Abstract
Introduction:
Among the high grade cerebral gliomas, Glioblastoma multiform for instance, would be the main pattern of local recurrence causes clinical deterioration and deaths. This has observed 2 - 3 cm upon the initial lesion. During the period of 2 - 4 weeks post-surgery, remaining tumor cells have re-grown until radiochemotherapy has initiated. So it has seemed clear that improved local control could hopefully translate into improved survival. As a matter of fact, mass reduction has insufficiently achieved in almost every case of GBM as that the tumor cell number has not fallen below a “threshold” that tumor control might achieve by the host immune system.Case Presentation:
We have been reporting 3 cases of high grade gliomas, one recurrent GBM, one primary glioma grade III, and the last one recurrent Rhabdoid GBM, which have been fulfilling our entrance criteria of IORT procedure, by using spherical applicators, which has been increasingly discussed in recent studies.Conclusions:
It was the first experience of intraoperative radiation therapy for cerebral malignant tumours in Iran. Finally, we had a brief overview on the past and present IORT strategies in the treatment of GBM.Keywords
Intraoperative Radiation Therapy Glioma High Grade Glioblastoma Multiform
1. Introduction
Malignant gliomas, including anaplastic astrocytoma and gliblastoma multiform have known as the most aggressive and most lethal primary brain tumor, with extremely poor prognosis and high rate of recurrence, even after surgery and radiotherapy. In current studies, among all the associated factors which might improve the prognosis, median survival has roughly considered 14 months for glioblastoma multiform (1) and 2 - 3 years for actrocytoma (2), with the high possibility in progression to glioblastoma multiform. Reports of cases exceeding 40 months of survival have discussed in some retrospective studies (3, 4). As a matter of fact, improving the local control could significantly increases the survival since it has proven that the main pattern of recurrence is local proliferation of the tumor, rather than distant metastasis, and the use of focal radiation fields appeared to be the most judicious approach to the treatment of patients with gliomas (5-8). Increasing the total radiation dose has limited by the consideration of exposure to the normal brain tissue. Intraoperative radiation therapy is a method of irradiation of a large single dose to the tumor bed, while the exposure of normal surrounding tissue has reduced.
2. Case Presentation
2.1. Case 1
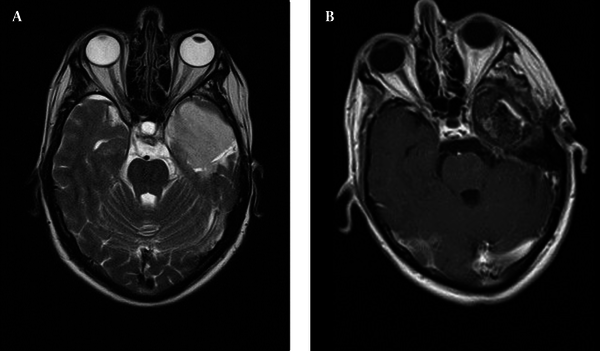
A 43 year old man with one month history of generalized seizure, and upward gaze and recent mild headache, and a past medical history of grade II glioma of 7 years ago, has come to the hospital with an evidences of a left temporal tumoral lesion, with mild enhancement and the size of 44 × 64 × 42 mm (Figure 1) in his routine subsequent brain MRI and. For more details, 3DCSI MRS with color coded map has obtained which revealed remarkable cholin rise with respect to NAA, which prompted him to the plan of surgical debulking and intraoperative radiation therapy as the known case of recurrence glioma with a history of previous receiving a total of 5.5 Gy radiation therapy. At the time of admission he has seemed alert, oriented with the Karnofsky score of 80 and Barthel index of 90. Pre operation CBC, LFT and RFT were normal.
A, Brain MRI of the case 1 which shows left temporal glioma; B, Post-operative MRI which shows complete tumor removal.
