Symptom clusters using the Brief Pain Inventory in patients with breast cancer
Introduction
Patients with cancer often experience several disease- and treatment- related symptoms, highlighting the importance of sensitivity and responsiveness to symptom identification and control in their care. Symptom clusters are groups of a minimum of two symptoms that co-occur in patients. Due to their implications on management of patient quality of life, they are of great clinical interest (1). Although symptom cluster research was recently named a priority in oncology nursing, there is limited data regarding symptom clusters in patients undergoing chemotherapy (2).
The majority of research conducted on symptom management in patients with breast cancer (BC) is focused on isolated symptoms, with the most prevalent being fatigue, pain, anxiety and depression (3). A literature review conducted by Nguyen et al. amalgamated results from five relevant studies published from 2005 to 2009 on symptom clusters in BC patients (4). However, these studies differed in terms of the number of clusters and the composition of items across clusters.
With great inter- and intra- patient variability cited in BC patients undergoing adjuvant chemotherapy, there are several challenges associated with the management of quality of life in these patients (5). Although currently limited, research on symptom cluster in women with BC undergoing chemotherapy may better illustrate the experiences of this patient population, and facilitate improved symptom identification and management. The aim of the present study is to investigate symptom clusters in patients with non-metastatic BC during and after chemotherapy.
Methods
This is a secondary analysis of a prospective study on docetaxel-associated pain syndrome, which accrued patients with non-metastatic BC commencing taxane chemotherapy at the Sunnybrook Odette Cancer Centre and North York General Hospital (6). Ethical approval for the study was obtained at the respective institutions, and all patients provided informed consent. Patients were followed for the first three consecutive cycles of docetaxel, paclitaxel or nab-paclitaxel chemotherapy.
The brief pain inventory (BPI) is a multiple-item measure of pain used extensively in the cancer patient population (7). The sensory component measures intensity of pain on 4 different scales (worst, least, average, and current pain) wherein higher scores are indicative of worse pain. The affective component of the BPI assesses the effect of pain on 7 functional items at baseline: general activity, normal work, walking ability, mood, sleep, relationships and enjoyment of life. The BPI utilizes an 11-point scale, wherein higher scores are indicative of greater functional interference.
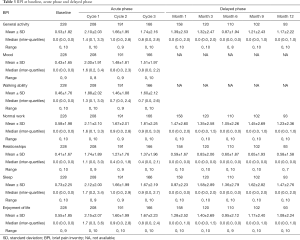
In the present study, patients completed the BPI at baseline, throughout days 1–21 during all three cycles (acute phase), and again at 1, 3, 6, 9, and 12 months post-treatment (delayed phase). During the delayed phase, mood and walking ability were not assessed. Average BPI scores were calculated for cycles 1–3 and used in the analysis. Consent was provided by all patients. Ethical approval was obtained from the hospital research ethics board.
Statistical analysis
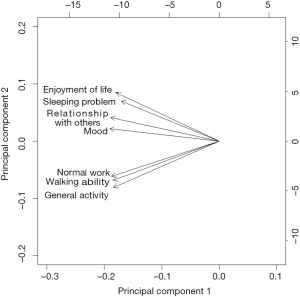
Descriptive analyses were performed on demographics and medication taken during treatment cycles, and were summarized as mean, standard deviation (SD), median, inter-quartiles and range for continuous variables, and proportions for categorical variables. BPI items were summarized at baseline, acute phase during treatment and delayed phase post-treatment. Spearman correlation was conducted at baseline, during and post-treatments. A principle component analysis (PCA) with varimax rotation was conducted on the BPI scores to delineate symptom clusters at baseline, at each cycle of the acute phase, and at 1, 3, 6, 9, and 12 months delayed phase. This statistical procedure transforms a number of observed variables into a smaller number of variables or “principal components”, wherein the first component accounts for as much variability in the data as possible. The number of significant principal components was selected with an Eigenvalue higher than 0.6 and each component explained more than 10% of the variance. The highest factor loading score predicted the assignment of individual symptoms to an independent factor. Cronbach’s alpha values were calculated to estimate the internal consistencies and reliabilities of symptom clusters. The varimax rotation is an orthogonal rotation, meaning that it results in uncorrelated components. Compared to other types of rotations, a varimax rotation tends to maximize the variance of a column of the factor pattern matrix. Robust relationships and correlations among symptoms were displayed with the biplot graphic. The longer the length and closer together the arrows were, the higher the correlation between symptoms. All analyses were conducted using Statistical Analysis Software (SAS version 9.4 for Windows).
