Abstract
The purpose of this review is to objectively evaluate the biochemical and pathophysiological properties of 0.9% saline (henceforth: saline) and to discuss the impact of saline infusion, specifically on systemic acid-base balance and renal hemodynamics. Studies have shown that electrolyte balance, including effects of saline infusion on serum electrolytes, is often poorly understood among practicing physicians and inappropriate saline prescribing can cause increased morbidity and mortality. Large-volume (>2 L) saline infusion in healthy adults induces hyperchloremia which is associated with metabolic acidosis, hyperkalemia, and negative protein balance. Saline overload (80 ml/kg) in rodents can cause intestinal edema and contractile dysfunction associated with activation of sodium-proton exchanger (NHE) and decrease in myosin light chain phosphorylation. Saline infusion can also adversely affect renal hemodynamics. Microperfusion experiments and real-time imaging studies have demonstrated a reduction in renal perfusion and an expansion in kidney volume, compromising O2 delivery to the renal parenchyma following saline infusion. Clinically, saline infusion for patients post abdominal and cardiovascular surgery is associated with a greater number of adverse effects including more frequent blood product transfusion and bicarbonate therapy, reduced gastric blood flow, delayed recovery of gut function, impaired cardiac contractility in response to inotropes, prolonged hospital stay, and possibly increased mortality. In critically ill patients, saline infusion, compared to balanced fluid infusions, increases the occurrence of acute kidney injury. In summary, saline is a highly acidic fluid. With the exception of saline infusion for patients with hypochloremic metabolic alkalosis and volume depletion due to vomiting or upper gastrointestinal suction, indiscriminate use, especially for acutely ill patients, may cause unnecessary complications and should be avoided. More education regarding saline-related effects and adequate electrolyte management is needed.
中文概要
概 要
本文旨在客观评价0.9%氯化钠溶液(盐水)的生物化学和病理生理学特性,并深入探讨静脉输注该盐水对机体酸碱平衡和肾脏血流动力学的影响。研究表明多数临床医生对电解质平衡的认识有限,对静脉输注盐水所引起的血浆电解质变化认识不足。而错误地应用盐水会增加患者的患病率和死亡率。健康成人大剂量(>2 L)输注盐水会导致高氯血症并进而引起代谢性酸中毒、高钾血症和负氮平衡。总之,盐水是一种高度酸化的液体,用于治疗呕吐或上消化道减压引起的低氯性代谢性碱中毒和容量不足较为合适。临床上不加区分地应用盐水对患者特别是对重症患者可能导致不必要的并发症,应注意避免。临床医生对于盐水相关作用和电解质管理的认识亟需增强。
Similar content being viewed by others
1 Introduction
0.9% saline (sodium chloride (NaCl), henceforth referred to as saline) was first described by Dr. Hartold Jacob Hamburber (Dutch physiological chemist, 1859–1924) in the 1890s. Having a similar freezing point to human serum and causing no visible erythrocyte lysis, the solution was initially named by Dr. Hamburber “indifferent fluid” (Awad et al., 2014). Over the years, the name has morphed into what is more commonly called “normal saline” or “physiological saline” despite no additional evidence or rationale for the relabeling. The implied normalcy and physiological property have perpetuated indiscriminate use of saline in medical practice. Saline today remains one of the most frequently used solutions for resuscitation of acutely ill patients with a variety of medical problems.
To revisit some of the biochemical properties and clinical applications of saline would likely be beneficial because studies have shown that fluid and electrolyte management for most perioperative care has been left to junior house officers who lack sufficient knowledge and experience to undertake such a task. This problem was highlighted by a survey showing more than half of house officers did not know the amount of Na (likely unaware of high Cl content and low pH) in a liter of saline. Moreover, only 16% of surveyed house staff felt that they were adequately informed on the topic prior to or during their training (Lobo et al., 2001; 2002b).
