate their quality of life and overestimate complication rates after IBR (38,39). These issues should be discussed with patients during the preoperative decision making process. On the other hand it is important to realize not every woman wants nor needs a reconstruction, whether immediate or delayed. We should refrain from talking patients into an unwanted reconstruction and value a proper shared decision making process. As a consequence, it is important to gain insight in what percentage of patients, wanting a reconstruction, really appreciate IBR, to be able to benchmark the IBR rate.
In contrast to mastectomy, IBR has been shown to provide better cosmetic outcome and superior quality of life, without compromising oncological safety (2-7,9-13,40-44). Although literature states that women benefit from IBR, in the past 3 years, 16% (range, 0–63%) of the patients with invasive breast cancer and 41% (range, 0–83%) of the patients with ductal carcinoma in situ underwent IBR in the Netherlands (1). We found a decreasing IBR trend over time in the 22.2% of breast cancer patients who underwent IBR. In the context of the multidisciplinary board, less patients were considered for reconstruction. Increasing indications for post mastectomy radiation treatment, lead to a more cautious policy of advising IBR. Moreover, plastic surgeons and patients alike increasingly prefer the superior cosmetic results of autologous reconstructions with DIEP. The downside of which is the long operation time, which can be difficult to reconcile with the expedited planning in case of malignancy.
Since this study was performed retrospectively, the lack of documentation in the records leaves us with often scarce explanation concerning the decision for or against IBR. We therefore had to contact patients by telephone to document reasons for refraining from IBR. In 65 patients no information was available whether or not IBR was discussed. Thirty nine patients were not properly informed about the (im)possibilities, 20% of these patients reported to regret this. It cannot be ruled out that closer attention to documenting whether IBR has been considered in the first place, could raise the rate of IBR offered to patients. Breast surgeons thus are more consciously involved in producing a well-founded shared decision vis-à-vis the patient confronted with the mastectomy. Potential risk factors for complications in IBR can be balanced against (ir)realistic expectations and fears of the patient.
Strengths of this study are the reflection of a real life situation, over a fairly large, non-selected population from a teaching breast center. Reviewing the files revealed the lack of documentation as a potential reason for the low reconstruction rate, which could not have been possible in a prospective fashion.
In conclusion, factors that appear to influence the breast surgeons’ decision to refrain from IBR are anticipated radiotherapy, high age and BMI. In half of breast cancer patients who did not undergo IBR, documentation about considerations regarding IBR was missing, suggesting a high proportion of patients might not be properly informed. Patients declined IBR mainly because of fear for implants and operation related trouble. In almost 10% of all patients IBR was not discussed. In all patients in whom a mastectomy is planned, IBR should be discussed and documented.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was not required. Patient data was retrieved from hospital medical record system, therefore informed consent was not required. Patient’s personal data have been secured. The study outcomes could affect future management of patients.
References
- Integraal Kankercentrum Nederland. Netherlands Comprehensive Cancer Organisation. Available online: https://www.iknl.nl/over-iknl/about-iknl
- Heneghan HM, Prichard RS, Lyons R, et al. Quality of life after immediate breast reconstruction and skin-sparing mastectomy - a comparison with patients undergoing breast conserving surgery. Eur J Surg Oncol 2011;37:937-43. [Crossref] [PubMed]
