
This article has an erratum available at: http://dx.doi.org/10.21037/gs-2023-03 the article has been update on 2023-05-17 at here.
Simultaneous nipple reconstruction in autologous breast reconstruction
Introduction
Skin-sparing mastectomy with immediate autologous latissimus breast reconstruction has been used increasingly in recent years (1). This combination is safe and offers high-quality aesthetic results (2).
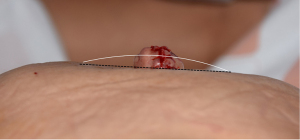
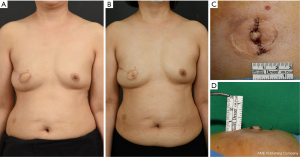
Nipple reconstruction is the final step in surgical restoration of the natural breast. Mastectomy involving nipple excision represents the treatment of choice when an intraoperative frozen biopsy of the peri-nipple area tissue is positive. In most of these cases, immediate breast reconstruction can be offered to overcome the psychological burden caused by the disfigurement resulting from the loss of the breast (3). In general, reconstruction of the nipple-areola complex (NAC) is delayed several months and is a separate procedure subsequent to the healing process of the autologous or implant-based breast reconstruction (4). The importance of NAC in body image perception, sexuality, and self-esteem of women and the significance of its reconstruction is increasingly being recognized by clinicians (5). An Ideal reconstruction of the NAC requires symmetry in position, size, shape, texture, pigmentation, and permanent projection (6). There are many innovative ways to create a nipple and each method has its unique characteristics that apply to certain breast types (7). Variable techniques, such as C-V, Hammond, and star flaps and inserting autologous cartilage, scar tissue, or silicone implant, have been reported, and surgeons tend to reconstruct symmetrical to the contralateral nipple in terms of shape, size, position, and projection (8-12). These techniques generally include designing the skin flap in various shapes and elevating the random flap for reconstructing a round, convex nipple of approximately 1 cm in width. Setting autologous, allogenic, and synthetic materials are available for projection augmentation (13). Reconstructing in two stages to prevent postoperative complications-such as venous congestion, partial necrosis, projection shrinkage, or infection-also attempted. To the best of our knowledge, these techniques tend to flatten the breast mound because they draw tissue from the mound itself for flap elevation and not from the surplus tissue (Figure 1).
This study began with the question “Would immediate nipple reconstruction be possible while performing an autologous tissue transfer?” Mastectomy followed by nipple excision would be an aggravating psychological stress for a patient (14). We assumed that these psychological burdens could subside if breast and nipple reconstruction is done simultaneously.
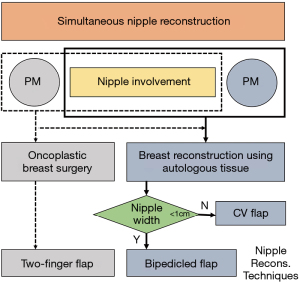
Because secondary breast reconstruction using classic local flaps or inserting the ADM into the nipple scar tissue can give disappointing results, we propose a reconstruction algorithm dependent on contralateral nipple size, outcomes, and patient satisfaction for simultaneous nipple reconstruction (SNR) during breast reconstruction with the autologous latissimus dorsi (LD) flap after total or partial mastectomy, the position of which is immediately defined because the skin envelope has been preserved and the limits of the breast have been restored (15,16).
We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/gs-21-338).
Methods
This single center study included 40 Korean patients who underwent nipple reconstruction between October 2016 and December 2020. The SNR experimental group was evaluated prospectively and the control group retrospectively, which two groups went through commonly set protocol. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved on January 4th, 2021 by Institutional Review Board (KNUCH2020-11-041-001) of the Kyungpook National University Chilgok Hospital (www.e-irb.com) and informed consent was taken from all the patients.
We proposed our algorithm of SNR to patients who were being considered for skin-sparing mastectomy and nipple excision (Figure 2). We included 21 patients who underwent delayed nipple reconstruction 6 months after breast reconstruction in the control group and 19 patients who underwent nipple reconstruction simultaneously with breast reconstruction in the experimental group. We collected data on nipple profile (width, projection) of all patients at preoperative, postoperative 6-month, and postoperative 1-year time periods. We used the healthy-side nipple profile to derive the ratio of width and projection. The patients were also photographed in a studio of a professional photographer in five standard projections (one anterior, two lateral, and two anterior oblique) with nipple view (anterior, lateral).