2.1.1. Surgical Procedure
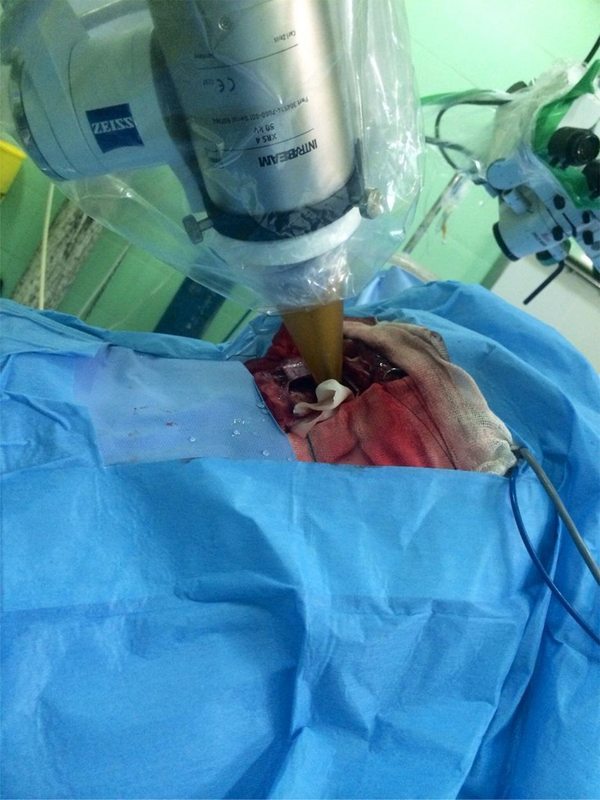
After performing a left temporal lobectomy, we have successfully resected more than 98% of the tumoural cavity, by using the conventional frameless neuronavigation-guided microsurgical tumor resection, tumoural bed has prepared for the placement of radiation source. The size of resection cavity in 3D was 4 × 5 × 3.5 cm. The craniotomy margin that has surrounded the tumor was 7 × 8 cm. Frozen section has confirmed high grade glioma. After achieving the favorable homeostasis, right before subjecting the tumor bed into the focal irradiation, has potentially involved risk structures and the expected doses to the risk organs have calculated by the team of neurosurgeons and radiation oncologists by considering the cavity borders using the neuronavigation software, the cavity geometry. Potential risk structures have identified. The most suitable applicator size has considered 3.5 cm in this patient. Then any skin or bone that could receive direct or scattered irradiation has shielded using sterile cutton pieces. IORT has applied in a straight forward way in the surgical procedure using the 50 Kv INTRABEAM® system (Carl Zeiss Meditec AG, Germany) and 10.3 Gy of focal irradiation therapy has administered for 12 minutes (Figure 2). Lateral side of the spherical probe had 0.5 cm distance to the resection bed, while for the posterior, anterior and medial sides it was zero. Optic Nerve with the distance of 8 mm and Optic Chiasma with 15 cm have considered as risk structures, and have paid attention to be safe with the calculation of probable expose of 3.7 Gy and 1.8 Gy, respectively. The intraoperative radiation therapy procedures have gone uneventful. After completion of the procedure, absolute hemostasis has maintained, duraplasty has performed with the pericranial patch. Cranioplasty has made with microplate and the wound has closed in layers. Post-operative MRI has shown gross total tumor removal (Figure 1).
The IORT Applicator Adjusted Into the Tumor Bed
2.1.2. Clinical Progress
The patient has gradually improved 48 hours after procedure, with the GCS of 15. Follow up pattern started with the early 48 - 72 hours post-operative MRI (Figure 1) and neurocognitive tests, in which he has shown functionally independent with the Barthel’s score of 100 and Karnofsky score of 90. Post operation CBC, LFT and RFT have remained normal. Follow-up brain imaging (Figure 1) has only shown some areas of encephalomalacia. Four days after the procedure he has presented with sign of aphasia which improved and disappeared within the next 3 days. He has discharged a week after the procedure and has currently under gone our regular follow-ups every 3 months, based on the combination of imaging studies (MRI), clinical presentation (physical examination, KPS, current medication) and a neurological assessment using the late effects in normal tissues subjective, objective, management and analytic (LENT-SOMA) scales.