- Patani N, Devalia H, Anderson A, et al. Oncological safety and patient satisfaction with skin-sparing mastectomy and immediate breast reconstruction. Surg Oncol 2008;17:97-105. [Crossref] [PubMed]
- Robertson S, Wengström Y, Eriksen C, et al. Breast surgeons performing immediate breast reconstruction with implants - assessment of resource-use and patient-reported outcome measures. Breast 2012;21:590-6. [Crossref] [PubMed]
- Agrawal A, Grewal M, Sibbering DM, et al. Surgical and oncological outcome after skin-sparing mastectomy and immediate breast reconstruction. Clin Breast Cancer 2013;13:478-81. [Crossref] [PubMed]
- Drucker-Zertuche M, Robles-Vidal C. A. 7 year experience with immediate breast reconstruction after skin sparing mastectomy for cancer. Eur J Surg Oncol 2007;33:140-6. [Crossref] [PubMed]
- Begum S, Grunfeld EA, Ho-Asjoe M, et al. An exploration of patient decision-making for autologous breast reconstructive surgery following a mastectomy. Patient Educ Couns 2011;84:105-10. [Crossref] [PubMed]
- Al-Ghazal SK, Sully L, Fallowfield L, et al. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol 2000;26:17-9. [Crossref] [PubMed]
- Agrawal A, Sibbering DM, Courtney CA. Skin sparing mastectomy and immediate breast reconstruction: a review. Eur J Surg Oncol 2013;39:320-8. [Crossref] [PubMed]
- Romics L Jr, Chew BK, Weiler-Mithoff E, et al. Ten-year follow-up of skin-sparing mastectomy followed by immediate breast reconstruction. Br J Surg 2012;99:799-806. [Crossref] [PubMed]
- Nedumpara T, Jonker L, Williams MR. Impact of immediate breast reconstruction on breast cancer recurrence and survival. Breast 2011;20:437-43. [Crossref] [PubMed]
- van Mierlo DR, Lopez Penha TR, Schipper RJ, et al. No increase of local recurrence rate in breast cancer patients treated with skin-sparing mastectomy followed by immediate breast reconstruction. Breast 2013;22:1166-70. [Crossref] [PubMed]
- Gieni M, Avram R, Dickson L, et al. Local breast cancer recurrence after mastectomy and immediate breast reconstruction for invasive cancer: a meta-analysis. Breast 2012;21:230-6. [Crossref] [PubMed]
- Eriksen C, Frisell J, Wickman M, et al. Immediate reconstruction with implants in women with invasive breast cancer does not affect oncological safety in a matched cohort study. Breast Cancer Res Treat 2011;127:439-46. [Crossref] [PubMed]
- Yang RL, Newman AS, Lin IC, et al. Trends in immediate breast reconstruction across insurance groups after enactment of breast cancer legislation. Cancer 2013;119:2462-8. [Crossref] [PubMed]
- Association of Breast Surgery at Baso. Surgical guidelines for the management of breast cancer. Eur J Surg Oncol 2009;35 Suppl 1:1-22. [Crossref] [PubMed]
- Association of Comprehensive Cancer Centres. Oncoline 2016. Available online: http://oncoline.nl/index.php
- Veronesi P, Ballardini B, De Lorenzi F, et al. Immediate breast reconstruction after mastectomy. Breast 2011;20 Suppl 3:S104-7. [Crossref] [PubMed]
- Lambert K, Mokbel K. Does post-mastectomy radiotherapy represent a contraindication to skin-sparing mastectomy and immediate reconstruction: an update. Surg Oncol 2012;21:e67-74. [Crossref] [PubMed]
- Jagsi R, Jiang J, Momoh AO, et al. Complications After Mastectomy and Immediate Breast Reconstruction for Breast Cancer: A Claims-Based Analysis. Ann Surg 2016;263:219-27. [Crossref] [PubMed]
- Korwar V, Skillman J, Matey P. Skin reducing mastectomy and immediate reconstruction: the effect of radiotherapy on complications and patient reported outcomes. Eur J Surg Oncol 2014;40:442-8. [Crossref] [PubMed]
- Reish RG, Lin A, Phillips NA, et al. Breast reconstruction outcomes after nipple-sparing mastectomy and radiation therapy. Plast Reconstr Surg 2015;135:959-66. [Crossref] [PubMed]
- Pinsolle V, Grinfeder C, Mathoulin-Pelissier S, et al. Complications analysis of 266 immediate breast reconstructions. J Plast Reconstr Aesthet Surg 2006;59:1017-24. [Crossref] [PubMed]