Operative technique
After main specimen was removed with sufficient safety margins, the surgeon obtained ductal tissue from just beneath of the nipple to evaluate the involvement of breast cancer as intraoperative frozen method. If the result of frozen section was confirmed as involvement of breast cancer, the breast surgeon removed the nipple only or nipple-areolar complex. After the removal of breast cancer was completed by breast surgeons, the breast reconstruction was conducted by plastic surgeons. In case of breast asymmetry with LD flap reconstruction only, a small silicone implant ranging 100–150 cc was inserted under the flap. To preserve the thoracodorsal artery, the surgeon fully detached the humeral attachment area and released the fascia or tendon, which might have drawn or twisted the main pedicle. In addition, the thoracodorsal nerve was cut to minimize jerking. Next, flap weight was measured with a portable scale to determine whether to insert an implant by comparing the weight with the mastectomy weight. If the LD flap weighed below the mastectomy weight, an antibiotic solutions (povidone-iodine, 50 cc; isepamicin, 80 mg; cefazolin, 1 g in 500 mL of sterile saline) was used to irrigate the breast pocket, followed by implant insertion without using an ADM. Two 800-cc negative drains were placed inferiorly and in the midaxillary direction in the back donor site, and two 400-cc negative drains were positioned above and under the LD flap.
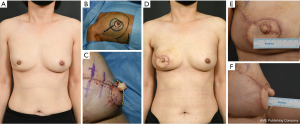
During the breast reconstruction procedure, both breast contour and symmetry were adjusted, followed by SNR. The position of the new NAC was well defined by the shape of the skin envelope (17,18). The surgeon indicated the nipple on the reconstructed LD flap skin where the excised nipple originally belonged and designed the new nipple by the algorithm depending on the projection of the contralateral healthy-side nipple. The rest of the skin paddle was then de-epithelialized. Classic C-V flap with 105–110% the size of the desired nipple size was designed in case the contralateral nipple projection was >1 cm, and the bipedicled flap or two-finger flap was designed at 110–120% the size of the desired nipple size if the contralateral nipple was <1 cm (Figures 3,4). The postoperative reconstructed nipple was sealed with a hand-made patient-adjusted nipple cap that was mixed with BASE and CATALYST of Aquasil Soft Putty and maintained for 3 months with ointment QD dressing (Video 1).


Statical analysis
We collected basic patient demographics such as age, body mass index (BMI), cancer stage, and reconstruction method. We collected objective data on nipple symmetry by analyzing the profile (projection, width) of the reconstructed nipple in preoperative, postoperative 6-month, and postoperative 1-year time period and also compared each ratio with the contralateral nipple. We created a patient questionnaire focused on the subjective perception of the shape and position of the reconstructed nipple. We evaluated patient satisfaction at postoperative 1-year follow up using a modified VAS score of 1–5. We performed statistical analysis using SPSS Statistics for Windows, version 16.0 (SPSS Inc., Chicago, IL, USA) and considered the differences as statistically significant if the P value was <0.05 using Student’s t-test.
Results
For the control and experimental groups, the mean patient age was 48.9 years (range, 35–68 years) and 50.3 years (range, 39–65 years), BMI was 24.4 kg/m2 (range, 19.23–34.1 kg/m2) and 23.4 kg/m2 (range, 18.0–29.2 kg/m2), and excised mass weight was 337.9 g (range, 191–600 g) and 353.7 g (range, 37–762 g), respectively. Ductal carcinoma in situ (DCIS) was diagnosed in 7 cases (33.3%) and 6 cases (31.6%), invasive lobular carcinoma (ILC) in 2 cases (9.5%) and 1 case (5.3%), invasive ductal carcinoma (IDC) in 12 cases in both (57.1% and 63.2%), cancer Stage 0 in 2 cases in both (9.5% and 10.5%), Stage I in 7 cases in both (33.3% and 36.8%), Stage II in 8 cases in both (38.1% and 42.1%), and Stage III in 4 cases (19.0%) and 2 cases (10.5%) in the control and the experimental groups, respectively. There were no Stage IV cases. C-V flap was performed in 17 and 12 patients, bipedicled flap in 3 and 5 patients, and two-finger flap in 0 and 2 patients in the control and experimental groups, respectively (Table 1).