Results
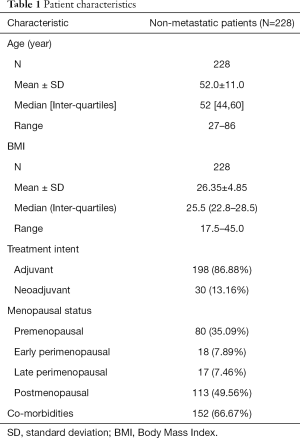
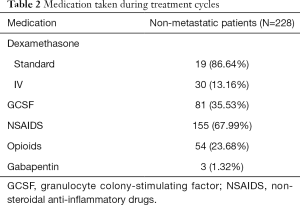
A total of 228 patients were accrued to the study. Patient characteristics are found in Table 1. The mean age was 52 years, with almost half of patients post-menopausal. Out of the three regimens, docetaxel was administered the most (88%). Most patients were chemotherapy naïve (92%). Medications taken during treatment are listed in Table 2. Descriptions of the BPI scores collected at the different phases of the study are provided in Table 3.
Full table
Full table
Full table
Baseline
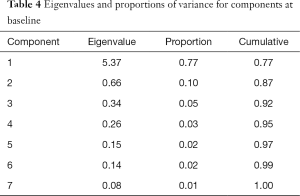
Spearman correlations between all BPI items were significant with P values <0.0001. Using the criterion of minimum eigenvalue of 0.60 and at least 10% of the total variance, the first two components accounted for 77% and 10% of the total variance respectively (Table 4). Cumulatively, 87% of the variance was accounted for.
Full table
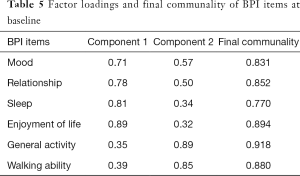
Cluster 1 was composed of mood, relationships, sleep and enjoyment of life. Cluster 2 consisted of general activity, walking ability and normal work. Final communality is the proportion of variance in an observed variable that is accounted for by the retained clusters. Values in this study showed that all variables were well accounted for by the two clusters, with final communalities ranging from 0.77 (sleep) to 0.92 (general activity) (Table 5). Cronbach’s alpha values demonstrated good internal consistency with values of 0.93 and 0.94 for the two clusters respectively. The two clusters can also be observed in the biplot (Figure 1).
Full table
Delayed phase
In delayed phase, clusters were identified at 1 and 3 months post-treatment. BPI scores for mood and walking ability were not collected during delayed phase. Spearman correlations at months 1 and 3 between the remaining 5 BPI items were all significant, with P values <0.0001.
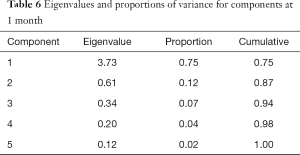
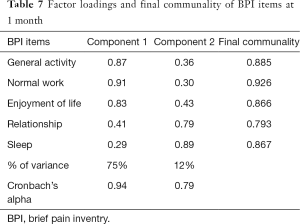
At 1 month post-treatment, 2 clusters were identified, respectively accounting for 75% and 12% of the total variance (Table 6). Cumulatively, the clusters explained 87% of the variance. Cluster 1 was composed of general activity, normal work and enjoyment of life. Cluster 2 was composed of relationships and sleep. Final communality values ranged from 0.79 (relationships) to 0.93 (normal work) (Table 7). Cronbach’s alpha values for the two clusters were 0.94 and 0.79 respectively, indicating good internal consistencies.