2 Saline is not physiological
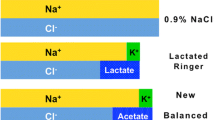
Despite its name, saline is neither “normal” nor “physiological”. Compared to human serum, saline has a nearly 10% higher Na concentration and 50% higher Cl concentration. Table 1 shows the compositions of human serum, saline, and several commonly used balanced crystalloid fluids. The acidic property of saline (pH 5.4) can be clearly explained using the Stewart approach of acid-base balance which provides a perfect framework for its understanding (Stewart, 1983). The three independent determinates of circulating acid-base status are (1) strong ion difference (SID), (2) total concentration of nonvolatile weak acid (Atot), and (3) partial pressure of CO2. Among the three, SID is the predominant determinate of pH. SID is defined as the difference of all fully dissociated cations (i.e. sodium, potassium, calcium, magnesium) and anions (chlorine, lactate, keto-acids, and all other organic anions with pKa values <4.0). SID in normal serum (pH 7.35–7.45) is approximately 40 mmol/L (Fig. 1a). Isolated increases/decreases in SID move the acid-base equilibrium towards metabolic alkalosis/acidosis, respectively. In serum, increases or decreases in Atot (primarily albumin and phosphate) shift the equilibrium towards metabolic acidosis or alkalosis, respectively.
Strong ion difference (SID) in normal circulation (a) and after 0.9% saline infusion (b)
(a) Based on the Stewart model, the difference between cations and anions in normal serum should be approximately 40 mmol/L (pH=7.4). SID decreases when negatively charged anions disproportionately increase compared to positively charged cations, resulting in a pH decline and acidosis. SID increases when anions disproportionately decrease, compared to cations causing pH elevation, metabolic alkalosis. (b) In normal serum, the predominant cation is Na (140 mmol/L) and predominant anions is Cl (100 mmol/L). The SID is approximately 40 mmol/L when pH is 7.4. 0.9% saline infusion causes elevations in both Na and Cl, but Cl increases in a larger magnitude, resulting in a net SID reduction and acidosis
Saline has zero SID (equal concentrations of Na and Cl) and zero Atot. Intravenous saline infusion dilutes existing circulating albumin and phosphate, thus reducing Atot (metabolic alkalosis); simultaneously, the infusion reduces SID (metabolic acidosis). The effect of SID reduction, however, overpowers that of Atot reduction resulting in a net metabolic acidosis if there is no pre-existing acid-base disturbance (Fig. 1b). Thus, saline infusion in humans is expected to perturb the extracellular milieu, especially when large volumes are administered, causing hyperchloremia, which in turn has the potential to cause multiple downstream adverse effects.
3 Hyperchloremia and hyperchloremic acidosis are abnormal
Cl, the most abundant anion in extracellular fluid, plays a fundamental role in the maintenance not only of acid-base balance but also of osmotic pressure, water distribution, and muscular activity in the body (Shires and Holman, 1948; Koch and Taylor, 1992; Powers, 1999; Yunos et al., 2010). Studies have demonstrated that Cl is responsible for about a third of the extracellular fluid tonicity and two-thirds of all anionic charges in serum (Koch and Taylor, 1992). Because of its high concentration, Cl is the most important anion in balancing extracellular cations.
Hyperchloremic acidosis shifts potassium out of cells. Potassium is the most abundant intracellular cation with an intracellular concentration of approximately 140 mmol/L, and only approximately 2% of total body potassium is extracellular. Thus, even the slightest shift of intracellular potassium out of cells, a process directly proportional to the decline in pH, will exert a major impact on extracellular potassium concentration. Therefore, saline-induced acidosis can incite clinically significant hyperkalemia.
Hyperchloremic acidosis in healthy adults adversely affects the nitrogen balance because of the demand on the kidney to generate and excrete extra ammonia and inhibition of growth factor-mediated protein synthesis (Ballmer et al., 1995). In a rodent sepsis model, hyperchloremic acidosis induces an increased concentration of circulating inflammatory mediators (interleukin-6, necrosis factor α, and interleukin-10) in a dose-dependent manner (Kellum et al., 2006). Acidosis and inflammatory state can both compromise cardiac and skeletal muscle performance by reducing calcium sensitivity and maximal force generation (Fujita and Ishiwata, 1999; Morimoto et al., 1999; Moopanar and Allen, 2005; 2006; Day et al., 2006; 2007; Knuth et al., 2006; Debold et al., 2008; Snook et al., 2008; Kapur et al., 2009).