Table 1
| Patient demographic | Delayed nipple reconstruction (N=21) | Simultaneous nipple reconstruction (N=19) | P value |
|---|---|---|---|
| Age, years, mean ± SD | 48.9±6.9 | 50.3±11.7 | 0.001 |
| BMI, kg/m2, mean ± SD | 24.4±3.8 | 23.4±2.5 | 0.052 |
| Excised mass weight (g) | 337.9±131.5 | 353.7±156.6 | 0.033 |
| Breast cancer | 0.2 | ||
| Tumor type, N (%) | |||
| DCIS | 7 (33.3) | 6 (31.6) | |
| ILC | 2 (9.5) | 1 (5.3) | |
| IDC | 12 (57.1) | 12 (63.2) | |
| Cancer stage, N (%) | 0.03 | ||
| Stage 0 | 2 (9.5) | 2 (10.5) | |
| Stage I | 7 (33.3) | 7 (36.8) | |
| Stage II | 8 (38.1) | 8 (42.1) | |
| Stage III | 4 (19.0) | 2 (10.5) | |
| Lymph node dissection, N (%) | 0.102 | ||
| SLNB | 16 (76.2) | 15 (78.9) | |
| ALND | 5 (23.8) | 4 (21.1) | |
| Nipple reconstruction type | 0.343 | ||
| C-V flap | 17 | 12 | |
| Hammond flap | 1 | – | |
| Bipedicled flap | 3 | 5 | |
| Two-finger flap | – | 2 |
N, number of patients; LD, latissimus dorsi flap; SD, standard deviation; IDC, invasive ductal carcinoma; DCIS, ductal carcinoma in situ; ILC, invasive lobular carcinoma; SLNB, sentinel lymph node biopsy; ALND, axillar lymph node dissection.
Outcome evaluation
For the control and experimental groups, patient satisfaction scores averaged 3.4 and 4.1 for projection, 3.7 and 4.3 for width, 4.0 and 4.5 for shape, and 3.1 and 4.6 for surgical time, respectively (Table 2).
Table 2
| Question about reconstructed nipple | Delayed nipple reconstruction | Simultaneous nipple reconstruction |
|---|---|---|
| Projection | 3.4±0.17 | 4.1±0.21 |
| Width | 3.7±0.11 | 4.3±0.07 |
| Shape | 4.0±0.14 | 4.5±0.12 |
| Surgical time | 3.1±0.13 | 4.6±0.17 |
| Overall outcomes | 3.6±0.18 | 4.5±0.16 |
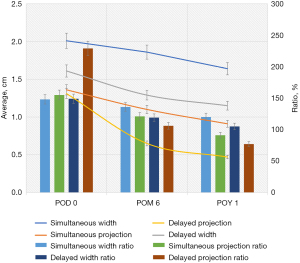
We measured nipple projection and width shrinkage over time and evaluated symmetry by calculating the ratio between the reconstructed and contralateral nipple. Over the preoperative, postoperative 6-month, and postoperative 1-year time periods, the control group had a gradual decline in scores over each period, with 1.31, 0.65, and 0.47 scores for projection and 1.61, 1.29, and 1.15 scores for width, respectively. The experimental group underwent a slight decline of 1.36, 1.1, and 0.91 for projection and 2.01, 1.86, and 1.64 for width, respectively. In terms of ratio as compared with the contralateral nipple, the differences become more distinct between the control and experimental groups across the three time periods, respectively: 229%, 106%, and 77% and 155%, 121%, and 91% for projection ratio; 149%, 119%, and 105% and 148%, 136%, and 120% for width ratio (Figure 5).
Discussion
The demand for immediate breast reconstruction after total or partial mastectomy when oncological safety has been demonstrated is increasing (19). Skin-sparing mastectomy is technically more difficult compared with modified radical mastectomy, but the primary advantage of this technique is the aesthetic and psychological results obtained from immediate breast reconstruction (20). The incidence of occult NAC involvement in breast cancer has been reported as 5–12% (21). If nipple involvement of cancer is shown in preoperative imaging or is strong suspected clinically, nipple excision is performed, accompanied by skin-sparing mastectomy.
