Introduction
Temporomandibular joint (TMJ) disorder is a disease in which the temporomandibular joint becomes inflamed or dislocated and jaw movement is restricted due to pain [1,2]. Injuries caused by external causes and various physiological and pathological factors are causes of TMJ disorder. Inappropriate habits such as teeth grinding and clenching due to stress are also driving the increase of this disorder [3]. It has been reported that about 30% of the total population have TMJ noise during opening and closing of the mouth and that 5~7% of them require treatment [4]. As a result of data analysis from National Health Insurance Service, the number of patients with TMJ disorder (K07.6) was increased from 391,168, in 2017 to 473,513 in 2021, an increase of 21% (annual average of 4.2%) in 5 years [5]. Total medical expenses due to TMJ disorder has also increased by 47.3% over 5 years (31,106 million won in 2015 to 45,834 million won in 2019). In particular, about 30% of the patients with TMJ disorder were in their 20s.
The initial TMJ disorder can be improved by eliminating oral habits (bruxism, clenching, etc.) that affect the TMJ. However, once the disorder becomes chronic, physical therapy is needed in the concept of rehabilitation to help its treatment by relaxing muscles around the TMJ and reducing pain [6,7]. With the revision of the medical law in 2014, dentists can directly perform physical therapy. The number of dental hospitals specializing in physical therapy is increasing [8]. The number of dental hospitals receiving certification for TMJ stimulation therapy by the Health Insurance Review and Assessment Service in 2022 has doubled over the past five years compared to about 2,000 in 2017. Hospital certification is expected to expand in the future. Therefore, dental hygienist need to have an enhanced knowledge of dental physiotherapy. However, most of the 84 universities (college) with dental hygiene majors’ program (in 2020; 28 4-year bachelor, 56 3-year bachelor) do not offer dental physiotherapy-related curriculum. Some of them have limited theories in oral medicine courses.
In this study, dental hygienists working in clinical practice were surveyed about the importance of dental physical therapy, the need for related education, and prospects. Through this survey, the need for education of dental hygienists about dental physical therapy was elucidated.
Methods
1. Subjects and data collection
This study conducted a survey of dental hygienists working in clinical dental hospital. The subjects were selected by convenience sampling. Through dental hygienists certified online community platform, URL links and QR codes were provided from Dec. 2021 to Jan. 2022. The code of research ethics was followed in accordance with the standard form provided by the 00 university. After being provided the purpose of the study, only subjects who voluntarily agreed to the questionnaire participated in the study by checking the online consent question. A total of 143 people responded, of which 140 responses were applied to the final analysis, excluding missing values of major variables (n=1) and 2 respondents for reasons such as response bias written with the same number. The present study was approved by the Institutional Review Board of 00 University (IRB No. EU22-26).
2. Materials
A simple and clearly structured questionnaire was used in order to increase response rate. The questionnaire consisted of 4 main questions and its sub-questions. The 4 main questions are general characteristics, experience of dental physiotherapy work, the importance of physiotherapy work performance and the need for physical therapy education for dental hygienist. General characteristics include educational attainment (college, 4-year bachelor, master and doctoral degree), years of clinical career, types of medical institution (dental clinic, dental hospital, others). In addition to the experience of dental physiotherapy work, as its sub-questions, accreditation hospital for temporomandibular joint stimulation therapy was investigated. Educational needs for physical therapy for dental hygienist were asked along with the appropriate way of learning as its sub-questions.
3. Statistical analysis
The collected data were analyzed using IBM SPSS program (ver. 28.0; IBM Corp., Armonk, NY, USA) statistical program. All statistics were expressed as frequencies and percentages for categorical variables. A p≤0.05 was considered statistically significant.
Results
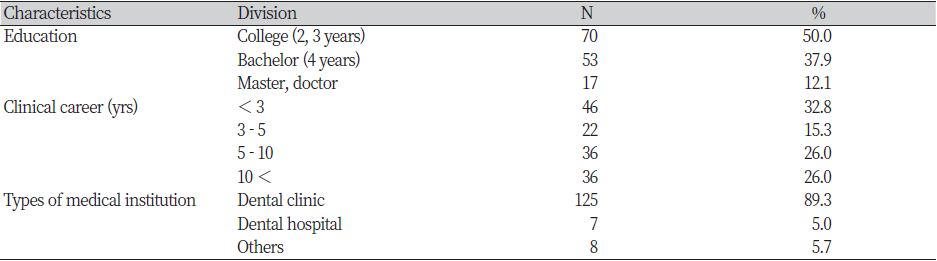
A total of 140 dental hygienists in clinical practice participated in this study, including 70 (50%) individuals with a 3-year Bachelor’s degree, 53 (37.9%) individuals with a 4-year Bachelor’s degree, and 17 (12.1%) individuals with a Master’s or Doctoral degree. Those with less than 10 years of clinical work experience accounted for 74% of the total participants and those with more than 10 years accounted for 26%. Local clinic workers constituted most (89.3%) of the respondents <Table 1>.