2.2. Case 2
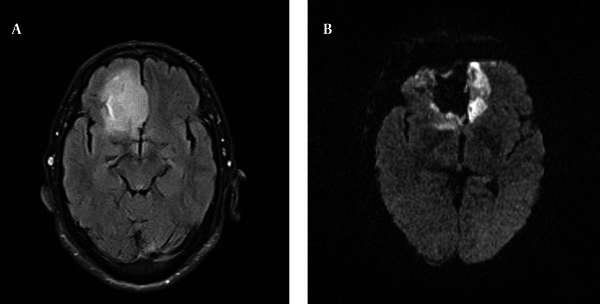
A 52 years old man with mild headache, seizure and blurring of vision with no previous history of malignancy has referred to the neurosurgery clinic. His brain MRI has shown a lesion in frontal lobe with no significant enhancement with the size of 24 × 48 × 42 mm (Figure 3). And a report of grade III glioma in MRS. Patient has candidate for the plan of debulking and intraoperative radiation therapy. At the time of admission, he was alert and oriented with the Karnofsky score of 90, and Barthel index of 90. Surgical procedure has performed with the approach of right frontal craniotomy with the access to the anterior cranial cavity. Tumor bed has debulked in 2 × 4.5 × 4 cm with the craniotomy margin of 5 × 5 cm around the tumor. After the total resection of more than 98% and reaching the hemostasis, the tumor bed has subjected to the 3.5 cm applicator of 50 Kv Zeiss intrabeam and the total of 12 Gy was to the focal irradiation. With the calculated risk structure of 1 Gy exposure to the optic nerve in 2 cm distance. The whole procedure had no remarkable complication and 48 hours later, the GCS of the patient was of 15, Karnofsky score was 90 and Barthel index was 90. Post-operative MRI has shown gross total tumor removal (Figure 3). He has shown no remarkable complication and now has considered to be followed up in the pattern of routine imaging and neurocognitive tests.
A, Pre-operative MRI of the second patient with right frontal lesion; B, Post-operative which shows complete tumor removal.
2.3. Case 3
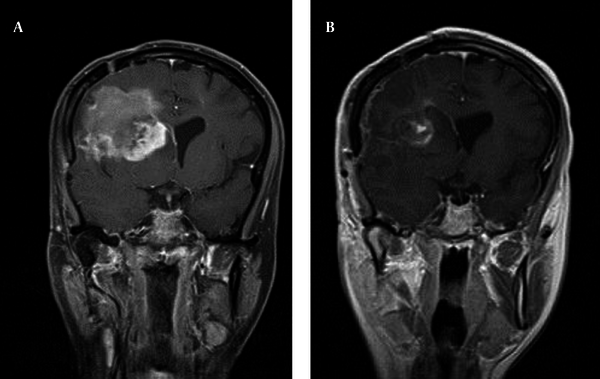
The third case was a 30 years old woman complaining of headache and obscuration of vision, with a history of Rhabdomoid GBM of 12 months ago, for which, she has received 60 Gy external radiotherapy. Her MRI has shown evidences of a right parietal lesion with mid line shift and contrast enhancement, with the size of 56 × 53 × 46 mm and pushing the motor cortex to the posterior (Figure 4). Brain M R spectroscopy (MRS) has confirmed grade IV glioma. She was alert, and oriented, with Barthel score 90 and Karnofsky of 100. As a known case of recurrence of glioma she has undergone a sub total resection (88 - 98%). The resection cavity was in 5.4 × 4.5 × 4.5 cm. After achieving the hemostasis, 8.8 Gy of focal radiation was irradiated in 2.5 cm depth by the 4.5 cm spherical applicator of IORT. The probe had the 0.5 cm to the motor cortex as the risk structure. The patient was stable clinically. Post-operative Barthel and Karnofsky index was as the same of pre operation state. No significant side effect has detected. Post-operative MRI has shown gross total tumor removal (Figure 4).
A, Pre-operative MRI of the 3rd patient with right parietal lesion; B, Post-operative MRI which shows complete tumor removal.
3. Discussion
The idea of application of electron beam-based IORT (IOERT) has first come into the mind of a pioneering group of scientists, on patients with supratentorial gliomas (9, 10). A brief review on literatures has shown the fact that, the effectiveness of intraoperative radiotherapy, on median survival, possible side effects and increasing quality of life has been discussed by the previous studies who has reported divergent outcomes, from highly effective, by Sakai et al. in 1991 for the first time (11), Matsutani (12) and Nakamura (13) in early 90s, to poorly remarkable, Nemoto (14) for instance. Ortiz, Fujiwara and Yong have believed IORT could be feasible for the treatment of malignant gliomas (15-17). In 2005, Schueller et al. has revealed their 12 years of experience in intraoperative radiotherapy. They have reported that there was no significant difference in outcome between primary tumors and recurrences (18). They have also concluded that IORT is a feasible method of increasing the local dose in the treatment of malignant gliomas. Neither complications have risen, compared to surgery and postoperative irradiation, nor outcome significantly improved. They have suggested that IORT should only be performed in specially equipped centers with making an accurate treatment plan to ensure complete target volume coverage. They have also mentioned that since additional temozolomide could significantly improve the results in GBM patients, a combination of IORT and temozolomide might be an interesting option in the future (18).