Considering a delayed nipple reconstruction when the postoperative scar is more stable after chemotherapy or radiotherapy has been a classic pathway for nipple reconstruction (22). The areola removed during mastectomy was replaced by skin from the LD flap, and the nipple was reconstructed on this flap after an interval of several months. However, besides the burden of an additional operation for patients, a great aesthetic outcome is usually not secured (23). Numerous techniques have been described for nipple reconstruction following mastectomy (e.g., using autologous tissue or materials such as collagen or silicone implant), but none is entirely satisfactory (24).
The continuous progress in the treatment of breast cancer treatment and increasing public awareness on the possibilities of breast reconstruction have stimulated the development of new concepts in NAC reconstruction. Numerous techniques were created over the years, whereas some methods have been discredited (25). A previous study reported the technique of immediate NAC reconstruction during immediate breast reconstruction using two local skin flaps from the LD flap in a group of 30 patients (26). At present, as the psychological benefits of NAC reconstruction has been receiving more attention (26), several authors have begun to reconstruct the nipple and breast in a single stage to improve the overall patient satisfaction (27,28). However, technical consensus has not been established because the most common problem following nipple reconstruction is that projection of the new nipple tends to shrink at most over 50% by time (29,30). The projection of reconstructed nipple is influenced essentially by two factors: (I) retraction forces of surrounding and underlying tissues and (II) tissue contraction of the flap (31). As the reconstructed nipple is subject to the substantial retraction forces of surrounding and underlying tissues, an unpredictable gradual loss of projection remains a challenge. Moreover, peri-reconstructed nipple flat phenomenon is inevitable, as most of the techniques designing the nipple on the mastectomy flap or the autologous flap, which is the random flap, draws the peri-nipple tissue for reconstructing the nipple (Figure 1).
In contrast, the SNR technique we present in this article gives a greater residual projection than that obtained with other procedures, such as Kroll et al.’s modified double-opposing tab flap (32) or the C-V flap of Losken et al. (33). To reduce patient’s previous burdens and discomforts, we set an algorithm in nipple reconstruction expecting reliable outcomes and conducted a comparison analysis (Figure 6).
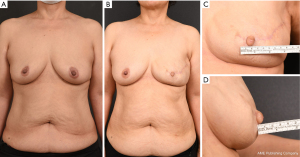
An extended LD flap following total mastectomy could cover most of the Asian breast, which is commonly applied in small to moderate breast volume, but a recent LD flap combined with a small implant insertion extended breast size in reconstruction. While in partial mastectomy followed by oncoplastic reduction mammoplasty, SNR using a two-finger flap is considered. By extending the median incision of reduction mammoplasty, the bilateral flap is elevated and approximated into the nipple-shaped flap. The nipple base is formed concave from the lateral margin of the bilateral flap, and the nipple tip is from the medial margin of both bilateral flaps. This simple, reliable technique is especially useful for reconstructing small nipples during reduction mammoplasty (Figure 7).
SNR is a reconstruction technique aligning symmetry of breast contour when the nipple or NAC is excised. This technique has several advantages. First, two types of reconstruction-breast and nipple-are performed simultaneously. Second, the procedure minimizes projection loss due to scar formation or contracture because the nipple and mastectomy flaps have different main blood supplies and wound healing. Third, two times the size of the contralateral nipple is generally reconstructed considering approximate 30% to 50% shrinkage over time; however, in this technique we used 1.1–1.3 times the size, which resulted in less reduction and good maintenance over 1 year, which is reconstructed because of volume replacement and not volume displacement. Fourth, this technique enables small nipple reconstruction while rather thick skin from the LD flap was difficult to reconstruct a small nipple <1 cm using ordinary local flap techniques.
By these classic techniques, which create a large-sized nipple considering volume loss, only the projection but not the width is severely reduced with time, followed by a poor aesthetic outcome and low patient satisfaction (34). However, our simultaneous “bipedicled flap” nipple reconstruction forms a tension-free, incision-less nipple (Figures 3,4,7). We propose that this bipedicled-flap technique enables nipple reconstruction in a broad range from a narrow, high nipple to a wide, low nipple. A single random pedicled skin flap supplies 2–3 flap tips in representative techniques and its variables, resulting in many reports of tissue loss owing to focal ischemia (35). The bipedicled flap reconstruction resolves these complications considerably with reliable aesthetic outcomes and less projection reduction (Figures 6,7).