Uray et al. (2011) investigated the effects of saline (80 ml/kg) infusion on intestinal contractile function in rodents. The infusion caused intestinal edema and contractile dysfunction associated with activation of signal transducer and activator of transcription 3 (STAT-3) and sodium-proton exchanger (NHE) and decreased myosin light chain phosphorylation, along with alterations in cytoskeletal muscle organization and F:G actin ratios. These salinemediated effects could be related to both interstitial edema as well as hyperchloremic acidosis because the infusion volume is expected to induce hyperchloremic acidosis. Moreover, hyperchloremic acidosis caused by saline infusion in healthy volunteers has been shown to activate lymphocyte NHEs (Kessler et al., 1997). Saline also exhibits a greater tendency of fluid retention in the interstitial space, compared to balanced crystalloids, causing edema, which is primarily related to a slow rate in excreting excess Cl by the kidneys (Veech, 1986). Thus pronounced interstitial fluid retention and hyperchloremia could be considered as convergent effects of saline infusion.
Cl channels are expressed in almost all cells in the body and appropriately circulating Cl concentrations are essential in maintaining cellular health. Cellular Cl alterations due to dysfunctions in Cl channels result in a broad spectrum of diseases (Puljak and Kilic, 2006; Veizis and Cotton, 2007; Tang et al., 2010). Thus, conceptually, hyperchloremia caused by saline infusion cannot be viewed as normal.
4 Saline-induced pathological effects in humans
The biochemical differences between saline and human serum may have many notable clinical and pathological consequences. For example, in normal adults, compared to intravenous (IV) infusion of balanced fluids, saline infusion causes (1) multiple clinical symptoms including abdominal discomfort, abdominal distention and pain, nausea, drowsiness, decreased mentation and mental capacity; (2) disproportionate Cl elevation, leading to hyperchloremic metabolic acidosis; (3) a longer time to first micturition following the infusion; and, (4) less urine production (Scheingraber et al., 1999; Williams et al., 1999; Reid et al., 2003). In addition, several randomized trials comparing saline with lactated Ringer’s solution administered during the perioperative period have shown that the saline groups had a more frequent occurrence of adverse effects, including hyperkalemia (>6 mmol/L), more blood product transfusion and bicarbonate therapy (Ho et al., 2001; Waters et al., 2001; O’Malley et al., 2005; Modi et al., 2012).
Other clinical studies have shown that hyperchloremic acidosis resulting from saline infusion is associated with reduced gastric blood flow and mucosal pH in elderly surgical patients (Wilkes et al., 2001), delayed recovery of gut function, increased complications, prolonged hospital stay in patients undergoing colonic surgery (Lobo et al., 2002a; Brandstrup et al., 2003), and impairment in cardiac contractility as well as diminished response to inotrope causing hypotension (Mitchell et al., 1972; Levy et al., 2010; Schotola et al., 2012). Saline resuscitation for patients with gastrointestinal hemorrhage exacerbated bleeding resulting in more transfusions compared to balanced fluid resuscitation (Barak et al., 2004). A large retrospective observational study involving 30 994 adults who underwent major open abdominal surgery showed that those who received saline had a significantly greater rate of developing complications, 33.7% versus 23% in those who received balanced fluids (Shaw et al., 2012). Recently, Yunos et al. (2012) conducted a study to compare outcomes of critically ill adults resuscitated with Cl liberal (primarily saline) versus Cl restricted IV fluids. They showed that Cl liberal fluid was associated with significant increase in the development of Stage 2 or Stage 3 acute kidney injury compared to the patients receiving Cl restricted fluid. In the Mayo Clinic admission patients (in the years 2011–2013), post-admission (within 48 h) disproportionate serum Cl increase due to a high proportion of saline infusion was associated with an elevated risk of hospital mortality (unpublished data). Taken together, saline infusion can cause Cl elevation and can exert outcome significance for both healthy adults and acutely ill patients.
