
Correlation between C-reactive protein/albumin and contralateral hip refracture after total hip arthroplasty in elderly patients with hip fractures
Introduction
Despite recent improvements in the one-year survival rates of hip fracture patients after hip replacement and the ability of most patients to recover to their pre-fracture state, the risk of post-surgery hip refracture remains high (1,2). After 1 year, the mortality rate among elderly hip fracture patients with contralateral hip refracture after total hip arthroplasty (THA) is 24.1% (3). C-reactive protein (CRP) is the main inflammatory marker, and it has been used in the prognostic evaluation of many diseases such as orthopedic infections and trauma. Related studies have found that abnormal changes in CRP levels and hip replacement in patients with hip fractures poor prognosis is related (4). Serum albumin levels reflect the nutritional status of patients. Preoperative serum albumin (Alb) expression has been shown to be associated with many postoperative complications (5), and studies have found that hip replacement surgery in elderly hip fracture patients post-adverse prognosis is significantly associated with preoperative serum albumin levels (6). However, the application of the ratio of serum CRP to Alb in hip fracture hip replacement is rare, especially whether the ratio between the two is related to the recurrence of the contralateral hip after operation in elderly hip fracture patients, and there are not many relevant studies. This study focused on the observation of CRP/Alb expression in contralateral hip re-fractures in elderly hip fracture patients after total hip replacement. The aim is to explore the correlation between CRP/Alb expression and contralateral hip re-fractures in patients. The report is as follows.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-855).
Methods
Subjects
The medical records of elderly hip fracture patients who received THA at our hospital between July 2017 and July 2019 were reviewed. The inclusion criteria were as follows: (I) complete medical records and follow-up data available; (II) new, Garden grade III–IV unilateral femoral neck fracture; (III) >60 years old; (IV) non-high-energy traumatic hip fractures caused by walking injuries, sprains, or misstep injuries; (V) total hip replacement surgery performed by the same group of anesthesiologists and chief surgeons; and (VI) normal cognitive function throughout the perioperative and follow-up periods. Patients who met any of the following criteria were excluded: (I) pathological fractures caused by bone tumors or bone cysts; (II) had received conservative treatment; (III) history of hip fractures; (IV) previous contralateral hip surgery; and (V) incomplete follow-up data.
General information
A total of 224 elderly hip fracture patients (105 males and 119 females) who underwent THA were enrolled. The patients had a mean age of 71.12±6.0 [60–85] years old. The mean duration between fracture and surgery was 4.02±1.61 [1–7] days. All patient data were collated and reviewed after informed consent was obtained from the patients. The study complied with the relevant medical ethics regulations.
Study methods
Grouping
All patients were followed up for a period of 1 year after THA. In the event of a patient experiencing a new trauma or fracture-related symptoms during this period, they were admitted to the hospital to undergo imaging tests and consultation. The patients with or without confirmed contralateral hip fracture were assigned to the refracture group and the control group, respectively.
Baseline data collection
Preoperative baseline data was collected using a questionnaire which took into account variables such as gender, age, fracture classification, time from fracture to surgery, and comorbidities (e.g., diabetes, hypertension, heart disease, chronic lung disease, or systemic diseases). Surgical information including operation time, anesthesia classification, and intraoperative blood loss was also recorded.
Laboratory tests
After fasting overnight, peripheral blood (5 mL) was collected from the basilic vein of the patients, and routine hematological indices, including white blood cell, platelet, and red blood cell counts and hemoglobin levels, were measured using an automated blood analyzer. The blood samples were centrifuged at 3,000 rpm for 15 minutes to collect serum. Subsequently, serum CRP and Alb levels were measured using the specific ELISA kits (Shenzhen Jingmei Biotech Co. Ltd., China), and the CRP/Alb ratio was calculated.