Flaps with bidirectional-rich vascularity have less shrinkage postoperatively. The elevated flap is simply folded by itself to form the round shape of the nipple, resulting in a good aesthetic outcome even in cases of delayed reconstruction (Figures 6,7). On the basis of these advantages, the approach we present maintains a stable nipple projection over a long period. Even with the classic C-V flap reconstruction in nipples >1 cm, the reconstructed nipple sustained a good outcome because the nipple-excised circular remnant defect of the postmastectomy skin contracted with time, which led to a concave, durable nipple base, and the nipple reconstructed from LD flap skin had a sufficient blood supply from the thoracodorsal artery (Figure 8). Moreover, this technique overcomes the postoperative flattened breast mound phenomenon because the reconstructed nipple is made of sufficient tissue from the LD skin flap, not from the near-breast tissue (Figure 9).

Several articles, including that by Cho et al. (36), have reported NAC necrosis after nipple-sparing mastectomy with immediate autologous breast reconstruction. However, in our approach and algorithm, no complications were observed until a year later. Because the SNR technique offers a respective blood supply source to the reconstructed nipple and mastectomy skin flap, the blood supply is sufficient and the healing process is separate. In addition, SNR provides another chance of revision with adequate skin, in case the new nipple is aborted or is inappropriately positioned.
Our experimental group also scored higher satisfaction with the SNR technique, avoiding the burden of an additional operation. Furthermore, we evaluated the ratio with the contralateral nipple profile, which has not been previously described. In fact, it is the aesthetic symmetry between both nipples that should be emphasized, not the maintenance of the reconstructed nipple’s profile. During the 1-year postoperative follow-up the mean projection of the immediately reconstructed nipple went nearly same with the contralateral nipple by 100%, whereas the delayed reconstructed nipple resulted in a 77% ratio. In contrast, the mean width at 1-year follow-up showed a 105% and 120% of ratio each in the control and experimental groups, respectively.
Nipple reconstruction is of capital importance for breast reconstruction patients, almost as important as breast volume (37). Some authors have observed that the presence of the nipple is a factor that helps balance of the reconstructed breast as part of the body image (37-39). Nipple reconstruction represents the simplest from a technical perspective but is among the most important from an aesthetic perspective (40). It is an integral part of the breast reconstruction process, as patients associate this stage with the end of the treatment and with a sense of completeness (41). Our simple, reliable technique gives a well-projecting nipple that has good stability.
This study has some limitations. First, the sample size was small, and the procedure did not include NAC tattooing, which is currently discussed in another report. In addition, the follow-up period was not long enough to compare longer term data between the two groups. Furthermore, additional study of the SNR technique using a thicker flap such as abdominal flap (e.g., TRAM or DIEP) is required.
This study was to establish algorithm of nipple reconstruction and it is potential to extend toward more objective study through detailed questionnaire comparing with contralateral nipple. Data is prospectively accumulating for larger patient pool and further analysis of each technique, outcomes and NAC profile systematization are in progress.
Conclusions
SNR as described in the presented algorithm may provide not only high patient satisfaction but also a reliable technique with a predictable aesthetic outcome. The one-stage reconstructive surgery may be psychologically beneficial to patients. Although our study is small, these preliminary results from using a new operative technique are encouraging.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/gs-21-338
Data Sharing Statement: Available at https://dx.doi.org/10.21037/gs-21-338
Peer Review File: Available at https://dx.doi.org/10.21037/gs-21-338
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/gs-21-338). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional Review Board of the Kyungpook National University Chilgok Hospital (KNUCH2020-11-041-001) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sood R, Easow JM, Konopka G, et al. Latissimus Dorsi Flap in Breast Reconstruction: Recent Innovations in the Workhorse Flap. Cancer Control 2018;25:1073274817744638 [Crossref] [PubMed]
- Sternberg EG, Perdikis G, McLaughlin SA, et al. Latissimus dorsi flap remains an excellent choice for breast reconstruction. Ann Plast Surg 2006;56:31-5. [Crossref] [PubMed]
- Wirth R, Banic A, Erni D. Aesthetic outcome and oncological safety of nipple-areola complex replantation after mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg 2010;63:1490-4. [Crossref] [PubMed]
- Zhong T, Antony A, Cordeiro P. Surgical outcomes and nipple projection using the modified skate flap for nipple-areolar reconstruction in a series of 422 implant reconstructions. Ann Plast Surg 2009;62:591-5. [Crossref] [PubMed]
- Sisti A, Tassinari J, Cuomo R, et al. Nipple-Areola Complex Reconstruction: Principles and Clinical Techniques. Springer Science Publishing: Berlin/Heidelberg, Germany, 2017; pp. 359-368.