Full table
Full table
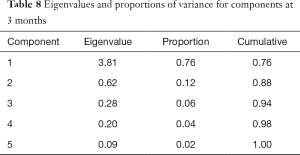
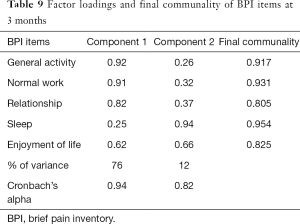
At 3 months post-treatment, 2 clusters were identified, respectively accounting for 76% and 12% of the total variance (Table 8). Cumulatively, they accounted for 88% of the total variance. Cluster 1 was composed of general activity, normal work and relationships. Cluster 2 was composed of sleep and enjoyment of life. Final communalities ranged from 0.81 (relationships) to 0.95 (sleep) (Table 9). Cronbach’s alpha values for the two clusters were 0.94 and 0.82 respectively, indicating good internal consistencies.
Full table
Full table
Discussion
Two functional interference clusters were found in three different stages in the study, at baseline and at 1- and 3-month post-treatment. General activity and normal work consistently clustered together. At baseline, we observed two clusters: physical interference (general working, normal work, walking ability) and psychosocial interference (mood, relationships, sleep and enjoyment of life). These clusters are identical to those observed by Klepstad et al. in their study sample of cancer patients (8). Emergence of psychosocial-/mood- and activity-related clusters using the BPI in cancer patients have been noted elsewhere in the literature (9-10). A previous analysis conducted by Chiu et al. reported that BPI interference scores correlated best with the average pain scale for patients experiencing taxane-induced arthralgia and myalgia, such as those in the present study sample (11). In contrasting the more stable nature of pain of non-metastatic compared to metastatic patients, the authors recommended use of this BPI scale in future evaluations of the symptom in this particular population.
Studies conducted in BC patients during and after treatment have used other symptom assessment tools. Implementing four different questionnaires across the span of chemotherapy and radiotherapy, Kim et al. observed a psychoneurological cluster in BC patients composed of cognitive disturbances, depressed mood, fatigue, insomnia and pain (12). This remained stable throughout treatment, with the exception of hot flashes appearing and disappearing after the initiation of treatment. Using the Profile of Mood States, EORTC-QLQ-C30 and -BR23, Evangelista and Santos observed physical (dyspnea, pain, arm symptoms, insomnia) and psychoemotional (depression, confusion, anger, tension, fatigue, breast symptoms) symptom clusters in their study of 138 BC patients following completion of adjuvant chemotherapy with curative intent (13). Bender et al. conducted a pooled analysis of results from three independent studies with women at different phases of BC, following primary resection, adjuvant chemotherapy and metastatic development. Their analysis identified 3 symptom clusters corresponding to different phases, composed of symptoms relating to fatigue, perceived cognitive impairment and mood (14). So et al. investigated the symptoms reported to be the most prevalent in BC patients (fatigue, pain, anxiety and depression) and observed significant correlations between them (15). In addition to confirming the existence of this symptom cluster, the authors remarked on the adverse effect of increased symptomatology in this group on patient quality of life.
Like our present study, an analysis conducted by Albusoul et al. used a sample of solely BC patients undergoing adjuvant chemotherapy (16). Their results departed from those of previous studies in this patient population, reporting that clusters were dynamic rather than stable (12,17-19). This was also observed in our study, with no two identical clusters emerging across the span of the study. Albusoul et al. reported a treatment-related cluster which at baseline, was composed of anxiety, appearance, concentration and sleep disturbance. At the third cycle of chemotherapy, bowel pattern, fatigue, pain and depression joined the cluster. At the fourth cycle, the cluster contained appetite, depression, fatigue, anxiety, appearance and concentration. At the 1-month mark post-treatment, the cluster divided into two: cluster 1, consisting of fatigue, pain and sleep disturbance; and cluster 2, containing anxiety, appearance and concentration.
There are several limitations to the present study. Since assessment of mood and walking ability were not assessed in the delayed phase in the primary study, the possible inclusion of these items in delayed phase symptom clusters could not be evaluated in this secondary analysis. Another limitation in our study is the low minimum Eigenvalue (0.60) used for cluster inclusion. Using the principal component analysis on average BPI scores, we were unable to identify significant clusters during the acute phase. Therefore, further research is required using the same patient population to assess the validity of the symptom clusters identified.
Conclusions
BC patients may present with symptom clusters in physical and psychological interference. Symptom clusters were identified in the delayed phase and were different at the assessed stages, indicating dynamic behavior. Given the demonstration of clusters and a lack of functional recovery to baseline levels, symptoms should be continuously managed following completion of chemotherapy.