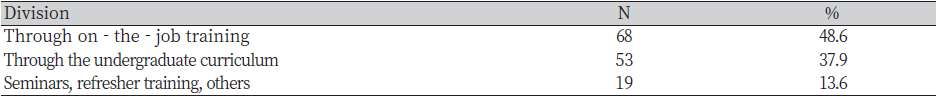
Among them, 49.3% of dental hygienists experienced dental physiotheraphy work and 45% of hospitals they were working for were certified hospitals for TMJ stimulation therapy <Table 2>. It can be seen that this survey includes a lot of respondents who have experience of dental physiotheraphy work in certified hospitals for TMJ stimulation therapy.
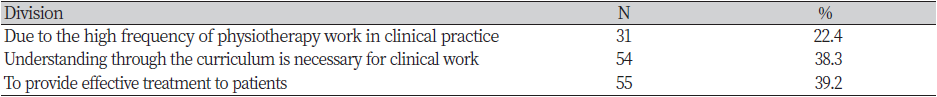
Regarding dentistry, only 11.4% of participants had the opinion that physiotheraphy work was not important, whereas the majority (88.6% of total) of participants had the opinion that ‘dental physiotherapy work is important’ (35.7%) and that ‘dental physiotherapy work will become more important in the future’ (52.9%). A high percentage (84.3%) of participants agreed with the opinion that ‘dental hygienists need physical therapy education’ <Table 3>. This result means that even dental hygienists without experience in physiotheraphy work (50.7%) perceive that related education is necessary due to the importance of physiotheraphy work in dentistry. Regarding dental hygiene education courses, through on-the-job training (48.6%), through undergraduate curriculum (37.9%), and seminar, refresher training, and others (13.6%) were suggested as methods to acquire dental physical therapy education <Table 4>. Reasons why dental physiotherapy education would be needed for dental hygienists included ‘to provide effective treatment to patients’ (39.2%), ‘understanding through the curriculum is necessary for clinical work’ (38.3%), and ‘due to the high frequency of physiotherapy work in clinical practice’ (22.4%) <Table 5>.
|
Table 2. Experience of dental physiotherapy work and accreditation hospital for temporomandibular joint stimulation therapy (N=140) 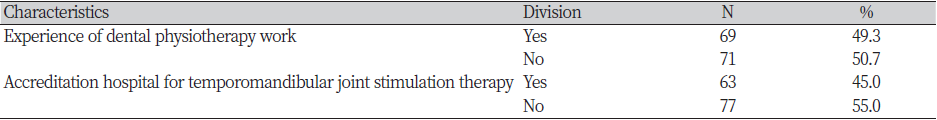
|
|
Table 3. The importance of physiotherapy work performance in dentistry and the need for physical therapy education for dental hygienists (N=140) 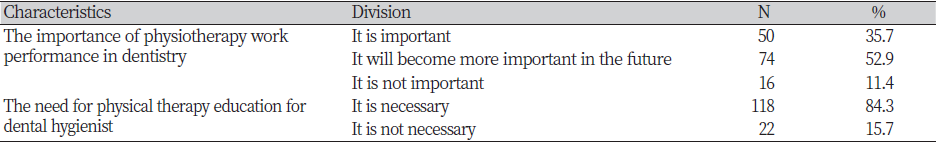
|
Discussion
TMJ disorder is regarded as a chronic musculoskeletal disease because it is often caused by long-term bad oral habits such as bruxism and clenching. Arthritis in the elderly is also a cause [1,2,9]. Therefore, continuous physical therapy is necessary to prevent and treat it. Even if irreversible treatments such as occlusal adjustment, prosthetic restoration, orthodontic treatment, and TMJ surgery are in progress, physical therapy for rehabilitation should be accompanied for a long time. Physical therapy performed reversibly in dentistry can relieve pain and help restore function by relaxing muscles and increasing tissue fluid and blood circulation. Hyperthermia (surface and deep heat therapy), cooling therapy, electrotherapy (galvanic stimulation, iontophoresis, percutaneous nerve stimulation, electroacupuncture), and laser therapy (GaAIAs semiconductor low-power laser, Nd:YAG laser, CO2 laser stimulation) are typical physical therapy options in dentistry [10].