5 Pathological effects of saline on renal hemodynamics
Wilcox (1983) conducted a series of studies on anesthetized dogs that had one kidney autotransplantation into the neck. Infusion of a hypertonic and NaCl-containing solution (two-thirds 0.154 mol/L NaCl solution and one-third 1.10 mol/L mannitol) to the renal artery resulted in hyperchloremia that was associated with persistent renovascular constriction (following a brief initial period of hyperosmolality associated vasodilation) and reduction in glomerular filtration rate. The change in renal blood flow and the glomerular filtration rate is highly correlated with changes in fractional reabsorption of Cl, suggesting that renovascular resistance is related to the delivery of Cl, but not Na, to the Loop of Henle. Potassium has also been shown to induce renal vasoconstriction, which is dependent on and responsive to increased extracellular Cl (Jensen et al., 1997; Hansen et al., 1998).
This experimental evidence of the negative impact of saline on renal hemodynamics and kidney function is consistent with findings of renal perfusion impairment induced by saline infusion demonstrated by Chowdhury et al. (2012) in recent years. Using magnetic resonance imaging (MRI) techniques, Chowdhury and colleagues monitored, in real-time, renal blood flow velocity and renal perfusion in healthy adult volunteers following IV infusion of saline versus Plasma-Lyte 148 in a randomized double-blind cross-over design. When compared with Plasma-Lyte 148, saline infusion resulted in a significant decline in renal artery flow velocity and renal perfusion, and an increase in kidney volume consistent with tissue edema. Mechanistically, it is tempting to suggest that disproportionate Cl elevation from saline infusion increases Cl in the fluids of renal tubules, which can activate tubuloglomerular feedback (TGF) and cause afferent arteriolar vasoconstriction, leading to a fall in the glomerular filtration rate (Fig. 2). Studies from genetically engineered mice show that activation of high Cl-affinity NKCC (Na-K-2Cl co-transporter) isoform 2B and lower Cl-affinity NKCC isoform 2A is responsible for a wide range of NaCl concentrations in the tubular fluids over which TGF operates (Oppermann et al., 2006; 2007).
A disproportionate increase in Cl and hyperchloremic acidosis caused by 0.9% saline infusion
The Cl filters into renal tubules. Through macular densa cells, the Cl signal is transmitted to afferent arterioles causing vasoconstriction, resulting in glomerular filtration rate (GFR) reduction and reduction in urine output. Regional ischemia due to saline-associated kidney volume expansion could further stimulate renin secretion from juxtaglomerular cells, leading to activation of the intra-renal renin angiotensin system (RAS). RAS activation would further enhance the proximal tubular Na absorption and afferent arteriolar vasoconstriction via tubuloglomerular feedback (TGF) activation
The role of molecular densa in providing TGF to afferent vessels and signaling pathways leading to changes in renovascular constriction and glomerular filtration rate has been better elucidated recently (Ren et al., 2004; Bell et al., 2009). Cl entry to the molecular densa cells has been shown to cause depolarization to the basal lateral membrane via Cl channels (Bell et al., 1989).
Moreover, kidney volume expansion following saline infusion can cause intra-renal regional tissue ischemia, as the kidneys have little room to expand within the confines of the renal capsule. Interstitial edema induced by saline can cause subcapsular pressure elevation in the kidney and cause renal ischemia (Herrler et al., 2010). The ischemia can induce regional activation of renin-angiotensin system (RAS), which increases proximal NaCl absorption and simultaneously enhances TGF activity causing further afferent arterial vasoconstriction (Mitchell and Navar, 1988) and reduction in the glomerular filtration rate (Mitchell and Navar, 1990). Mediators, which transmit the TGF signal from the macular densa cells to afferent arterioles, include adenosine working collaboratively with angiotensin II (Traynor et al., 1998).
