INTRODUCTION
Chronic tobacco smoking is one of the leading preventable risk factors for non-communicable diseases, with immediate and long-term adverse health consequences such as cancer, cardiovascular disease, respiratory disease, and compromised immune system1. In 2015, there were reportedly 148.6 million disability-adjusted life years (DALYs: a measure of overall disease burden, expressed as numbers of years lost due to ill-health, disability or early death) attributable to smoking worldwide, resulting in adverse personal and population health effects, together with billions of dollars in lost productivity and healthcare costs2. In addition to the direct health consequences, it is estimated that smoking an average of 15.8 cigarettes daily reduces the lifespan by 6.5 years or 11 minutes of life per cigarette3. Globally, tobacco smoking is the cause of more than 6 million premature deaths annually4. Although smoking generally is declining worldwide, there are certain geographical regions where the prevalence remains high. The Global Adult Tobacco Survey (GATS) 2016 found that 49.5% of Russian men and 14.4% of Russian women used tobacco5, compared to 30% men and 7% women globally6, making the Russian Federation one of the highest tobacco-consuming countries in the world5. Other studies on smoking prevalence in the Russian population are relatively few and limited to the population of university students7-9 and to inpatients at medical institutions10. At the same time, life expectancy for Russian men is much lower compared to other Western European men, with tobacco smoking being suggested as one of the primary reasons for this difference11. Tobacco use ranks among the top risk factors for total deaths and total DALYs in Russia12.
In response to the increasing number of smoking-related deaths worldwide, the World Health Organization (WHO) has set out the Framework for Convention on Tobacco Control (FCTC), a treaty aimed at reducing smoking through regulatory strategies, and the MPOWER report that defines policies consistent with the FCTC13. Russian institutions and departments have implemented several measures aimed at reducing the consumption of tobacco products in the population14, entirely consistent with the visions of the WHO FCTC. These measures have yielded substantial results, reflected in a significant reduction in tobacco consumption in Russia in recent years15.
Smoking is a significant risk factor for non-communicable diseases and is known to be highly correlated with other negative lifestyle factors such as consumption of psychoactive substances, especially alcohol16, and mental distress17. Although a few studies have investigated the prevalence among emergency-department patients, most of those studies found that prevalence among those patients is higher compared to the general population18-20. By reducing negative lifestyle factors such as tobacco smoking among patients admitted for acute medical illnesses, it is possible to lower the burden of non-communicable diseases on the healthcare system21, reduce coronary heart disease mortality22, and improve quality of life23. The departments of multidisciplinary clinics admitting patients can be crucial places in identifying individuals with tobacco addiction because of the increased focus on patient health and the lack of triggers associated with smoking in the hospital environment. Studies show that many patients who are smokers or have harmful alcohol consumption might experience a ‘teachable moment’ when they are admitted to hospital24, and so be willing to change their behaviour. However, unlike the use of alcohol, non-medicinal drugs, and illicit drugs, smoking is more socially acceptable, resulting in a significantly lower level of biased self-reporting. Subsequently, from a clinical perspective, the correlation between smoking and alcohol use would be of interest as daily smokers might be easier to identify than those with harmful alcohol use. Emergency medical department populations provide an excellent opportunity for screening and subsequent smoking cessation interventions.
The main aim of this study was to investigate sociodemographic and lifestyle predictors of tobacco smoking, and the association between smoking and harmful alcohol use, among acute medically ill patients admitted to the somatic departments of one of Moscow’s multidisciplinary hospitals, as both smoking and harmful alcohol use are important risk factors for non-communicable diseases.
METHODS
Participants
A cross-sectional study was conducted at the V. P. Demikhov hospital in Moscow during a 1-year period (November 2016 through December 2017). The hospital is a multidisciplinary clinic with 972 beds and an annual hospitalization rate of about 60000 patients; the study inclusion areas were the southeastern districts of Moscow. Recruitment and interviews were performed by addiction doctors at the hospital, and the recruitment of patients was performed seven days and nights per week in the departments of internal medicine, neurology, pulmonology, and cardiology. The study was approved by the Local Ethical Committee of Moscow Research and Practical Centre on Addictions (Approval No. 04/2016 of 27.09.2016). Before inclusion, eligible participants were informed about the study, and those that agreed to take part provided a signed informed consent for participation. Inclusion criteria were acute medically ill patients aged ≥18 years. Exclusion criteria were injury (as the reason for admission), non-Russian-speaking patients, or patients unable to provide informed consent for other reasons. To determine smoking status patients filled in self-reporting questionnaires, or, in the case of poor health condition, the questionnaire was filled in by the interviewer. The study was conducted anonymously, and the participant data were entered into the project database coded by an identification number. This study is part of a larger collaborative project between Oslo University Hospital and the Moscow Research Center on Addictions.