Statistical analysis
Data were processed using SPSS20.0 statistical software [IBM Corporation (SPSS Co.)] and tested for normal distribution. The normally distributed measurable data were expressed as x±s and compared using the independent samples t-test. Count data were expressed as percentages and compared using the χ2 test. Binary Logistic regression analysis was used to test the effect of CRP/Alb on contralateral hip re-fracture after total hip replacement. The area under the receiver operating characteristic (ROC) curve was calculated to assess the predictive value of CRP/Alb. Statistical significance was indicated when P<0.05.
Results
Incidence of refracture
Of the 224 elderly hip fracture patients who underwent THA, only 20 (8.93%) experienced contralateral hip refracture.
Comparison of baseline data between the refracture and control groups
There were no significant differences in gender, age, time from fracture to surgery, fracture classification, comorbidities, surgical conditions, white blood cell count, platelet count, red blood cell count, hemoglobin, and bone density between the refracture and control groups (P>0.05; Table 1).
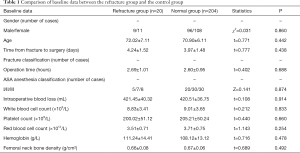
Full table
Preoperative serum CRP and Alb levels, and CRP/Alb ratio differed between the two groups
The refracture group had significantly higher preoperative serum CRP levels, lower Alb levels, and a higher CRP/Alb ratio compared to the controls (P<0.05; Table 2).

Full table
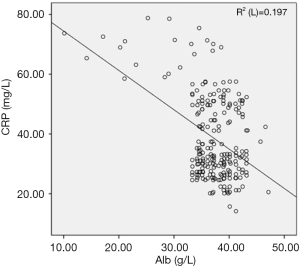
Preoperative serum CRP and Alb levels were negatively correlated in the elderly patients with hip refracture
Pearson’s correlation coefficient demonstrated that serum CRP level was negatively correlated with Alb level in the elderly hip fracture patients (r=−0.443, P<0.001). The correlation scatterplot is shown in Figure 1.
Linear binary logistic regression analysis of the effect of pre-operative CRP/Alb ratio on contralateral hip re-fracture in elderly hip fractures
The preoperative CRP/Alb ratio was used as a covariate, and the recurrence of contralateral hip fracture in elderly hip fracture patients was used as the dependent variable (1 = occurred, 0 = not occurred). The results of binary logistic regression analysis showed that high CRP/Alb ratio may be a risk factor for contralateral hip re-fracture after total hip replacement in elderly hip fracture patients (P<0.05; Table 3).

Full table
Preoperative CRP/Alb ratio has a high predictive value for contralateral hip refracture in elderly hip fracture patients
A ROC curve was plotted with incidence of post-THA hip refracture as the state variable. The area under the curve for the CRP/Alb ratio was 0.841 (95% CI: 0.702–0.914), and the optimal cutoff value was 1.12. The corresponding specificity and sensitivity were 0.782 and 0.945, respectively, and the Youden index was 0.727 (Figure 2); thus, preoperative CRP/Alb has high predictive ability for post-THA refracture.

Discussion
Older patients carry a higher risk of contralateral hip refracture following hip arthroplasty due to bone loss. Besalduch et al. (7) reported an incidence of 10.8% for post-surgery contralateral hip fractures in the elderly population, which is close to the 8.4% observed in a similar Chinese study (8). The incidence of post-THA contralateral hip refracture in our cohort was 8.93%, which is consistent with these findings. Because of the increased risk of death for patients with post-surgery contralateral hip fracture, it is vital that the causative and predictive factors with relatively high specificity and sensitivity are identified, so that refracture can be prevented and treated early (9,10). Despite the results of previous studies showing satisfactory prediction of the risk of post-surgery contralateral hip refracture through acute physiological and chronic health evaluation systems, surgical severity, physiological ability, and surgical invasiveness scores (11,12), the complexity and diversity of these indices often limit their application in a clinical setting, especially in primary hospitals. Therefore, a simpler and more effective laboratory-based indicator is urgently needed to predict and evaluate this risk.