- Boccola MA, Savage J, Rozen WM, et al. Surgical correction and reconstruction of the nipple-areola complex: current review of techniques. J Reconstr Microsurg 2010;26:589-600. [Crossref] [PubMed]
- Gougoutas AJ, Said HK, Um G, et al. Nipple-Areola Complex Reconstruction. Plast Reconstr Surg 2018;141:404e-16e. [Crossref] [PubMed]
- Collis N, Lalloo MT, Sharpe DT. Nipple reconstruction and mastectomy scars. Plast Reconstr Surg 2000;105:2277. [Crossref] [PubMed]
- Alfano C, Tenna S, Caggiati A, et al. Nipple reconstruction by local flaps: a long-term comparative study between star and skate techniques. Acta Chir Plast 2004;46:127-31. [PubMed]
- Di Benedetto G, Sperti V, Pierangeli M, et al. A simple and reliable method of nipple reconstruction using a spiral flap made of residual scar tissue. Plast Reconstr Surg 2004;114:158-61. [Crossref] [PubMed]
- Gamboa-Bobadilla GM. Nipple reconstruction: the top hat technique. Ann Plast Surg 2005;54:243-6. [PubMed]
- Guerra AB, Khoobehi K, Metzinger SE, et al. New technique for nipple areola reconstruction: arrow flap and rib cartilage graft for long-lasting nipple projection. Ann Plast Surg 2003;50:31-7. [Crossref] [PubMed]
- Winocour S, Saksena A, Oh C, et al. A Systematic Review of Comparison of Autologous, Allogeneic, and Synthetic Augmentation Grafts in Nipple Reconstruction. Plast Reconstr Surg 2016;137:14e-23e. [Crossref] [PubMed]
- Harcourt DM, Rumsey NJ, Ambler NR, et al. The psychological effect of mastectomy with or without breast reconstruction: a prospective, multicenter study. Plast Reconstr Surg 2003;111:1060-8. [Crossref] [PubMed]
- Delay E, Bremond A. Mastectomie avec conservation de l’e’tui cutane: [Concept, proble’mes, indications]. In: Namer M, Tessier E, Ferrero JM, eds. Les Traitements Me’dicaux des Cancers du Sein. Paris: Arnette. Oxford, United Kingdom: Blackwell; 1996:309-338.
- Delay E, Gratadour AC, Jorquera F, et al. Immediate autologous latissimus breast reconstruction after skin sparing mastectomy. Eur J Plast Surg 1999;22:111-8. [Crossref]
- Tanabe HY, Tai Y, Kiyokawa K, et al. Nipple-areola reconstruction with a dermal-fat flap and rolled auricular cartilage. Plast Reconstr Surg 1997;100:431-8. [Crossref] [PubMed]
- Brent B. Nipple-areola reconstruction following mastectomy: an alternative to the use of labial and contralateral nipple-areolar tissues. Clin Plast Surg 1979;6:85-92. [Crossref] [PubMed]
- Malata CM, McIntosh SA, Purushotham AD. Immediate breast reconstruction after mastectomy for cancer. Br J Surg 2000;87:1455-72. [Crossref] [PubMed]
- Simmons RM, Adamovich TL. Skin-sparing mastectomy. Surg Clin North Am 2003;83:885-99. [Crossref] [PubMed]
- Agha RA, Wellstead G, Sagoo H, et al. Nipple sparing versus skin sparing mastectomy: a systematic review protocol. BMJ Open 2016;6:e010151 [Crossref] [PubMed]
- Losken A, Duggal CS, Desai KA, et al. Time to completion of nipple reconstruction: what factors are involved? Ann Plast Surg 2013;70:530-2. [Crossref] [PubMed]
- Tierney BP, Hodde JP, Changkuon DI. Biologic collagen cylinder with skate flap technique for nipple reconstruction. Plast Surg Int 2014;2014:194087 [Crossref] [PubMed]
