A systematic review and meta-analysis examining the benefits of quantitative exercise intervention on effective bowel preparation prior to colonoscopy
Introduction
Colonoscopy is currently the gold standard procedure for the diagnosis and screening of colon lesions and colon cancer. The accuracy and success of colonoscopy diagnosis, as well as the safety of the procedure, largely depend on the quality of bowel preparation (1,2). Insufficient preparation of the bowel may lead to missed diagnosis of bowel tumors or precancerous lesions, increase the time and difficulty of the examination, and patients may require repeat examinations which can increase their pain and economic burden (3). Therefore, the quality of bowel preparation prior to a colonoscopy is crucial. However, approximately 20–40% of patients receiving a colonoscopy have poor bowel preparation (4,5) and falls short of the 90% readiness rate stipulated by the European Society of Gastrointestinal Endoscopy (ESGE) (6).
Inadequate bowel preparation can result in a large amount of residual stool in the intestinal cavity which can obstruct the view through the colonoscope, leading to missed diagnosis of colon cancers and precancerous lesions. Furthermore, serious complications such as intestinal perforation and intestinal bleeding may occur (7). Because quantitative exercise can promote intestinal peristalsis, which is conducive to the removal of intestinal contents. During the colonoscopy, there is no residual stool, the visual field is clear, and the intestinal wall and intestinal cavity are clearly visible, which is considered to be adequate intestinal preparation. Previous studies have suggested that exercise can promote gastrointestinal emptying by enhancing gastrointestinal peristalsis, which can clean the gastrointestinal tract (8,9). Indeed, the role of exercise has been well documented in numerous medical fields (10-13). In recent years, some studies have suggested the use of exercise to intervene in the bowel preparation of colonoscopy patients with good results (10). Although quantitative exercise has been widely used clinically, however, the efficacy of exercise on bowel preparation remains controversial (11-13).
To the best of our knowledge, this meta-analysis can provide more medical evidence to evaluate the effects of quantitative exercise on bowel preparation in colonoscopy patients. We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/apm-21-3378).
Methods
Search strategy
Randomized controlled trials (RCTs) and clinical controlled trials (CCTs) that quantified the effects of exercise intervention on colonoscopy bowel preparation were identified through database searches using the Cochrane Library, JBI evidence-based database, Embase, Web of Science, CINAHL, Medline, CNKI, China Biomedical Literature Database (CBM), and the Wanfang database. Literatures published in Chinese or English from the establishment of the database until July 2021 were included. The search strategy combined subject terms, titles, and keywords. The search terms were as follows: “bowel preparation” OR “bowel cleansing” OR “colonoscopy” OR “preparation, bowel” OR “cleansing, bowel” AND “exercise” OR “physical activity” OR “walking”.
Inclusion criteria
RCTs or comparative studies of CCTs published in Chinese or English were considered. Studies were included if the following inclusion criteria were satisfied: (I) all included research subjects underwent colonoscopy; (II) participants in the control group were only given routine care; (III) patients in the intervention group received routine care and walking exercise intervention quantified by exercise time and frequency; and (IV) clear outcome indicators, including the efficiency of intestinal cleansing and the incidence of adverse events such as nausea, vomiting, and abdominal pain, were reported.
Exclusion criteria
The following literatures were excluded: (I) duplicate articles; (II) studies with incomplete data which cannot be extracted; (III) reviews, expert opinions, and letters; (IV) studies which did not assess the quality of bowel preparation; (V) studies which did not report adverse events such as nausea, vomiting, and abdominal pain; and (VI) articles which did not specify the randomized control design of the study.
Literature screening and data extraction
Two researchers independently screened the literature via reviewing the title, followed by reading the abstract and full text article, and finally, assessing it against the inclusion criteria. Any disagreements were resolved via discussion or consultation with a third researcher. Article authors were contacted to supplement any missing data and information. The following data were collated: (I) the first author and year of publication; (II) the type of study; (III) the number of patients in each study group; (IV) the intervention for each group; and (V) the outcome indicators (including bowel preparation quality and adverse reactions). The quality of bowel preparation was recorded as the number of qualified bowel preparation cases/total number of bowel preparation cases in each group. Adverse reactions were recorded as the number of adverse reactions in each group/total number of bowel preparations.