- Whitfield GA, Horan G, Irwin MS, et al. Incidence of severe capsular contracture following implant-based immediate breast reconstruction with or without postoperative chest wall radiotherapy using 40 Gray in 15 fractions. Radiother Oncol 2009;90:141-7. [Crossref] [PubMed]
- Behranwala KA, Dua RS, Ross GM, et al. The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconstr Aesthet Surg 2006;59:1043-51. [Crossref] [PubMed]
- Albornoz CR, Matros E, McCarthy CM, et al. Implant breast reconstruction and radiation: a multicenter analysis of long-term health-related quality of life and satisfaction. Ann Surg Oncol 2014;21:2159-64. [Crossref] [PubMed]
- Preminger BA, Trencheva K, Chang CS, et al. Improving access to care: breast surgeons, the gatekeepers to breast reconstruction. J Am Coll Surg 2012;214:270-6. [Crossref] [PubMed]
- Howard-McNatt M, Forsberg C, Levine EA, et al. Breast cancer reconstruction in the elderly. Am Surg 2011;77:1640-3. [PubMed]
- Woerdeman LA, Hage JJ, Hofland MM, et al. A prospective assessment of surgical risk factors in 400 cases of skin-sparing mastectomy and immediate breast reconstruction with implants to establish selection criteria. Plast Reconstr Surg 2007;119:455-63. [Crossref] [PubMed]
- Lin KY, Johns FR, Gibson J, et al. An outcome study of breast reconstruction: presurgical identification of risk factors for complications. Ann Surg Oncol 2001;8:586-91. [Crossref] [PubMed]
- Alderman AK, Wilkins EG, Kim HM, et al. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2002;109:2265-74. [Crossref] [PubMed]
- Davies K, Allan L, Roblin P, et al. Factors affecting post-operative complications following skin sparing mastectomy with immediate breast reconstruction. Breast 2011;20:21-5. [Crossref] [PubMed]
- Vargas CR, Koolen PG, Anderson KE, et al. Mastectomy skin necrosis after microsurgical breast reconstruction. J Surg Res 2015;198:530-4. [Crossref] [PubMed]
- Gfrerer L, Mattos D, Mastroianni M, et al. Assessment of patient factors, surgeons, and surgeon teams in immediate implant-based breast reconstruction outcomes. Plast Reconstr Surg 2015;135:245e-52e. [Crossref] [PubMed]
- Xue DQ, Qian C, Yang L, et al. Risk factors for surgical site infections after breast surgery: a systematic review and meta-analysis. Eur J Surg Oncol 2012;38:375-81. [Crossref] [PubMed]
- Albornoz CR, Cordeiro PG, Farias-Eisner G, et al. Diminishing relative contraindications for immediate breast reconstruction. Plast Reconstr Surg 2014;134:363e-369e. [Crossref] [PubMed]
- Angarita FA, Acuna SA, Torregrosa L, et al. Perioperative variables associated with surgical site infection in breast cancer surgery. J Hosp Infect 2011;79:328-32. [Crossref] [PubMed]
- Waljee JF, Ubel PA, Atisha DM, et al. The choice for breast cancer surgery: can women accurately predict postoperative quality of life and disease-related stigma? Ann Surg Oncol 2011;18:2477-82. [Crossref] [PubMed]
- Damen TH, de Bekker-Grob EW, Mureau MA, et al. Patients' preferences for breast reconstruction: a discrete choice experiment. J Plast Reconstr Aesthet Surg 2011;64:75-83. [Crossref] [PubMed]
- Kim MK, Kim T, Moon HG, et al. Effect of cosmetic outcome on quality of life after breast cancer surgery. Eur J Surg Oncol 2015;41:426-32. [Crossref] [PubMed]
- Kim SW, Lee HK, Kang SM, et al. Short-term outcomes of immediate breast reconstruction using an implant or tissue expander after mastectomy in breast cancer patients. Breast Cancer 2016;23:279-85. [Crossref] [PubMed]
- Meretoja TJ, von Smitten KA, Leidenius MH, et al. Local recurrence of stage 1 and 2 breast cancer after skin-sparing mastectomy and immediate breast reconstruction in a 15-year series. Eur J Surg Oncol 2007;33:1142-5. [Crossref] [PubMed]
- Lim W, Ko BS, Kim HJ, et al. Oncological safety of skin sparing mastectomy followed by immediate reconstruction for locally advanced breast cancer. J Surg Oncol 2010;102:39-42. [Crossref] [PubMed]
- Yang X, Zhu C, Gu Y. The prognosis of breast cancer patients after mastectomy and immediate breast reconstruction: a meta-analysis. PLoS One 2015;10:e0125655. [Crossref] [PubMed]


