
Retroperitoneal emphysema caused by a renal abscess: a case report
Introduction
Renal and perinephric abscesses are uncommon but severe lesions caused predominantly by urinary tract infections (1,2). The incidence of renal and perinephric abscesses ranges from 1 to 10 cases per 100,000 hospitalizations (3). Ten percent of all renal cortical abscesses rupture through the renal capsule, forming a perinephric abscess (3). Retroperitoneal emphysema is a pathological situation with an abnormal amount of air in the retroperitoneal tissue (4). The most common causes of this condition are surgical complications (5). We report a case of retroperitoneal emphysema caused by a renal abscess. We present the following case in accordance with the CARE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-21-524/rc) (6).
Case presentation
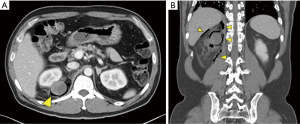
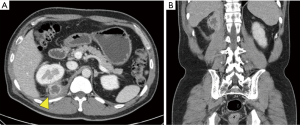
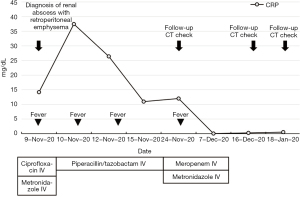
A 45-year-old man visited the emergency department with right flank pain and fever. He was under medication for type 2 diabetes mellitus (DM) since 7 months ago. He was diagnosed with myocardial infarction by coronary angiography, which was treated with percutaneous coronary intervention 10 years previously. In addition, he was diagnosed with rotator cuff tear of the right shoulder 7 months ago, which was when the type 2 DM was detected. At the time of admission, his blood pressure was 100/60 mmHg, heart rate was 86 beats/min, respiratory rate was 20 breaths/min, and body temperature was 38.0 °C. The abdomen was soft, and bowel sounds were normoactive. Right costovertebral tenderness in the ipsilateral flank was noted. On the day of admission, his laboratory results were as follows: white blood cell count, 13,000/μL (4,000–8,000/μL); hemoglobin, 14.1 g/dL (12–18 g/dL); blood urea nitrogen, 17.0 mg/dL (8–23 mg/dL); serum creatinine, 0.71 mg/dL (0.5–1.3 mg/dL); C-reactive protein, 37.45 mg/dL (0–0.3 mg/dL); lactate, 1.88 mmol/L (0.5–2.2 mmol/L); and procalcitonin, 6.21 ng/mL (0–0.5 ng/mL). The fasting and postprandial glucose levels were 125 and 195 mg/dL, respectively. Hemoglobin A1c level was 9.2%. Urinalysis showed pyuria and glucosuria. Urine culture was positive for Streptococcus agalactiae. A computed tomography (CT) scan of the abdomen showed a focal, low-attenuation lesion in the right kidney with a 3-cm, exophytic, high-attenuation lesion in the right kidney upper pole and gas-containing fluid collection within the retroperitoneal space (Figure 1). The diagnosis was retroperitoneal emphysema caused by a renal abscess. The radiological classification was type 2 (renal or perirenal fluid accompanied by a bubbly gas pattern or gas in the collecting system) and class 3a (extension of gas or abscess to the perinephric space). A day before hospitalization, intravascular ciprofloxacin and metronidazole were administered at a private clinic. We changed the treatment to intravascular piperacillin-tazobactam. We also considered performing puncture, but the patient refused. Since the patient’s vital sign was stable and the pathogen was identified through the urine culture, we decided only to follow-up the patient while on antibiotics. The patient developed a fever again after 14 days of hospitalization. Since the follow-up CT showed improved retroperitoneal emphysema and renal abscess, we changed the antibiotics to intravascular meropenem and intravascular metronidazole instead of considering surgical treatment. After 2 weeks of antibiotic use, the patient showed clinical improvement and was discharged. Two weeks after discharge, the follow-up CT showed that the renal abscess had decreased (Figure S1). We decided to conduct the follow-up using CT scans without additional antibiotic therapy. A month later, the follow-up CT confirmed that renal abscess had decreased from 3 to 2.5 cm, and the retroperitoneal emphysema was completely resolved (Figure 2). The timeline of patient’s clinical course is detailed in Figure 3. The patient has doing well without any complications during the 6-momth follow-up period, so we plan to take a follow-up CT after 1 year.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
We present a case of retroperitoneal emphysema caused by a renal abscess. The patient was treated with antibiotics alone and cured successfully. More than 75% of renal and perinephric abscesses arise from urinary tract infections (7). The kidneys are surrounded by a layer of perirenal fat that is in turn surrounded by the renal fascia (8). It is rare for a renal abscess to penetrate the renal fascia and progress to posterior paranephric emphysema.