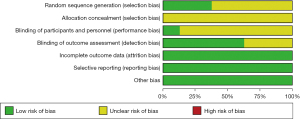
Risk of bias
The Cochrane Handbook 5.1.0 bias risk assessment tool was used to evaluate the bias risk in the RCTs. There were 7 assessment items, including random sequence generation, allocation hiding, blinding of participants and personnel, blinding of outcome evaluation, incomplete outcome data, selective reports, and other sources of bias. Each area was assessed as low, high, or unclear risk of bias. Research bias was classified as “unclear”, “low risk”, or “high risk”. Any disagreements were resolved via consultation with a third investigator.
Statistical analysis
Meta-analysis of the included data was performed using the RevMan 5.3 software. For binary variables, relative risk (RR) values or mean difference (MD) values and the 95% confidence intervals (CI) were selected as the effect analysis statistics with the test level set to α=0.05. The χ2 test was used to explore heterogeneity among studies. If P≥0.05 and I2<50%, the included studies were considered homogeneous and a fixed effects model was adopted. If P<0.05 and I2≥50%, there was heterogeneity among the studies and the random effects model was used and sensitivity analysis was performed. If P≤0.05 and the source of heterogeneity could not be determined, a descriptive analysis was performed.
Results
Search results and study characteristics
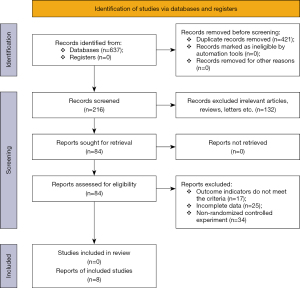
The database search identified 637 articles, including 317 articles in Chinese and 320 articles in English. After excluding duplicate articles, a total of 216 articles were obtained. After strict layer by layer screening, 8 studies were finally included, with a total of 1,486 patients, including 747 in the intervention group and 739 in the control group. The literature screening process is shown in Figure 1.
The included literatures mainly originated from China, Korea, and the United States. All studies reported the comparative analysis of the joint intervention of quantitative exercise and routine care. The basic characteristics of the included studies are detailed in Table 1.
Table 1
| Author | Country | Year | Journal | Intervention (n) | Control (n) |
|---|---|---|---|---|---|
| Zhang et al. (13) | China | 2017 | Journal of Nursing Administration | 110 | 110 |
| Chen et al. (14) | China | 2017 | China Medicine and Pharmacy | 124 | 124 |
| Chen et al. (15) | China | 2018 | Anhui Medical Journal | 60 | 60 |
| Kim et al. (11) | Korea | 2005 | American Journal of Gastroenterology | 182 | 174 |
| Fang et al. (12) | China | 2017 | Journal of Colorectal & Anal Surgery | 34 | 34 |
| Noh et al. (16) | Korea | 2020 | Gut and Liver | 100 | 100 |
| Arya et al. (17) | America | 2010 | The Journal of Alternative and Complementary Medicine | 27 | 27 |
| Qin et al. (18) | China | 2016 | Therapeutics and Clinical Risk Management | 110 | 110 |
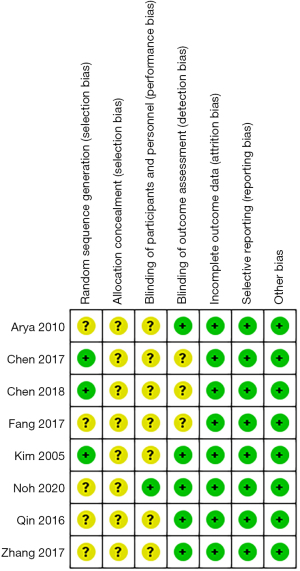
The risk of bias in each study was assessed using the Cochrane Collaboration’s risk of bias assessment tool (Figure 2). Three trials reported the generation of random sequences in detail, and the generation of random sequences in seven trials was unclear. Due to the characteristics of the intervention, it is impractical to hide the allocation and the blinding of the participants and researchers. Therefore, only one article clearly reported the blinding of the patients and researchers. Five articles were blinded for outcome evaluation, while the other three were unclear. All the included studies had a low risk of bias in selective reporting and there was no missing data. The risk of other biases is considered non-existent.
