
The comparison of electromagnetic with virtual bronchoscopic navigation accuracy at hybrid operating room in patient with sternal wires
Introduction
Surgical excision biopsy for small lung lesions can provide both diagnosis and curative treatment. However, these small lesions particularly when they are soft or ground glass opacities (GGO) require preoperative localization. Percutaneous and endobronchial “marking” can be performed and may be chosen depending on location and depth of lesion, as well as local expertise. Many navigation bronchoscopy systems depend on electromagnetic field for navigation and its accuracy may be affected by small volumes of ferrous material near the patient. We describe a case of a 63-year-old lady with right upper lobe GGO, who has steel sternal wires from recent coronary artery bypass surgery (CABG) undergoing hybrid operating room cone-beam CT (CBCT) image-guided electromagnetic navigation bronchoscopy (iENB) dye marking for video-assisted thoracic surgery (VATS) excisional biopsy (1). The accuracy of an electromagnetic navigation bronchoscopy (ENB) system was assessed and compared with a virtual bronchoscopic navigation system in the presence of sternal wires.
Case presentation
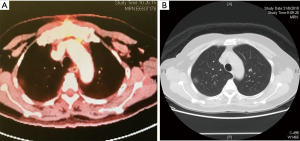
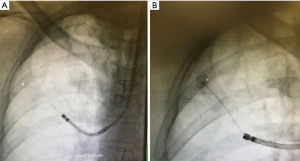
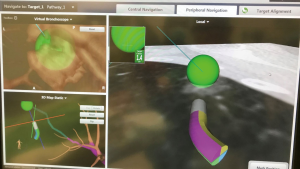
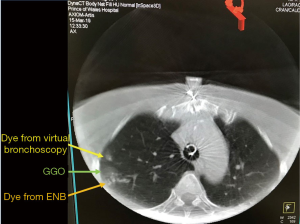
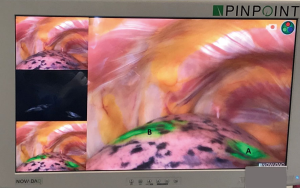
A 63-year-old lady with prior CABG for multi-vessel coronary artery disease had a persistent peripheral right upper lobe 1.4 cm × 1.5 cm GGO with a 0.35-cm central solid component (Figure 1). An 18-fluorodeoxyglucose positron emission tomography-computed tomography (PET-CT) showed mild activity and potential malignant lesion. There were no other lesions or lymph nodes suggestive of metastatic disease. Her forced expiratory volume in 1 second was 65% predicted and diffusion capacity of carbon monoxide was 61%. VATS surgical excision biopsy was planned. However, the small and soft lesion required pre-operative localization. In view of the lesion shielded by the scapula and ribs, percutaneous “marking” would be challenging. Hybrid operating room CBCT navigation bronchoscopy dye marking followed by immediate VATS resection of the lesion was performed. Due to the uncertainty of effects of steel sternal wires on electromagnetic navigation accuracy, we additionally performed virtual bronchoscopic navigation dye marking. After induction of general anaesthesia, a CBCT (Artis Zeego, Siemens, Germany) of the chest was performed and the centre of the lesion marked by i-Guide toolbox to highlight its location on subsequent real-time fluoroscopy to facilitate bronchoscopic navigation. Virtual bronchoscopic navigation (LungPoint, Broncus, USA) using a standard 3.8-mm diameter flexible bronchoscope was performed followed by peripheral navigation by 5-Fr angulated angiographic catheter (Cordis, Johnson & Johnson, USA) and 0.2 mL of triple contrast dye injection (iohexol, methylene blue, indocyanine green) (2) (Figures 2). Subsequently, ENB (Medtronic SuperDimension Version 7.0) was used with locatable guide via 90-degree Edge Extended Working Channel (EWC) to reach distance 1.4 cm from the centre of the lesion (Figure 3) and injection of 0.2 mL of triple contrast dye marking was performed using 21G Edge biopsy needle under direct fluoroscopic guidance. CBCT following both approaches were performed showing the two dye markings (Figure 4) at close proximity and bracketing the GGO lung lesion. Uniportal VATS lung resection was performed clearly showing the two markings with near infra-red light fluorescence thoracoscopy (Pinpoint, Stryker, USA) (Figure 5). Intra-operative frozen section confirmed adenocarcinoma thus a completion right upper lobectomy was performed. Pathology showed pT1a adenocarcinoma with maximum 1cm invasive acinar component and surrounding lepidic growth. There was no lymph node metastasis. The patient had unremarkable recovery and prognosis was good with timely resection of the stage IA lung cancer.