Both extra-renal pressure, such as ascites, and intracapsular pressure to the kidney can decrease the pressure gradient across the renal arterioles and result in decreasing renal blood flow and renal flow velocity. Improvement of urine output and kidney function has been demonstrated after release of the pressures (Stone and Fulenwider, 1977; Zand et al., 2014).
6 Conclusions
Despite the availability of safer and more physiologically balanced solutions and despite not a single study demonstrating saline to be superior to balanced solutions, saline continues to be used frequently, if not the most commonly used resuscitative fluid, in medical practice. Evidence suggests that high Cl-containing fluids (such as saline) are associated with multiple adverse effects including an increased occurrence of kidney dysfunction with possible reduced survival. Although large randomized controlled trials comparing saline and balanced fluids are necessary, the time has come to at least recognize that saline is neither normal nor physiological. Saline administration should be considered to have the same status as a drug prescription. Strengthening knowledge of saline management would likely result in improvement in patient outcomes.
Compliance with ethics guidelines
Heng LI, Shi-ren SUN, John Q. YAP, Jiang-hua CHEN, and Qi QIAN declare that they have no conflict of interest.
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Awad, S., Allison, S.P., Lobo, D.N., 2008. The history of 0.9% saline. Clin. Nutr., 27(2): 179–188. http://dx.doi.org/10.1016/j.clnu.2008.01.008
Ballmer, P.E., McNurlan, M.A., Hulter, H.N., et al., 1995. Chronic metabolic acidosis decreases albumin synthesis and induces negative nitrogen balance in humans. J. Clin. Invest., 95(1): 39–45. http://dx.doi.org/10.1172/JCI117668
Barak, M., Rudin, M., Vofsi, O., et al., 2004. Fluid administration during abdominal surgery influences on coagulation in the postoperative period. Curr. Surg., 61(5): 459–462. http://dx.doi.org/10.1016/j.cursur.2004.02.002
Bell, P.D., Lapointe, J.Y., Cardinal, J., et al., 1989. Direct measurement of basolateral membrane potentials from cells of the macula densa. Am. J. Physiol., 257(3 Pt 2): F463–F468.
Bell, P.D., Komlosi, P., Zhang, Z.R., et al., 2009. ATP as a mediator of macula densa cell signalling. Purinergic Signal., 5(4): 461–471. http://dx.doi.org/10.1007/s11302-009-9148-0
Brandstrup, B., Tønnesen, H., Beier-Holgersen, R., et al., 2003. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann. Surg., 238(5): 641–648. http://dx.doi.org/10.1097/01.sla.0000094387.50865.23
Chowdhury, A.H., Cox, E.F., Francis, S.T., et al., 2012. A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and plasmalyte(R) 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann. Surg., 256(1): 18–24. http://dx.doi.org/10.1097/SLA.0b013e318256be72
Day, S.M., Westfall, M.V., Fomicheva, E.V., et al., 2006. Histidine button engineered into cardiac troponin I protects the ischemic and failing heart. Nat. Med., 12(2): 181–189. http://dx.doi.org/10.1038/nm1346
Day, S.M., Westfall, M.V., Metzger, J.M., 2007. Tuning cardiac performance in ischemic heart disease and failure by modulating myofilament function. J. Mol. Med., 85(9): 911–921. http://dx.doi.org/10.1007/s00109-007-0181-6
Debold, E.P., Beck, S.E., Warshaw, D.M., 2008. Effect of low pH on single skeletal muscle myosin mechanics and kinetics. Am. J. Physiol. Cell Physiol., 295(1):C173–C179. http://dx.doi.org/10.1152/ajpcell.00172.2008
Fujita, H., Ishiwata, S., 1999. Tropomyosin modulates pH dependence of isometric tension. Biophys. J., 77(3): 1540–1546. http://dx.doi.org/10.1016/S0006-3495(99)77001-3
Hansen, P.B., Jensen, B.L., Skott, O., 1998. Chloride regulates afferent arteriolar contraction in response to depolarization. Hypertension, 32(6): 1066–1070. http://dx.doi.org/10.1161/01.HYP.32.6.1066
Herrler, T., Tischer, A., Meyer, A., et al., 2010. The intrinsic renal compartment syndrome: new perspectives in kidney transplantation. Transplantation, 89(1): 40–46. http://dx.doi.org/10.1097/TP.0b013e3181c40aba
Ho, A.M.H., Karmakar, M.K., Contardi, L.H., et al., 2001. Excessive use of normal saline in managing traumatized patients in shock: a preventable contributor to acidosis. J. Trauma, 51(1): 173–177. http://dx.doi.org/10.1097/00005373-200107000-00033
Jensen, B.L., Ellekvist, P., Skott, P., et al., 1997. Chloride is essential for contraction of afferent arterioles after agonists and potassium. Am. J. Physiol., 272(3 Pt 2): F389–F396.