Meta-analysis results
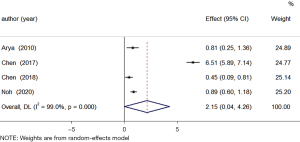
Bowel cleansing quality
All included studies compared the effects of quantitative walking exercises and conventional nursing interventions and individual conventional nursing interventions on the quality of bowel cleansing. A total of 622 subjects were included. The heterogeneity test showed that the included studies were heterogeneous and the random effects model was used for meta-analysis. There was significant difference in the quality of bowel cleansing between the quantitative exercise intervention group and patients in the control group (MD =2.15; 95% CI: 0.04 to 4.26; Z=1.999; P=0.046; Figure 3).
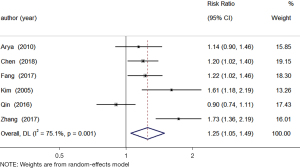
Adequacy rate of bowel preparation
A total of 1,038 subjects were assessed for adequacy of bowel preparation. The studies were heterogeneous and the random effects model was used. Meta-analysis revealed that the quantitative exercise intervention group had a significantly higher rate of adequate bowel preparation compared to the control group (RR =1.25, 95% CI: 1.05 to 1.49; Z=2.527; P=0.012; Figure 4).
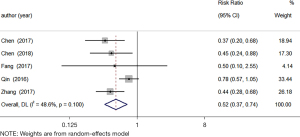
Incidence of nausea
A total of 876 patients were included in the nausea-related study. The heterogeneity test showed that the included studies were heterogeneous and the random effects model was used. Meta-analysis demonstrated that the quantitative exercise intervention group had a significantly lower incidence of nausea after bowel preparation compared to the control group (RR =0.52; 95% CI: 0.37 to 0.74; Z=−3.681; P=0.000; Figure 5).
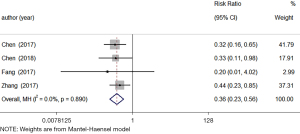
Incidence of vomiting
The incidence of vomiting related to the bowel preparation was assessed in 656 patients. The included studies were homogeneous and the fixed effects model was used for meta-analysis. The incidence of vomiting after bowel preparation was significantly lower in the quantitative exercise intervention group compared to the control group (RR =0.36; 95% CI: 0.23 to 0.56; Z=−4.593; P=0.000; Figure 6).
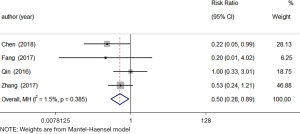
Incidence of abdominal pain
A total of 628 patients were included in the study examining bowel preparation and abdominal pain. The heterogeneity test revealed that the included studies were homogeneous and the fixed effects model was used. Meta-analysis showed that the quantitative exercise intervention group had a significantly lower incidence of abdominal pain after bowel preparation compared to the control group (RR =0.50; 95% CI: 0.28 to 0.89; Z=−2.349; P=0.019; Figure 7).
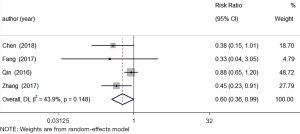
Incidence of bloating
A total of 628 patients were included in the study investigating bowel preparation and bloating. The heterogeneity test revealed that the data were heterogeneous and the random effects model was used for meta-analysis. The quantitative exercise intervention group and the control group had comparable rates of abdominal distension after bowel preparation, and there was statistical difference (RR =0.60; 95% CI: 0.36 to 0.99; Z=−1.989; P=0.047; Figure 8).