Acknowledgements
We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval for the study was obtained at the respective institutions and written informed consent was obtained from all patients.
References
- Chow E, Fan G, Hadi S, et al. Symptom clusters in cancer patients with bone metastases. Support Care Cancer 2007;15:1035-43. [Crossref] [PubMed]
- Oncology Nursing Society. Oncology Nursing Society 2014-2018 Research Agenda. 2014. Available online: https://www.ons.org/sites/default/files/2014-2018%20ONS%20Research%20Agenda%20Executive%20Summary.pdf
- National Institutes of Health. State-of-the-Science Conference Statement on symptom management in cancer: Pain, depression, and fatigue. JNCI Monographs 2004;32:9-16. [PubMed]
- Nguyen J, Cramarossa G, Bruner D, et al. A literature review of symptom clusters in a patients with breast cancer. Expert Rev Pharmacoecon Outcomes Res 2011;11:533-9. [Crossref] [PubMed]
- Miakowski C, Cooper BA, Paul SM, et al. Subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: a cluster analysis. Oncol Nurs Forum 2006;33:E79-89. [Crossref] [PubMed]
- Chiu N, Zhang L, Dent R, et al. A prospective study of docetaxel-associated pain syndrome. Support Care Cancer. 2018;26:203-11. [Crossref] [PubMed]
- Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore 1994;23:129-38. [PubMed]
- Klepstad P, Loge JH, Borchgrevink PC, et al. The Norwegian Brief Pain Inventory questionnaire: Translation and validation in cancer pain patients. J Pain Symptom Manage 2002;24:517-25. [Crossref] [PubMed]
- Saxena A, Mendoza T, Cleeland CS. The assessment of cancer pain in North India: The validation of the Hindi Brief Pain Inventory – BPI-H. J Pain Symptom Manage 1999;17:27-41. [Crossref] [PubMed]
- Chow E, James J, Barsevick A, et al. Functional interference clusters in cancer patients with bone metastases: A secondary analysis of RTOG 9714. Int J Radiat Oncol Biol Phys 2010;76:1507-11. [Crossref] [PubMed]
- Chiu N, Zhang L, Gallo-Hershberg D, et al. Which pain intensity scale from the Brief Pain Inventory correlates most highly with functional interference scores in patients experiencing taxane-induced arthralgia and myalgia? Support Care Cancer 2016;24:2979-88. [PubMed]
- Kim HJ, Barsevick A, Tulman L, et al. Treatment-related symptom clusters in breast cancer: a secondary analysis. J Pain Symptom Manage 2008;36:468-79. [Crossref] [PubMed]
- Evangelista AL, Santos EM. Cluster of symptoms in women with breast cancer treated with curative intent. Support Care Cancer 2012;20:1499-506. [Crossref] [PubMed]
- Bender CM, Ergyn FS, Rosenzweig MQ, et al. Symptom clusters in breast cancer across 3 phases of the disease. Cancer Nurs 2005;28:219-25. [Crossref] [PubMed]
- So WK, Marsh G, Ling WM, et al. The symptom cluster of fatigue, pain, anxiety, and depression and the effect on the quality of life of women receiving treatment for breast cancer: a multicenter study. Oncol Nurs Forum 2009;36:E205-14. [Crossref] [PubMed]
- Albusoul RM, Berger AM, Gay CL, et al. Symptom clusters change over time in women receiving adjuvant chemotherapy for breast cancer. J Pain Symptom Manage 2017;53:880-6. [Crossref] [PubMed]
- Molassiotis A, Farrell C, Bourne K, et al. An exploratory study to clarify the cluster of symptoms predictive of chemotherapy-related nausea using random forest modeling. J Pain Symptom Manage 2012;44:692-703. [Crossref] [PubMed]
- Phligbua W, Pongthavornkamol K, Knobl T, et al. Symptom cluster and quality of life in women with breast cancer receiving adjuvant chemotherapy. Pac Rim Int J Nurs Res 2013;17:249-66.
- Kim E, Jahan T, Aouizerat B, et al. Changes in symptom clusters in patients undergoing radiation therapy. Support Care Cancer 2009;17:1383-91. [Crossref] [PubMed]