- Lee JS, Kwon JH, Lee JW, et al. Usefulness of Rapiplug in nipple reconstruction to improve nipple projection. ANZ J Surg 2019;89:E71-5. [Crossref] [PubMed]
- Farhadi J, Maksvytyte GK, Schaefer DJ, et al. Reconstruction of the nipple-areola complex: an update. J Plast Reconstr Aesthet Surg 2006;59:40-53. [Crossref] [PubMed]
- Goh SC, Martin NA, Pandya AN, et al. Patient satisfaction following nipple-areolar complex reconstruction and tattooing. J Plast Reconstr Aesthet Surg 2011;64:360-3. [Crossref] [PubMed]
- Delay E, Mojallal A, Vasseur C, et al. Immediate nipple reconstruction during immediate autologous latissimus breast reconstruction. Plast Reconstr Surg 2006;118:1303-12. [Crossref] [PubMed]
- Ma G, Richardson H, Pacella SJ, et al. Single-stage breast reconstruction following areola-sparing mastectomy. Plast Reconstr Surg 2009;123:1414-7. [Crossref] [PubMed]
- Jamnadas-Khoda B, Thomas R, Heppell S. The 'cigar roll' flap for nipple areola complex reconstruction: a novel technique. J Plast Reconstr Aesthet Surg 2011;64:e218-20. [Crossref] [PubMed]
- Jones AP, Erdmann M. Projection and patient satisfaction using the "Hamburger" nipple reconstruction technique. J Plast Reconstr Aesthet Surg 2012;65:207-12. [Crossref] [PubMed]
- Nimboriboonporn A, Chuthapisith S. Nipple-areola complex reconstruction. Gland Surg 2014;3:35-42. [PubMed]
- Kroll SS, Reece GP, Miller MJ, et al. Comparison of nipple projection with the modified double-opposing tab and star flaps. Plast Reconstr Surg 1997;99:1602-5. [Crossref] [PubMed]
- Losken A, Mackay GJ, Bostwick J 3rd. Nipple reconstruction using the C-V flap technique: a long-term evaluation. Plast Reconstr Surg 2001;108:361-9. [Crossref] [PubMed]
- Mori H, Uemura N, Okazaki M. Nipple reconstruction with banked costal cartilage after vertical-type skin-sparing mastectomy and deep inferior epigastric artery perforator flap. Breast Cancer 2015;22:95-7. [Crossref] [PubMed]
- Lee JS, Eom JR, Lee JW, et al. Safe delayed procedure of nipple reconstruction in poorly circulated nipple. Breast J 2019;25:129-33. [Crossref] [PubMed]
- Cho JW, Yoon ES, You HJ, et al. Nipple-Areola Complex Necrosis after Nipple-Sparing Mastectomy with Immediate Autologous Breast Reconstruction. Arch Plast Surg 2015;42:601-7. [Crossref] [PubMed]
- Wellisch DK, Schain WS, Noone RB, et al. The psychological contribution of nipple addition in breast reconstruction. Plast Reconstr Surg 1987;80:699-704. [Crossref] [PubMed]
- Schain WS, Wellisch DK, Pasnau RO, et al. The sooner the better: a study of psychological factors in women undergoing immediate versus delayed breast reconstruction. Am J Psychiatry 1985;142:40-6. [Crossref] [PubMed]
- Rosenqvist S, Sandelin K, Wickman M. Patients' psychological and cosmetic experience after immediate breast reconstruction. Eur J Surg Oncol 1996;22:262-6. [Crossref] [PubMed]
- Few JW, Marcus JR, Casas LA, et al. Long-term predictable nipple projection following reconstruction. Plast Reconstr Surg 1999;104:1321-4. [Crossref] [PubMed]
- Sisti A, Grimaldi L, Tassinari J, et al. Nipple-areola complex reconstruction techniques: A literature review. Eur J Surg Oncol 2016;42:441-65. [Crossref] [PubMed]