In 20s, when the Spherical applicators has come to the stage, rather than the forward scattering ones, Takakura and Kubo have treated 55 high-grade gliomas with the spherical applicators and saw 2-year survival rates of 89% and 42% for patients with anaplastic astrocytoma or GBM, superior to the control rates from the Japanese tumor registry (77% and 21%) (19).
In 2012, Zamzuri et al. (20) has reported a GBM case with the treatment planning of surgical resection, intraoperative radiation therapy (IORT) in combination with whole brain irradiation therapy and chemotherapy (temozolamide cycles), whose symptoms have improved after 3 months of this polymodal therapy and remained independently functional for more than two years. In more recent studies, Han has come to the conclusion that long term follow up for recurrent malignant brain tumors have not been satisfying, but for new diagnosis brain tumor patients have shown good local tumor control with relatively long term survival (21). In 2014, Giordano et al. pose the question, if IORT was a resurrected option for treating glioblastoma (22). As an explanation why the outcomes in previous studies have shown such a controversy, he has come to the conclusion that the majority of previous studies has used forward-scattering electron tubes (resembling intraoperative electron radiotherapy, IOERT) and suffered from technical and geometrical mistakes.
As we have known, extent of resection was one of the most important prognostic factors in patients with GBM and patients with more than 98% of tumor resection have a significantly higher survival rate than the patients with incompletely resected tumors (19, 23) which could be possible in only 20% of all GBM patients (24) due to technical errors or involvement of eloquent areas. So, it has seemed important to consider some add-on techniques to achieve additional tumor cell depletion or at least a growth arrest residual non resected cells, in the interval of surgery and adjuvant therapies. Intraoperative radiotherapy (IORT) could be one of the novel approaches with good news, on condition of minimizing the limitations including, areas of inadequate target volume coverage (TVC), wrongly selected electron energies (mostly too low), inappropriate cone sizes (mostly undersized) and angle errors (22). They have found that patients with adequate TVC showed a significantly improved median survival and 2-year survival rate in comparison with the patients with inadequate TVC. Novel devices such as INTRABEAM (Carl-ziess, AG, Germany) which we have used in our experience, has proven to achieve local control in up to 80% of cases with delayed necrosis appearing in less than 5% (25), the putatively most widely recognized paper reporting on outcomes after IORT for brain tumors with the INTRABEAM applicators has published by John Kalapurakal and his colleagues from Chicago’s Northwestern Memorial Hospital, focusing on 14 children with recurrent primary brain tumors (mostly ependymomas, n = 13) with 10 Gy in 2 and 5 mm depth or 12 Gy in 2 mm depth) using spherical applicators (26). They have reported a median follow-up of six months (range, 5 - 40 months) the group had three cases of radiation necrosis and all have been occurring in previously un irradiated patients that have treated at the higher dose level (10 Gy in 5 mm depth). Although none of these patients have died and all remained asymptomatic after treatment. Although the group have decided to stop the dose escalation and limit the dose to 10 Gy in 2 mm depth. As no other late toxicity has appeared and local control has achieved in 8 out of 14 patients (57%) with the best response has observed in previously un irradiated tumors (local control has achieved in 5 of 6 patients; 83%). Therefore, IORTs with INTRABEAM applicators could be judged as feasible and safe procedures even in children, where brain tissue was most sensitive to irradiation (27, 28). They have called it a benefit which was greater than the risk, and IORT was not inferior option in overall survival and a superior option in terms of quality of life, compared to EBRT or chemotherapy alone (22, 27, 28).
As the extent of brain necrosis in the cerebrum has determined the improvement in overall survival, we also have paid attention to calculate the impact of necrosis in the cerebrum (e.g. the frontal, parietal, temporal or occipital lobes) and those of the risk structures including brain stem and the optical nerves/chiasm.