The predisposing factors of renal and perinephric abscesses are previous urinary tract infections, renal or ureteric calculi, DM, and chronic kidney disease (9,10). The most common organisms in renal and perinephric abscesses are Escherichia coli, Proteus species, and Klebsiella species (7). As the symptoms of renal and perinephric abscess are non-specific, careful history-taking and physical examination are essential. Fever with chills and general weakness are common symptoms. Flank pain and abdominal pain are also common, and pain may be referred to the groin or leg (7,9). Renal ultrasonography and CT scan are the diagnostic methods of choice (11).
Up to 95% of the emphysematous pyelonephritis cases have underlying DM (12,13). If patients have underlying DM and complaints of fever or flank pain, early diagnosis is needed to evaluate emphysematous pyelonephritis. The choice of antibiotics should consider the local sensitivity patterns of the infecting organism. Fluoroquinolone is one of the empirical choices, but when local resistance to fluoroquinolone is high or the patient is severely ill, agents such as piperacillin-tazobactam, ceftolozane-tazobactam, and imipenem may also be considered (14,15). Renal abscesses and emphysemas often require not only antibiotics but also percutaneous drainage or surgery (16). For localized emphysematous pyelonephritis, percutaneous drainage combined with antibiotics can provide better outcome. Patients with emphysematous or xanthogranulomatous pyelonephritis may require surgical excision, and nephrectomy is also commonly performed (17). Our patient improved with only antibiotic treatment due to rapid diagnosis and proper antibiotics treatment.
In conclusion, retroperitoneal emphysema is a rare complication of a renal abscess. Owing to non-specific signs and symptoms, the diagnosis may be delayed. We suggest that if patients have underlying DM, complaints of fever or flank pain, and sustained symptoms after initiation of antibiotic therapy, careful physical examination and imaging diagnostic tests are important. Proper antibiotic treatment is needed, and percutaneous drainage or urgent surgery would be beneficial depending on the patient’s condition.
Acknowledgments
Funding: This study was supported by a grant (BCRI20025&20076) from the Chonnam National University Hospital Biomedical Research Institute.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-21-524/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-21-524/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Trabelsi N, Horchani A, Boujnah H, et al. Abscess of the kidney. Apropos of 21 cases. J Urol (Paris) 1988;94:193-8. [PubMed]
- Rubilotta E, Balzarro M, Lacola V, et al. Current clinical management of renal and perinephric abscesses: a literature review. Urologia 2014;81:144-7. [Crossref] [PubMed]
- Dembry LM, Andriole VT. Renal and perirenal abscesses. Infect Dis Clin North Am 1997;11:663-80. [Crossref] [PubMed]
- Vowinkel T, Senninger N. Retroperitoneal emphysema after endoscopic retrograde cholangiopancreatography. Chirurg 2015;86:462-7. [Crossref] [PubMed]
- Petros JG, Thanikachalam M, Lopez MJ. Retroperitoneal and abdominal wall emphysema after transanal excision of a rectal carcinoma. Am Surg 1996;62:759-61. [PubMed]
- Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. J Med Case Rep 2013;7:223. [Crossref] [PubMed]
- Jameson JL, Fauci AS, Kasper DL, et al. Harrisons Principles of Internal Medicine. 20th Ed. Available online: https://accessmedicine.mhmedical.com/book.aspx?bookID=2129
- Netter FH. Atlas of Human Anatomy Including Student Consult Interactive Ancillaries and Guides. 6th Ed. Philadelphia: Saunders, 2014.
- Rai RS, Karan SC, Kayastha A. Renal and Perinephric Abscesses Revisited. Med J Armed Forces India 2007;63:223-5. [Crossref] [PubMed]
- Yen DH, Hu SC, Tsai J, et al. Renal abscess: early diagnosis and treatment. Am J Emerg Med 1999;17:192-7. [Crossref] [PubMed]
- Gardiner RA, Gwynne RA, Roberts SA. Perinephric abscess. BJU Int 2011;107:20-3. [Crossref] [PubMed]
- Ubee SS, McGlynn L, Fordham M. Emphysematous pyelonephritis. BJU Int 2011;107:1474-8. [Crossref] [PubMed]
- Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med 2000;160:797-805. [Crossref] [PubMed]
- Stapleton A. Urinary tract infections in patients with diabetes. Am J Med 2002;113:80S-84S. [Crossref] [PubMed]
- Schneeberger C, Holleman F, Geerlings SE. Febrile urinary tract infections: pyelonephritis and urosepsis. Curr Opin Infect Dis 2016;29:80-5. [Crossref] [PubMed]
- Gerzof SG. Percutaneous drainage of renal and perinephric abscess. Urol Radiol 1981;2:171-9. [Crossref] [PubMed]
- Patel NP, Lavengood RW, Fernandes M, et al. Gas-forming infections in genitourinary tract. Urology 1992;39:341-5. [Crossref] [PubMed]