Measures
Self-reported questionnaires were completed for each patient, and data on gender and age were gathered. Socioeconomic factors such as partnership status (married/living with partner, LWP, divorced, single, or widowed) and occupational status (economically active, not economically active, including unemployed and disabled in working age, and retired) were recorded. To assess mental distress, the Symptom Checklist 5 (SCL-5) questionnaire was used25. SCL-5 is a validated measure comprising 5 items extracted from the SCL-90 full version questionnaire, which was translated and previously used in a Russian population26. In the present study, SCL-5 was used as a dichotomized variable with a cut-off score of >2, as an indicator of mental distress. Self-reported alcohol use was assessed using the Alcohol Use Disorders Identification Test 4 (AUDIT-4), which consists of the three first and tenth item of AUDIT27. On AUDIT-4, each item is given a score from 0 to 4 points, giving a total score ranging from 0 to 16. We used AUDIT-4 total score as a dichotomized variable for detection of harmful alcohol use with a cut-off ≥7 [m] for males and ≥5 [f] for females28. AUDIT-4 provides a continuous score reflecting risk and severity in alcohol use. In addition to using it as a dichotomized variable, AUDIT-4 was also divided according to the proportion of the WHO division of the full AUDIT into four zones reflecting different drinking patterns: zone 1 - low-risk drinking or abstinence (0–3 points); zone 2 - alcohol use in excess of low-risk guidelines (4–6 points); zone 3 - hazardous drinking (7–8 points); zone 4 - risky alcohol use and possible alcohol dependence (≥9 points)29. We applied these ‘definitions’ and modified divisions of zones from the full AUDIT (10 items) to our 4-item AUDIT-4 zones, bearing in mind that the full AUDIT scores range 0–40 points, whereas AUDIT-4 scores range 0–16 points. Also, to facilitate the patient’s understanding of the ‘standard drink’ concept, a graphic aid was developed, visualizing the size of a single dose for the most common Russian alcoholic beverages (beer, dry wine, fortified wine, strong alcoholic beverages). The size of a single dose in the study was 10 g of absolute alcohol, as recommended by WHO29. Lastly, the patients were asked about their tobacco smoking behavior using a specially designed questionnaire. They were first asked about their experience with tobacco use. If the patient reported that he/she had never smoked or was not currently smoking (never-smoker), the questionnaire was not filled in any further. For patients who had previously smoked, but had quit for more than six months (quitters), then the time since quitting was recorded. If the patient was smoking at the time of data collection or stated that he/she quit smoking within the last six months, they were defined as smokers, and data on daily number of cigarettes, years of smoking and Fagerström test for nicotine dependence (FTND) was used to determine the severity of smoking dependence30,31. The FTND questionnaire is an internationally validated screening tool for nicotine dependence and consists of 6 items30,31. The answers to each item are given points ranging from 0 to 1 or 0 to 3, where the highest point reflects the highest degree of dependency, with 10 points being the highest total score. To achieve the objectives of the study, we applied the generally accepted division into 4 zones, corresponding to: zone 1 - low dependency (0–2 points); zone 2 – low to moderate dependency (3–4 points); zone 3 – moderate dependency (5–7 points); and zone 4 – high dependency (≥8 points)30.
Data analysis
Statistical analysis was performed using IBM SPSS Statistics 25.0, supplied by Predictive Solutions, the official supplier of IBM SPSS software products in Russia. Smoking status (and cessation) was used both as a dichotomous and categorical variable, AUDIT-4 was used as a dichotomous and ordinal variable, and FTND was used as an ordinal variable. Chi-squared test and binary logistic regression adjusted for all variables were used to investigate the association between smoking status (and cessation) and demographic variables, mental distress, and alcohol use. Linear-by-linear Association Test was used to investigate the association between AUDIT-4 zones and FTND zones. The level of significance was p<0.05 for all statistical tests.