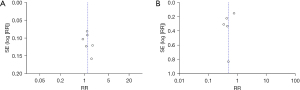
Publication bias
The funnel plot was used to detect the publication bias of the adequacy rate of bowel preparation and the vomiting rate after bowel preparation. Visual observations based on the funnel plot showed asymmetry, indicating that both may have publication bias (Figure 9).
Risk of bias
Among the eligible studies, 3 articles described the random sequence generation as low risk (11,14,15), 5 articles described the random sequence generation as unclear (12,13,16-18), all studies had unclear allocation hidden bias, and 1 trial had a low risk of bias for blinding participants and researchers (16). A total of 5 trials described the risk of bias in blinded results assessment as low risk (11,13,16-18). All trials had low risk of bias for incomplete outcome data, selective reporting domains, and other bias (Figure 10).
Discussion
This systematic review and meta-analysis examined the impact of quantitative exercise intervention on bowel preparation for colonoscopy patients, with the aim of using quantitative exercise as a reference in bowel preparation and in other fields of medicine.
The results of this meta-analysis, combined with the conclusions of the included studies, showed that quantitative exercise can increase the rate of adequate bowel preparation and reduce the incidence of adverse reactions. Indeed, studies have shown that the quality of bowel preparation is positively correlated to the walking time during medication (8,11,13). It is speculated that exercise can promote the secretion of the digestive glands and the movement of the digestive tract, and accelerate gastrointestinal emptying, thereby improving the cleanliness of the bowel (2,4,19).
At present, most patients use laxatives to promote intestinal cleansing prior to colonoscopy, and this is prone to poor tolerance, as well as nausea, vomiting, and other adverse reactions. Indeed, 19.7% of patients will experience abdominal pain and 16.4% of patients will experience vomiting (6,20). These adverse reactions will significantly reduce the quality of bowel preparation and lead to inaccurate colonoscopy results (16,21). The current meta-analysis revealed that quantitative exercise intervention can reduce the incidence of nausea, vomiting, and abdominal pain. Reasonable exercise can promote blood circulation in the intestinal tract, stimulate the movement of the digestive tract, and accelerate the absorption and excretion of intestinal contents, thereby reducing the adverse side effects such as abdominal pain and vomiting. However, the current quantitative exercise standards differ in each center, including exercise time and intensity, and are affected by the patient’s ability to withstand, and further unified standards are needed.
There were some limitations to this study. First, the number of research articles and the sample sizes included were relatively small, which may reduce the reliability of this research results to a certain extent. Second, most of the included studies had an obvious risk of bias in allocation hiding and blinding of the participants and researchers. Some articles did not incorporate random sequence generation and result evaluation blinding methods, which may also lead to certain bias. Finally, most of the publications originated from a single country and this may have caused certain limitations to this study. Future multi-centered, large sample, randomized controlled studies quantifying the impact of exercise intervention on the quality of bowel preparation and related factors should be performed to verify these results. Furthermore, the methods for monitoring exercise should be standardized to draw more accurate and reliable conclusions.