Studies have revealed that the concurrence of a fracture and trauma or infection is closely associated with the severity of the fracture. CRP, a reliable marker of trauma/infection-related inflammation, is an important indicator of orthopedic infection following surgery (13,14). A recent study showed that an elevated level of preoperative CRP is a primary risk factor of post-THA death in older patients with hip fractures (15), indicating that it may also be associated with increased incidence of post-surgery contralateral hip refracture. Serum Alb is an important indicator of protein/energy consumption and is routinely used to evaluate perioperative nutritional status (16). As a standard laboratory test, several studies have used serum Alb detection as a prognostic indicator in elderly patients with hip fractures. Low perioperative serum Alb level is a major factor affecting the length of hospital stay, recovery of normal activities, and the risk of postoperative death among such patients; this is evidenced by the correlation between poor nutritional status during the perioperative period and slower postoperative recovery (17,18). Thus, low serum Alb level is also a factor potentially related to the incidence of post-surgery contralateral hip refractures.
As indicators of the immunological and nutritional status respectively, CRP and Alb levels have limited clinical utility when applied separately. In fact, the ratio of CRP to Alb is more accurate as an indicator of both inflammatory and nutritional status compared to either index (19,20). Because the level of perioperative or postoperative detection may be affected by the operation itself or medication during the perioperative period, this study mainly observes the impact of the preoperative CRP/Alb on patients, and has ensured the credibility of the results. The results of this study showed that compared with the normal group, the patients in the contralateral hip re-fracture group had higher preoperative blood CRP levels, lower Alb levels, and higher CRP/Alb ratio, and the contralateral hip re-fracture group patients showed higher CRP and Alb levels. Negative correlation, that was, with the increase of CRP, the Alb of the patient decreased. It was speculated that the increase in systemic inflammatory response before surgery may be the cause of poor nutritional status. As the nutritional status continued to deteriorate, the systemic inflammatory response also increased, both Interactions were causal to each other and therefore affect the prognosis. Linear regression analysis indicated that the CRP/Alb ratio is a potential risk factor for post-THA contralateral hip refracture in elderly hip fracture patients, and its high predictive value was confirmed by ROC curve analysis. Altogether, these findings suggest that preoperative serum CRP and Alb levels, and the CRP/Alb ratio can predict the risk of post-surgery contralateral hip refracture in older people, this risk can be reduced by nutritional fortification and attenuation of systemic inflammatory response before surgery. However, this study also has certain limitations. First, the study was a retrospective single-center study with limited medical record data, especially the small sample size of the contralateral hip re-fracture group. Second, the study did not fully consider other factors. The possible impact and the results obtained may deviate from the actual. These limitations should also be verified by prospective, large sample and long-term research in the future.
In summary, serum CRP level is correlated with Alb level in elderly hip fracture patients, and the CRP/Alb ratio is a risk factor for post-THA contralateral hip refracture. Therefore, to predict the risk of post-THA contralateral hip refracture, the preoperative serum CRP/Alb ratio should be measured in elderly hip fracture patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-855
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-855
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-855). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All patient data were collated and reviewed after informed consent was obtained from the patients. The study complied with the relevant medical ethics regulations. The Affiliated Hospital of North Sichuan Medical College [2017ER (A) 034].
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Thien TM, Chatziagorou G, Garellick G, et al. Periprosthetic femoral fracture within two years after total hip replacement: analysis of 437,629 operations in the nordic arthroplasty register association database. J Bone Joint Surg Am 2014;96:e167. [Crossref] [PubMed]
- Zhou XF, Zhang BZ, Weng XS, et al. Treating strategy of second hip fractures in elderly patients. Beijing Medical Journal 2017;39:138-42.