RESULTS
In total, 91% (N=3009) of the eligible patients consented to take part in the study, and descriptive data, for the whole study group and for the study group divided into smoking status, are presented in Table 1. The total prevalence of smokers among the patients was 31.6%. There were marginally more women compared to men included in the study (52.9% and 47.1%, respectively), and approximately half of the male patients were smokers (49.2%) compared to 15.8% of the female patients, the difference being significant (chi-squared test p<0.001). The proportion of smokers in each age group decreased with increasing age, with 53.4% of smokers in the youngest age group (18–40 years), and 6.3% in the oldest age group (≥71 years). Partnership status was found to be significantly associated with smoking, and almost half of the single and divorced patients (50.6% and 45.0%, respectively), 34.2% of married or cohabiting patients, and only 12.1% of widowed patients, were smokers. Among the economically non-active patients, 57.4% were smokers, while 44.9% of economically active patients and 16.4% of retired patients were smokers. The greatest proportion of smokers was found in the zone of risky alcohol use (9–16 points), with 73.9% being smokers, and the zone of hazardous alcohol use (7–8 points), where 73.2% identify as being smokers. The lowest proportion of smokers was in the zone of low-risk alcohol consumption or abstinence (0–3 points), with 19.1% being smokers.
Table 1
Characteristics of the study sample admitted to a Moscow hospital, 2016–2017 (N=3009)
| Variables | Total | Non-smoker | Smoker ** | pa |
|---|---|---|---|---|
| n (% within variable) | n (%) | n (%) | ||
| Gender | 0.000 | |||
| Male | 1418 (47.1) | 720 (50.8) | 698 (49.2) | |
| Female | 1591 (52.9) | 1339 (84.2) | 252 (15.8) | |
| Age (years) | 0.000 | |||
| 18–40 | 528 (17.5) | 246 (46.6) | 282 (53.4) | |
| 41–60 | 924 (30.7) | 493 (53.4) | 431 (46.6) | |
| 61–70 | 742 (24.7) | 556 (74.9) | 186 (25.1) | |
| ≥71 | 815 (27.1) | 764 (93.7) | 51 (6.3) | |
| Partnership status | 0.000 | |||
| Married/LWP*** | 1457 (48.4) | 958 (65.8) | 499 (34.2) | |
| Divorced | 398 (13.2) | 219 (55.0) | 179 (45.0) | |
| Widowed | 810 (26.9) | 712 (87.9) | 98 (12.1) | |
| Single | 344 (11.4) | 170 (49.4) | 174 (50.6) | |
| Employment status* | 0.000 | |||
| Active | 897 (29.8) | 494 (55.1) | 403 (44.9) | |
| Non-active | 491 (16.3) | 209 (42.6) | 282 (57.4) | |
| Retired | 1620 (53.9) | 1355 (83.6) | 265 (16.4) | |
| SCL-5* | 0.001 | |||
| ≤2 | 2764 (92.1) | 1987 (71.9) | 777 (28.1) | |
| >2 | 238 (7.9) | 152 (63.9) | 86 (36.1) | |
| AUDIT-4 zones* | 0.000 | |||
| 1 (0–3) | 2214 (73.7) | 1792 (80.9) | 422 (19.1) | |
| 2 (4–6) | 238 (7.9) | 121 (50.8) | 117 (49.2) | |
| 3 (7–8) | 123 (4.1) | 33 (26.8) | 90 (73.2) | |
| 4 (9–16 points) | 429 (14.3) | 112 (26.1) | 317 (73.9) |
Binary logistic regression was used in order to investigate the association between smoking and demographic variables, mental distress, and alcohol use. The odds ratios (ORs) adjusted for all variables are depicted in Table 2. There was a significant association between gender and smoking, with a lower OR for women being smokers compared to men (OR=0.30; p<0.001). Age was also significantly associated with smoking, with ORs of 0.52 and less for the two oldest age groups, using the age group 18–40 years as reference (p<0.01). Compared to married patients or patients living with a partner, divorced and single patients had higher ORs of being smokers (OR=1.61, p<0.001; and OR=1.62, p=0.002; respectively). Being economically non-active was found to be significantly associated with smoking, compared to being economically active (OR=1.47; p=0.003). The most marked association with tobacco smoking was noted in the group with harmful alcohol use according to the dichotomized AUDIT-4 score (≥5 [f] / 7 [m]), compared to those with non-harmful alcohol use (OR=4.04; p<0.001).