Conclusions
In summary, this meta-analysis provided evidence that quantitative exercise intervention plays an important role in bowel preparation for colonoscopy by effectively improving the bowel cleansing quality and adequacy rate, and reducing the incidence of nausea, vomiting, abdominal pain, and incidence of bloating. However, as this meta-analysis was based on a limited number of high-quality studies, further clinical multi-centered and large-scale RCTs are warranted to verify these conclusions.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-3378
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-3378). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- ASGE Standards of Practice Committee. Bowel preparation before colonoscopy. Gastrointest Endosc 2015;81:781-94. [Crossref] [PubMed]
- Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2012;143:844-57. [Crossref] [PubMed]
- Johnson DA, Barkun AN, Cohen LB, et al. Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the US multi-society task force on colorectal cancer. Gastroenterology 2014;147:903-24. [Crossref] [PubMed]
- Mahmood S, Farooqui SM, Madhoun MF. Predictors of inadequate bowel preparation for colonoscopy: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 2018;30:819-26. [Crossref] [PubMed]
- Serper M, Gawron AJ, Smith SG, et al. Patient factors that affect quality of colonoscopy preparation. Clin Gastroenterol Hepatol 2014;12:451-7. [Crossref] [PubMed]
- Rembacken B, Hassan C, Riemann JF, et al. Quality in screening colonoscopy: position statement of the European Society of Gastrointestinal Endoscopy (ESGE). Endoscopy 2012;44:957-68. [Crossref] [PubMed]
- Chokshi RV, Hovis CE, Hollander T, et al. Prevalence of missed adenomas in patients with inadequate bowel preparation on screening colonoscopy. Gastrointest Endosc 2012;75:1197-203. [Crossref] [PubMed]
- He LI, Wei WR, Can Z. Effects of 12-week brisk walking training on exercise blood pressure in elderly patients with essential hypertension: a pilot study. Clin Exp Hypertens 2018;40:673-9. [Crossref] [PubMed]
- McDermott MM, Liu K, Guralnik JM, et al. Home-based walking exercise intervention in peripheral artery disease: a randomized clinical trial. JAMA 2013;310:57-65. [Crossref] [PubMed]
- Kim YS, Song BK, Oh JS, et al. Aerobic exercise improves gastrointestinal motility in psychiatric inpatients. World J Gastroenterol 2014;20:10577-84. [Crossref] [PubMed]
- Kim HS, Park DH, Kim JW, et al. Effectiveness of walking exercise as a bowel preparation for colonoscopy: a randomized controlled trial. Am J Gastroenterol 2005;100:1964-9. [Crossref] [PubMed]
- Fang H. The effect of different intestinal cleaning and exercise programs in colonoscopy bowel preparation. Journal of Colorectal & Anal Surgery 2017;23:618-21.
- Zhang Y, Niu M, Wang Q, et al. An application of quantified exercise intervention plan in patients while colonoscopy. Journal of Nursing Administration 2017;17:58-60.
- Chen B, Tao Y, Liu X, et al. Effect of quantifying exercise on bowel preparation in patients undergoing colonoscopy. China Medicine and Pharmacy 2017;7:150-2.
- Chen F, Luo M, Lin F, et al. Application of sports bracelet in bowel preparation for colonoscopy in the elderly. Anhui Medical Journal 2018;39:889-92.
- Noh CK, Kim IS, Lee GH, et al. Comparison of Effectiveness between Abdominal Vibration Stimulation and Walking Exercise for Bowel Cleansing before Therapeutic Colonoscopy. Gut Liver 2020;14:468-76. [Crossref] [PubMed]
- Arya V, Gupta KA, Arya SV. Efficacy of bolus lukewarm saline and yoga postures as colonoscopy preparation: a pilot study. J Altern Complement Med 2010;16:1269-77. [Crossref] [PubMed]
- Qin Y, Liu W, Lin S, et al. Effects of first-dose volume and exercise on the efficacy and tolerability of bowel preparations for colonoscopy in Chinese people. Ther Clin Risk Manag 2016;12:613-6. [PubMed]
- Horner KM, Schubert MM, Desbrow B, et al. Acute exercise and gastric emptying: a meta-analysis and implications for appetite control. Sports Med 2015;45:659-78. [Crossref] [PubMed]
- Chan WK, Azmi N, Mahadeva S, et al. Split-dose vs same-day reduced-volume polyethylene glycol electrolyte lavage solution for morning colonoscopy. World J Gastroenterol 2014;20:14488-94. [Crossref] [PubMed]
- Fang J, Fu HY, Ma D, et al. Constipation, fiber intake and non-compliance contribute to inadequate colonoscopy bowel preparation: a prospective cohort study. J Dig Dis 2016;17:458-63. [Crossref] [PubMed]
(English Language Editor: J. Teoh)