In brief, the full potential of the procedure, up to now has not been defiantly clear as most previous studies used forward-scattering (electron-based) irradiation techniques, which frequently caused inadequately covered target volumes. We have reported our first experience of intraoperative radiation therapy with cerebral malignant Glioma, 1 primary grade III Glioma, and 2 recurrent GBM (one Rhabdoid GBM), using the Spherical applicator and INTRABEAM X-ray device. This patient with recurrent glioma has already received the maximum dose of radiotherapy and couldn’t get any further doses. They have currently under gone our regular follow-up program every 3 months, based on the combination of imaging studies (MRI), clinical presentation (physical examination, KPS, current medication) and a neurological assessment using the late effects in normal tissues subjective, objective, management and analytic (LENT-SOMA) scales.
Acknowledgements
References
-
1.
Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJB, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10(5):459-66. https://doi.org/10.1016/s1470-2045(09)70025-7.
-
2.
Nuno M, Birch K, Mukherjee D, Sarmiento JM, Black KL, Patil CG. Survival and prognostic factors of anaplastic gliomas. Neurosurgery. 2013;73(3):458-65. [PubMed ID: 23719055]. https://doi.org/10.1227/01.neu.0000431477.02408.5e.
-
3.
Heesters M, Molenaar W, Go GK. Radiotherapy in supratentorial gliomas. A study of 821 cases. Strahlenther Onkol. 2003;179(9):606-14. [PubMed ID: 14628126]. https://doi.org/10.1007/s00066-003-1098-9.
-
4.
Laws ER, Parney IF, Huang W, Anderson F, Morris AM, Asher A, et al. Survival following surgery and prognostic factors for recently diagnosed malignant glioma: data from the Glioma Outcomes Project. J Neurosurg. 2003;99(3):467-73. [PubMed ID: 12959431]. https://doi.org/10.3171/jns.2003.99.3.0467.
-
5.
Choucair AK, Levin VA, Gutin PH, Davis RL, Silver P, Edwards MS, et al. Development of multiple lesions during radiation therapy and chemotherapy in patients with gliomas. J Neurosurg. 1986;65(5):654-8. [PubMed ID: 3021931]. https://doi.org/10.3171/jns.1986.65.5.0654.
-
6.
Hochberg FH, Pruitt A. Assumptions in the radiotherapy of glioblastoma. Neurology. 1980;30(9):907-11. [PubMed ID: 6252514].
-
7.
Wallner KE, Galicich JH, Krol G, Arbit E, Malkin MG. Patterns of failure following treatment for glioblastoma multiforme and anaplastic astrocytoma. Int J Radiat Oncol Biol Phys. 1989;16(6):1405-9. [PubMed ID: 2542195].
-
8.
Salazar OM, Rubin P, Feldstein ML, Pizzutiello R. High dose radiation therapy in the treatment of malignant gliomas: final report. Int J Radiat Oncol Biol Phys. 1979;5(10):1733-40. [PubMed ID: 231023].
-
9.
Goldson AL, Streeter OJ, Ashayeri E, Collier-Manning J, Barber JB, Fan KJ. Intraoperative radiotherapy for intracranial malignancies. A pilot study. Cancer. 1984;54(11 Suppl):2807-13. [PubMed ID: 6498760].
-
10.
Abe M, Fukuda M, Yamano K, Matsuda S, Handa H. Intra-operative irradiation in abdominal and cerebral tumours. Acta Radiol Ther Phys Biol. 1971;10(4):408-16. [PubMed ID: 4107080].
-
11.
Sakai N, Yamada H, Andoh T, Hirata T, Nishimura Y, Miwa Y, et al. Intraoperative radiation therapy for malignant glioma. Neurol Med Chir (Tokyo). 1991;31(11):702-7. [PubMed ID: 1723157].
-
12.
Matsutani M, Nakamura O, Nagashima T, Asai A, Fujimaki T, Tanaka H, et al. Intra-operative radiation therapy for malignant brain tumors: rationale, method, and treatment results of cerebral glioblastomas. Acta Neurochir (Wien). 1994;131(1-2):80-90. [PubMed ID: 7709789].
-
13.
Nakamura O, Matsutani M, Shitara N, Okamoto K, Kaneko M, Nakamura H, et al. New treatment protocol by intra-operative radiation therapy for metastatic brain tumours. Acta Neurochir (Wien). 1994;131(1-2):91-6. [PubMed ID: 7709790].
-
14.
Nemoto K, Ogawa Y, Matsushita H, Takeda K, Takai Y, Yamada S, et al. Intraoperative radiation therapy (IORT) for previously untreated malignant gliomas. BMC Cancer. 2002;2:1. [PubMed ID: 11818027].
-
15.