Discussion
ENB is widely gaining popularity for the management of lung cancer (1,3). Used commonly to target small peripheral lung nodules to obtain tissue diagnosis, injection of dye markers for planned lung resection, placement of fiducial markers for radiotherapy, and even utilized in conjunction with ablative catheters for lung tumors, ENB has become one of the important skill that a clinician should consider in managing lung cancer (4). With the wide application of ENB in thoracic surgery, relatively little is known about its accuracy in patients with implanted metallic materials within the thorax, especially in cases of patients with sternal wires who had undergone open cardiac surgery. Anecdotal evidence and feedback from regular users of electromagnetic navigation system suggest it is safe and feasible, but no previous reports have used real time CBCT to study its accuracy.
Several issues have to be considered when performing ENB in the hybrid theatre. The degree of electromagnetic interference within the theatre has to be calibrated prior to ensure compatibility of the hybrid operating theatre with the ENB. Usually, a designated position to place the ENB machine in relation to the CBCT and other machinery is recommended during the procedure to minimize interference (3). Metallic objects should be kept away from the navigation system so as to minimize any electromagnetic interference that may reduce navigational accuracy. Thus, non-metallic bronchoscopic holders to secure the system during CBCT scanning are used. In a review Leong et al highlighted the importance of a consistent bronchoscopy suite set-up since metal objects and mobile communications devices within 1 metre of the electromagnetic field will reduce system accuracy (5). Although many have echoed the undesirable effect of metallic objects on the accuracy of ENB navigation, none has studied in detail or used real time imaging to investigate the effects. On the other hand, the safety of ENB in patients with pacemakers and implanted cardiac defibrillator (ICD) have shown that ENB is safe as long as the electromagnetic interference levels are below the reference levels for general public exposure to time-varying electric and magnetic fields set by the International Commission on Non-ionizing Radiation Protection (ICNIRP) (6). However, this study did not establish the effect of metallic ICD on the navigation procedure and accuracy itself.
Conclusions
Our case clearly shows the high degree of navigation accuracy is achieved with ENB to precisely reach our target lung lesion in a patient with sternal wires in the chest, and confirmed by CBCT in hybrid operating room setting. In addition, we performed an alternative virtual bronchoscopic navigation as a comparison and control. Further studies may generate a more objective measure of the effect of metallic objects on electromagnetic based navigation bronchoscopy procedures.
Acknowledgments
None.
Footnote
Conflicts of Interest: CS Ng is a consultant for Medtronic, USA and Broncus. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Ng CS, Yu SC, Lau RW, et al. Hybrid DynaCT-guided electromagnetic navigational bronchoscopic biopsy†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i87-8. [PubMed]
- Ng CSH, Zhao Z, Long H, et al. Electromagnetic Navigation Bronchoscopy Triple Contrast Dye Marking for Lung Nodule Localization. Thorac Cardiovasc Surg 2019. [Epub ahead of print]. [PubMed]
- Zhao ZR, Lau RW, Ng CS. Hybrid theatre and alternative localization techniques in conventional and single-port video-assisted thoracoscopic surgery. J Thorac Dis 2016;8:S319-27. [PubMed]
- Ng CSH, He JX, Rocco G. Innovations and technologies in thoracic surgery. Eur J Cardiothorac Surg 2017;52:203-5. [Crossref] [PubMed]
- Leong S, Ju H, Marshall H, et al. Electromagnetic navigation bronchoscopy: A descriptive analysis. J Thorac Dis 2012;4:173-85. [PubMed]
- Magnani A, Matheoud R, Brambilla M, et al. In vitro tests of electromagnetic interference of electromagnetic navigational bronchoscopy to implantable cardioverter defibrillators. Europace 2012;14:1054-9. [Crossref] [PubMed]
Cite this article as: Fernandez RAS, Yu PSY, Chan JWY, Lim K, Lau RWH, Ng CSH. The comparison of electromagnetic with virtual bronchoscopic navigation accuracy at hybrid operating room in patient with sternal wires. AME Case Rep 2020;4:5.