Kapur, S., Wasserstrom, J.A., Skøtt, O., 2009. Acidosis and ischemia increase cellular Ca2+ transient alternans and repolarization alternans susceptibility in the intact rat heart. Am. J. Physiol. Heart Circ. Physiol., 296(5): H1491–H1512. http://dx.doi.org/10.1152/ajpheart.00539.2008
Kellum, J.A., Song, M., Almasri, E., 2006. Hyperchloremic acidosis increases circulating inflammatory molecules in experimental sepsis. Chest, 130(4): 962–967. http://dx.doi.org/10.1378/chest.130.4.962
Kessler, R., Leibhammer, S., Laue, O., et al., 1997. Acute saline infusion induces extracellular acidification and activation of the Na+/H+ exchanger in man. Eur. J. Clin. Invest., 27(7): 558–565. http://dx.doi.org/10.1046/j.1365-2362.1997.1620711.xn
Koch, S.M., Taylor, R.W., 1992. Chloride ion in intensive care medicine. Crit. Care Med., 20(2): 227–240. http://dx.doi.org/10.1097/00003246-199202000-00012
Knuth, S.T., Dave, H., Peters, J.R., et al., 2006. Low cell pH depresses peak power in rat skeletal muscle fibres at both 30°C and 15°C: implications for muscle fatigue. J. Physiol., 575(Pt 3):887–899. http://dx.doi.org/10.1113/jphysiol.2006.106732
Levy, B., Collin, S., Sennoun, N., et al., 2010. Vascular hyporesponsiveness to vasopressors in septic shock: from bench to bedside. Intensive Care Med., 36(12): 2019–2029. http://dx.doi.org/10.1007/s00134-010-2045-8
Lobo, D.N., Dube, M.G., Neal, K.R., et al., 2001. Problems with solutions: drowning in the brine of an inadequate knowledge base. Clin. Nutr., 20(2): 125–130. http://dx.doi.org/10.1054/clnu.2000.0154
Lobo, D.N., Bostock, K.A., Neal, K.R., et al., 2002a. Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: a randomised controlled trial. Lancet, 359(9320): 1812–1818. http://dx.doi.org/10.1016/S0140-6736(02)08711-
Lobo, D.N., Dube, M.G., Neal, K.R., et al., 2002b. Perioperative fluid and electrolyte management: a survey of consultant surgeons in the UK. Ann. R. Coll. Surg. Engl., 84(3): 156–160.
Mitchell, J.H., Wildenthal, K., Johnson, R.L., et al., 1972. The effects of acid-base disturbances on cardiovascular and pulmonary function. Kidney Int., 1(5): 375–389. http://dx.doi.org/10.1038/ki.1972.48
Mitchell, K.D., Navar, L.G., 1988. Enhanced tubuloglomerular feedback during peritubular infusions of angiotensins I and II. Am. J. Physiol., 255(3 Pt 2):F383–F390.
Mitchell, K.D., Navar, L.G., 1990. Interactive effects of angiotensin II on renal hemodynamics and tubular reabsorptive function. Kidney Int. Suppl., 30:S69–S73.
Modi, M.P., Vora, K.S., Parikh, G.P., et al., 2012. A comparative study of impact of infusion of Ringer’s Lactate solution versus normal saline on acid-base balance and serum electrolytes during live related renal transplantation. Saudi J. Kidney Dis. Transpl., 23(1): 135–137.