Ortiz de Urbina D, Santos M, Garcia-Berrocal I, Bustos JC, Samblas J, Gutierrez-Diaz JA, et al. Intraoperative radiation therapy in malignant glioma: early clinical results. Neurol Res. 1995;17(4):289-94. [PubMed ID: 7477745].
-
16.
Fujiwara T, Honma Y, Ogawa T, Irie K, Kuyama H, Nagao S, et al. Intraoperative radiotherapy for gliomas. J Neurooncol. 1995;23(1):81-6. [PubMed ID: 7623073].
-
17.
Chung YG, Kim CY, Lee HK, Lee KC, Chu JW, Choi MS. Preliminary experiences with intraoperative radiation therapy (IORT) for the treatment of brain tumors. J Korean Med Sci. 1995;10(6):449-52. [PubMed ID: 8924231].
-
18.
Schueller P, Micke O, Palkovic S, Schroeder J, Moustakis C, Bruns F, et al. 12 years' experience with intraoperative radiotherapy (IORT) of malignant gliomas. Strahlenther Onkol. 2005;181(8):500-6. [PubMed ID: 16044217]. https://doi.org/10.1007/s00066-005-1354-2.
-
19.
Pichlmeier U, Bink A, Schackert G, Stummer WALA. Glioma Study Group. Resection and survival in glioblastoma multiforme: an RTOG recursive partitioning analysis of ALA study patients. Neuro Oncol. 2008;10(6):1025-34. [PubMed ID: 18667747]. https://doi.org/10.1215/15228517-2008-052.
-
20.
Zamzuri I, Rahman GI, Muzaimi M, Jafri AM, Nik Ruzman NI, Lutfi YA, et al. Polymodal therapy for high grade gliomas: a case report of favourable outcomes following intraoperative radiation therapy. Med J Malaysia. 2012;67(1):121-2. [PubMed ID: 22582564].
-
21.
Han X, Fu B, Wu M, Zhang H, Li D, Zhang J, et al. P13.13 * Intraoperative Radiotherapy with Intrabeam in Primary Brain Tumors after Resection: Preliminary Reports of 26 Cases. Neuro-Oncology. 2014;16(suppl 2):ii68. https://doi.org/10.1093/neuonc/nou174.259.
-
22.
Giordano FA, Brehmer S, Abo-Madyan Y, Welzel G, Sperk E, Keller A, et al. INTRAGO: intraoperative radiotherapy in glioblastoma multiforme-a Phase I/II dose escalation study. BMC cancer. 2014;14(1):992.
-
23.
Stummer W, Novotny A, Stepp H, Goetz C, Bise K, Reulen HJ. Fluorescence-guided resection of glioblastoma multiforme by using 5-aminolevulinic acid-induced porphyrins: a prospective study in 52 consecutive patients. J Neurosurg. 2000;93(6):1003-13. [PubMed ID: 11117842]. https://doi.org/10.3171/jns.2000.93.6.1003.
-
24.
Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95(2):190-8. [PubMed ID: 11780887]. https://doi.org/10.3171/jns.2001.95.2.0190.
-
25.
Curry WJ, Cosgrove GR, Hochberg FH, Loeffler J, Zervas NT. Stereotactic interstitial radiosurgery for cerebral metastases. J Neurosurg. 2005;103(4):630-5. [PubMed ID: 16266044]. https://doi.org/10.3171/jns.2005.103.4.0630.
-
26.
Kalapurakal JA, Goldman S, Stellpflug W, Curran J, Sathiaseelan V, Marymont MH, et al. Phase I study of intraoperative radiotherapy with photon radiosurgery system in children with recurrent brain tumors: preliminary report of first dose level (10 Gy). Int J Radiat Oncol Biol Phys. 2006;65(3):800-8. [PubMed ID: 16580791]. https://doi.org/10.1016/j.ijrobp.2006.01.006.
-
27.
Mulhern RK, Palmer SL. Neurocognitive late effects in pediatric cancer. Curr Probl Cancer. 2003;27(4):177-97. [PubMed ID: 12855950].
-
28.
Briere ME, Scott JG, McNall-Knapp RY, Adams RL. Cognitive outcome in pediatric brain tumor survivors: delayed attention deficit at long-term follow-up. Pediatr Blood Cancer. 2008;50(2):337-40. [PubMed ID: 17458873]. https://doi.org/10.1002/pbc.21223.