Table 2
Binary logistic regression of factors related to current smoking status among patients who visited the hospital, Moscow 2016–2017
| Variables | Adjusted OR | 95% CI | p |
|---|---|---|---|
| Gender | |||
| Male | Ref. | ||
| Female | 0.298 | 0.241–0.368 | 0.000 |
| Age (years) | |||
| 18–40 | Ref. | ||
| 41–60 | 0.862 | 0.660–1.126 | 0.276 |
| 61–70 | 0.524 | 0.355–0.773 | 0.001 |
| ≥71 | 0.142 | 0.087–0.233 | 0.000 |
| Partnership status | 1.606 | 1.216–2.121 | 0.001 |
| Married/LWP** | Ref. | ||
| Divorced | |||
| Widowed | 1.143 | 0.829–1.577 | 0.414 |
| Single | 1.622 | 1.203–2.186 | 0.002 |
| Employment status | |||
| Active | Ref. | ||
| Non-active | 1.469 | 1.138–1.897 | 0.003 |
| Retired | 0.802 | 0.582–1.105 | 0.177 |
| SCL-5 | |||
| ≤2 | Ref. | ||
| >2 | 1.406 | 0.994–1.989 | 0.054 |
| AUDIT-4 | |||
| < 5 [f] / 7 [m] | Ref. | ||
| ≥ 5 [f] / 7 [m] | 4.036 | 3.224–5.052 | 0.000 |
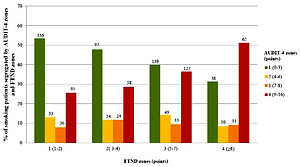
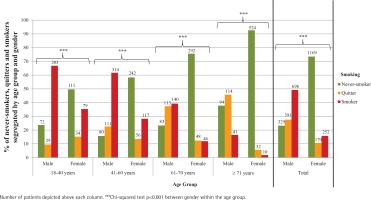
When asked about smoking status and cessation, 49.2% of all male patients responded that they were smokers (current smokers or had quit within the last 6 months), compared to 15.8% of all female patients, as shown in Figure 1. Approximately equal proportions of all male patients had either quit for ≥6 months or never smoked (27.6% and 23.2%, respectively), while most female patients had never smoked (73.5%) and 10.7% had quit ≥6 months. The results showed that the proportion of female smokers and quitters decreased with increasing age and that the proportion of female never-smokers increased with age. Comparatively, the proportion of male smokers tended to decrease with increasing age, while the proportion of male quitters increased with increasing age. However, the proportions of male never-smokers appeared to be comparable among the three youngest age groups and somewhat higher in the oldest age group (37.8%). While there were more men compared to women in the two youngest age groups, and marginally more women in the age group 61–70 years, there were more than twice as many female patients in the oldest age group compared to male patients.
Figure 1
Smoking status and cessation (never-smoker, quitter, smoker) segregated by age group and gender
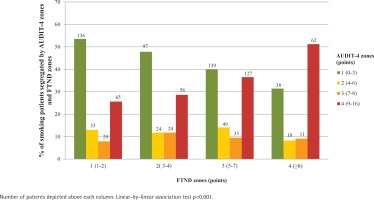
For the investigation of the relationship between nicotine dependence and alcohol consumption, a Linear-by-Linear Association Test was performed using FTND zones as the independent variable and AUDIT-4 zones as the dependent variable. It was found that over half of the patients with low nicotine dependence (1–2 FTND points) also had low alcohol consumption (0–3 AUDIT-4 points, p<0.001), as shown in Figure 2. At the same time, over half of those with high nicotine dependence (≥8 FTND points) also had risky use of alcohol (9–16 AUDIT-4 points). A high proportion of individuals (with various degrees of nicotine dependence) had either low or high alcohol consumption.