- Ouanezar H, Jalaguier T, Franck F, et al. Mid-term outcomes of titanium modular neck femoral stems in revision total hip arthroplasty. Ann Transl Med 2019;7:92. [Crossref] [PubMed]
- Kim BG, Lee YK, Park HP, et al. C-reactive protein is an independent predictor for 1-year mortality in elderly patients undergoing hip fracture surgery: A retrospective analysis. Medicine (Baltimore) 2016;95:e5152. [Crossref] [PubMed]
- Adogwa O, Martin JR, Huang K, et al. Preoperative serum albumin level as a predictor of postoperative complication after spine fusion. Spine (Phila Pa 1976) 2014;39:1513-9. [Crossref] [PubMed]
- Kieffer WK, Rennie CS, Gandhe AJ. Preoperative albumin as a predictor of one-year mortality in patients with fractured neck of femur. Ann R Coll Surg Engl 2013;95:26-8. [Crossref] [PubMed]
- Besalduch M, Carrera I, Gómez-Masdeu M, et al. Antiresorptive treatment, when initiated after a first hip fracture, may not protect of a second contralateral episode in elderly population: A study with 685 patients. Injury 2016;47:877-80. [Crossref] [PubMed]
- Tian SJ, Zhao LP, Ni SJ, et al. Influencing factors of refractures of the contralateral hip in elderly patients with hip fracture. Chinese Journal of Orthopaedic Trauma 2015;17:124-8.
- Li SG, Liu Z, Sui TS, et al. The postoperative mortality of one year after surgery for hip fracture in elderly population and risk factors analysis. Beijing Medical Journal 2015;37:16-20.
- Zhang SM, Zhao D, Wang HB. Preoperative risk prediction models for mortality and complications following hip fracture surgery in the elderly. Orthopedic Journal of China 2015;23:1869-75.
- Gao H, Wang BJ, Zhao L, et al. Quantitative analysis of operation risks for femoral intertrochanteric fractures under the guidance of Acute Physiology and Chronic Health Evaluation system. Chinese Journal of Orthopaedic Trauma 2018;20:76-9.
- Moppett I. Accuracy of POSSUM and Nottingham Hip Fracture Score. Acta Anaesthesiol Scand 2018;62:1333-4. [Crossref] [PubMed]
- Eriksson AL, Movérare-Skrtic S, Ljunggren Ö, et al. High-sensitivity CRP is an independent risk factor for all fractures and vertebral fractures in elderly men: the MrOS Sweden study. J Bone Miner Res 2014;29:418-23. [Crossref] [PubMed]
- de Oliveira VM, Moraes RB, Stein AT, et al. Accuracy of C - Reactive protein as a bacterial infection marker in critically immunosuppressed patients: A systematic review and meta-analysis. J Crit Care 2017;42:129-37. [Crossref] [PubMed]
- Kim BG, Lee YK, Park HP, et al. C-reactive protein is an independent predictor for 1-year mortality in elderly patients undergoing hip fracture surgery: A retrospective analysis. Medicine (Baltimore) 2016;95:e5152. [Crossref] [PubMed]
- Li J, Nong AH, Zhang LC, et al. Effect of pre-operative serum albumin level and total lymphocyte count on outcomes of elderly patients with hip fracture. Chinese Journal of Multiple Organ Diseases in the Elderly 2014;13:255-8.
- Kieffer WK, Rennie CS, Gandhe AJ. Preoperative albumin as a predictor of one-year mortality in patients with fractured neck of femur. Ann R Coll Surg Engl 2013;95:26-8. [Crossref] [PubMed]
- O'Daly BJ, Walsh JC, Quinlan JF, et al. Serum albumin and total lymphocyte count as predictors of outcome in hip fractures. Clin Nutr 2010;29:89-93. [Crossref] [PubMed]
- Guo S, He X, Chen Q, et al. The C-reactive protein/albumin ratio, a validated prognostic score, predicts outcome of surgical renal cell carcinoma patients. BMC Cancer 2017;17:171. [Crossref] [PubMed]
- Liang Y, Xiao W, Guan YX, et al. Prognostic value of the C-reactive protein/Albumin Ratio (CAR) in patients with operable soft tissue sarcoma. Oncotarget 2017;8:98135-47. [Crossref] [PubMed]