Moopanar, T.R., Allen, D.G., 2005. Reactive oxygen species reduce myofibrillar Ca2+ sensitivity in fatiguing mouse skeletal muscle at 37°C. J. Physiol., 564(Pt 1):189–199. http://dx.doi.org/10.1113/jphysiol.2005.083519
Moopanar, T.R., Allen, D.G., 2006. The activity-induced reduction of myofibrillar Ca2+ sensitivity in mouse skeletal muscle is reversed by dithiothreitol. J. Physiol., 571(Pt 1):191–200. http://dx.doi.org/10.1113/jphysiol.2005.101105
Morimoto, S., Harada, K., Ohtsuki, I., et al., 1999. Roles of troponin isoforms in pH dependence of contraction in rabbit fast and slow skeletal and cardiac muscles. J. Biochem., 126(1): 121–129. http://dx.doi.org/10.1093/oxfordjournals.jbchem.a022412
O’Malley, C.M., Frumento, R.J., Hardy, M.A., et al., 2005. A randomized, double-blind comparison of lactated Ringer’s solution and 0.9% NaCl during renal transplantation. Anesth. Analg., 100(5): 1518–1524. http://dx.doi.org/10.1213/01.ANE.0000150939.28904.81
Oppermann, M., Mizel, D., Huang, G., et al., 2006. Macula densa control of renin secretion and preglomerular resistance in mice with selective deletion of the B isoform of the Na,K,2Cl co-transporter. J. Am. Soc. Nephrol., 17(8): 2143–2152. http://dx.doi.org/10.1681/ASN.2006040384
Oppermann, M., Mizel, D., Kim, S.M., et al., 2007. Renal function in mice with targeted disruption of the A isoform of the Na-K-2Cl co-transporter. J. Am. Soc. Nephrol., 18(2): 440–448. http://dx.doi.org/10.1681/ASN.2006091070
Powers, F., 1999. The role of chloride in acid-base balance. J. Intraven. Nurs., 22(5): 286–291.
Puljak, L., Kilic, G., 2006. Emerging roles of chloride channels in human diseases. Biochim. Biophys. Acta, 1762(4): 404–413. http://dx.doi.org/10.1016/j.bbadis.2005.12.008
Reid, F., Lobo, D.N., Williams, R.N., et al., 2003. (Ab)normal saline and physiological Hartmann’s solution: a randomized double-blind crossover study. Clin. Sci., 104(1): 17–24. http://dx.doi.org/10.1042/cs1040017
Ren, Y., Garvin, J.L., Liu, R., et al., 2004. Role of macula densa adenosine triphosphate (ATP) in tubuloglomerular feedback. Kidney Int., 66(4): 1479–1485. http://dx.doi.org/10.1111/j.1523-1755.2004.00911.x
Scheingraber, S., Rehm, M., Sehmisch, C., et al., 1999. Rapid saline infusion produces hyperchloremic acidosis in patients undergoing gynecologic surgery. Anesthesiology, 90(5): 1265–1270. http://dx.doi.org/10.1097/00000542-199905000-00007
Schotola, H., Toischer, K., Popov, A.F., et al., 2012. Mild metabolic acidosis impairs the β-adrenergic response in isolated human failing myocardium. Crit. Care, 16(4):R153. http://dx.doi.org/10.1186/cc11468
Shaw, A.D., Bagshaw, S.M., Goldstein, S.L., et al., 2012. Major complications, mortality, and resource utilization after open abdominal surgery: 0.9% saline compared to Plasma-Lyte. Ann. Surg., 255(5): 821–829. http://dx.doi.org/10.1097/SLA.0b013e31825074f5
Shires, G.T., Holman, J., 1948. Dilution acidosis. Ann. Intern. Med., 28(3): 557–559. http://dx.doi.org/10.7326/0003-4819-28-3-557
Snook, J.H., Li, J., Helmke, B.P., et al., 2008. Peroxynitrite inhibits myofibrillar protein function in an in vitro assay of motility. Free Radic. Biol. Med., 44(1): 14–23. http://dx.doi.org/10.1016/j.freeradbiomed.2007.09.004
Stewart, P.A., 1983. Modern quantitative acid-base chemistry. Can. J. Physiol. Pharmacol., 61(12): 1444–1461. http://dx.doi.org/10.1139/y83-207
Stone, H.H., Fulenwider, J.T., 1977. Renal decapsulation in the prevention of post-ischemic oliguria. Ann. Surg., 186(3): 343–355.