DISCUSSION
In this study, comprising acutely ill patients admitted to V. P. Demikhov hospital in Moscow, we found that tobacco smoking was significantly associated with several factors such as partnership status, being economically non-active and having mental distress, while those with harmful alcohol use displayed four times higher odds ratio of smoking compared to those without harmful alcohol use.
The overall prevalence of smokers in this hospital population (31.6%) was found to be approximately the same as the population prevalence in Russia, estimated at 30.5% in 20165. These prevalences are about equal to what was found in previous studies investigating smoking prevalence among hospital patients. A hospital population comprising 399 Russian cancer patients found that 41.6% were smokers32, indicating a higher prevalence compared to the general population, however smoking is a well-known significant risk factor for cancer. Also, among 335 Australian ED patients smoking prevalence was found to be 23%, compared to 18% in the general population33. One explanation for the similar prevalences in our study and the general Russian population might be that our hospital population is older compared to the general population described in GATS, which might be due to the negative impact of tobacco use on individual life expectancy. Also, GATS showed that older adults generally believe that smoking causes serious illnesses5, which again might explain why fewer older adults smoke. The patients in the younger age groups (18–40 and 41–60 years) have a much higher prevalence of smokers compared to the younger age groups in the general population (15–24, 25–44 and 45–64 years)5, indicating that smoking might have been a contributing factor for somatic illness in the younger patients.
The higher prevalence of male smokers in all age groups in our study is in concordance with what we know of global gender-differences in tobacco use34, especially in low- and middle-income countries13, and smoking is generally associated with socio-cultural and economic factors35. Although tobacco advertisement is prohibited by law in Russia, it was found in GATS that a higher percentage of non-smoking men compared to non-smoking women had noticed cigarette marketing during the last 30 days, especially in stores where cigarettes are sold and on the internet, and more women generally also believed that smoking caused illness5, which might explain the lower prevalence of female smokers in both our study and the general Russian population.
When investigating sociodemographic predictors, we found that smoking was significantly associated with partnership status, with a higher proportion of smokers being observed among single and divorced patients compared to patients that were married/LWP. Other studies have found similar associations between smoking and partnership status36. One reason for higher smoking prevalence among single and divorced patients might be that smoking is a mechanism to cope with the psychosocial stress of living alone and different values concerning smoking. Smoking was found to be significantly associated with employment status, with a higher proportion of smokers among economically non-active compared to economically active patients, similar to other studies37. As smoking results in more negative health consequences, this might be one of the reasons why there are more smokers among economically inactive patients. The lower proportion of smokers among the retired patients was not significant after adjusting for all other variables, presumably because of the high proportion of older women in this group.
Negative lifestyle factors, such as harmful alcohol use, were found to be significantly associated with smoking, in agreement with other studies on alcohol use and smoking38. The linear relationship between smoking dependence (FTND) and harmful alcohol use among patients underlines the importance of identifying these patients.
When examining smoking cessation between genders, we found that increasing proportions of men quit smoking with increasing age, compared to women. Women tend to be less likely to quit smoking, especially in the long-term, compared to men, but there are significant variations both regarding time-interval, geography and treatment/non-treatment settings39.
Patients will have health benefits from smoking cessation, and admission to a hospital is an excellent opportunity to intervene, especially since the patient might be more motivated to stop smoking in this setting. A review of smoking intervention studies in hospitals found that high-intensity behavioral smoking cessation interventions initiated during the hospital stay, with prolonged contact after discharge, promoted increased smoking cessation rates40. In order to design effective programs for detection and subsequent psychological and medical treatment of tobacco-smoking patients, it is essential to know the sociodemographic portrait of this patient group, and its association to other negative lifestyle factors such as harmful alcohol use. It would be interesting to investigate the patient’s motivation to reduce or quit smoking and alcohol use at admission to hospital, as this knowledge would be beneficial in developing comprehensive therapeutic interventions aimed at reducing both alcohol and tobacco use.
CONCLUSIONS
This study demonstrated that tobacco smoking is a widespread phenomenon among acute medically ill patients in Moscow, especially among younger patients, and that there is an association between harmful alcohol use and tobacco smoking among patients. Based on other studies, we believe that patients will be motivated and benefit from cessation interventions for smoking and alcohol use, at the hospital.