Tang, Y.B., Zhou, J.G., Guan, Y.Y., 2010. Volume-regulated chloride channels and cerebral vascular remodelling. Clin. Exp. Pharmacol. Physiol., 37(2): 238–242. http://dx.doi.org/10.1111/j.1440-1681.2008.05137.x
Traynor, T., Yang, T., Huang, Y.G., et al., 1998. Inhibition of adenosine-1 receptor-mediated preglomerular vasoconstriction in AT1A receptor-deficient mice. Am. J. Physiol., 275(6 Pt 2): F922–F927.
Uray, K.S., Shah, S.K., Radhakrishnan, R.S., et al., 2011. Sodium hydrogen exchanger as a mediator of hydrostatic edema-induced intestinal contractile dysfunction. Surgery, 149(1): 114–125. http://dx.doi.org/10.1016/j.surg.2010.04.001
Veech, R.L., 1986. The toxic impact of parenteral solutions on the metabolism of cells: a hypothesis for physiological parenteral therapy. Am. J. Clin. Nutr., 44(4): 519–551.
Veizis, I.E., Cotton, C.U., 2007. Role of kidney chloride channels in health and disease. Pediatr. Nephrol., 22(6): 770–777. http://dx.doi.org/10.1007/s00467-006-0355-4
Waters, J.H., Gottlieb, A., Schoenwald, P., et al., 2001. Normal saline versus lactated Ringer’s solution for intraoperative fluid management in patients undergoing abdominal aortic aneurysm repair: an outcome study. Anesth. Analg., 93(4): 817–822. http://dx.doi.org/10.1097/00000539-200110000-00004
Wilcox, C.S., 1983. Regulation of renal blood flow by plasma chloride. J. Clin. Invest., 71(3): 726–735. http://dx.doi.org/10.1172/JCI110820
Wilkes, N.J., Woolf, R., Mutch, M., et al., 2001. The effects of balanced versus saline-based hetastarch and crystalloid solutions on acid-base and electrolyte status and gastric mucosal perfusion in elderly surgical patients. Anesth. Analg., 93(4): 811–816. http://dx.doi.org/10.1097/00000539-200110000-00003
Williams, E.L., Hildebrand, K.L., McCormick, S.A., et al., 1999. The effect of intravenous lactated Ringer’s solution versus 0.9% sodium chloride solution on serum osmolality in human volunteers. Anesth. Analg., 88(5): 999–1003. http://dx.doi.org/10.1213/00000539-199905000-00006
Yunos, N.M., Bellomo, R., Story, D., et al., 2010. Bench-tobedside review: chloride in critical illness. Crit. Care, 14(4):226. http://dx.doi.org/10.1186/cc9052
Zand, L., King, B.F., Qian, Q., 2014. Role of kidney Doppler ultrasonography in the diagnosis and management of anuric kidney failure. Clin. Nephrol., 82(2): 122–127. http://dx.doi.org/10.5414/CN107765
Acknowledgements
The authors are grateful for the support of the ISN Sister Renal Center Program. This topic was presented in 2015 at one of the Sister Renal Center conferences.
Author information
Authors and Affiliations
Corresponding author
Additional information
The two authors contributed equally to this work
ORCID: Qi QIAN, http://orcid.org/0000-0002-1735-2657
Rights and permissions
About this article
Cite this article
Li, H., Sun, Sr., Yap, J.Q. et al. 0.9% saline is neither normal nor physiological. J. Zhejiang Univ. Sci. B 17, 181–187 (2016). https://doi.org/10.1631/jzus.B1500201
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1631/jzus.B1500201