TMJ physiotherapy options include spay and stretch therapy, TMJ manipulation therapy, closed reduction of TMJ dislocation, and TMJ stimulation therapy [7]. Among these, TMJ stimulation such as TMJ simple stimulation therapy, TMJ electrical stimulation therapy, and TMJ complex stimulation therapy (including temporomandibular disorder exercise therapy, low-level laser therapy, biofeedback, iontophoresis therapy, trigger point injection stimulation therapy) requires Health Insurance Review and Assessment Service certification [11]. Dentists must complete training in the field of facial pain, have a treatment room of a certain area and equipment to be used, and must be certified by the Health Insurance Review and Assessment Service through the Korean Dental Association to perform TMJ stimulation therapy [12]. Although continuing education is being actively conducted at the Oral Medicine academy and the temporomandibular joint and facial pain-related societies for practicing dental physical therapy and clinic certification, the dental hygiene curriculum has very limited content on physical therapy. Therefore, it is important to discuss the necessity of the relevant curriculum in depth with urgency. Lack of undergraduate education can affect dental hygienists' clinical practice.
Half of the participants in this study had experience working in the field of physical therapy in dentistry that obtained TMJ stimulation therapy certification. In terms of clinical work, 88.6% of participants agreed that physical therapy work is important and will become more important in the future. Even a dental hygienist with no experience in physical therapy predicted that dental physical therapy would be important in dental care in the future. In terms of education, 84.3% agreed with the opinion that physical therapy education is necessary for dental hygienists. Even dental hygienists with no experience in physical therapy recognized the need for related education for dental hygienists because of the importance of physical therapy work in dentistry. In particular, the need for dental physiotherapy education was high to effectively respond to dental physiotherapy works. Despite the high educational requirements, dental physiotherapy-related practices were acquired during clinical work. The main reason is that the content of dental physiotherapy is not reflected in the dental hygiene education curriculum. Although the content of dental physiotherapy is reflected in a part of the oral medicine course for dental hygienists, it is very limited, such as hyperthermia (superficial and deep hyperthermia), cooling therapy, and laser therapy [13]. This may limit the effective response of dental hygienists to dental physiotherapy works. In addition, for effective dental physiotherapy education for dental hygienists, the necessity for clinic practice (48.6%) as well as undergraduate course (37.9%) was suggested. Therefore, the necessity of reflecting dental physiotherapy in the dental hygiene education curriculum for improving clinical work efficiency of dental hygienists was derived from the results of this study. Dentists may legally hire physical therapists to guide their work in dental clinic [8]. However, since physical therapy performed in dentistry is a part of the overall treatment, and physical therapists cannot cope with duties of a dental hygienist, the implementation of dental physical therapy through employment of physical therapists at local clinics is clearly limited. Considering the expansion of TMJ physiotherapy certificated hospitals, reflecting dental hygienist's major curriculum for dental physiotherapy should also be considered to improve clinical practice. In addition, considering that most dental physical therapy training is acquired during clinical work, it will be necessary to specify the scope of dental physical therapy performance by dental hygienists in the Medical Technician Act along with the necessity of dental physical therapy training for dental hygienists.
The results of this study suggest that there is a need to provide dental physiotherapy-related education through various methods including undergraduate education for effective clinical work performance of dental hygienists. The opinion of dentists on the necessity of dental physiotherapy education for dental hygienists is also very important. The number of dental physiotherapy clinics certified by the Health Insurance Review and Assessment Service is increasing [8]. It is thought that the educational content that dentists require of dental hygienists to cope with dental physiotherapy has changed. In addition, the clear mechanism for dental physiotherapy is still incomplete. Information on new and various physical therapy tools is not reflected in the education of dental hygienists either.
This study has some limitations. First, as a cross-sectional study design and a questionnaire tool consisting of very simple questions, it is difficult to prove the reliability of the tool. Second, various covariates that affect the response such as region and number of medical personnel were not considered. In further study, the development of a reliable survey tool for education needs should be prioritized.
Conclusions
To investigate the status of dental physiotherapy work and the need for education of dental hygienists, a total of 140 dental hygienists working in clinical dental hospital were analyzed consisting of questions asking about general characteristics, experience of dental physiotherapy work, the importance of physiotherapy work performance and the need for physical therapy education for dental hygienist.
1. Half of the study participants had experience of working in dental physiotherapy.
2. Of 140 participants, 88.6% agreed with the opinion that ‘physical therapy work is important or that it will become important’.
3. 84.3% agreed with the opinion that ‘physical therapy education is necessary for dental hygienists’.
In the present study, the awareness and education requirements for dental physical therapy were identified for dental hygienists in clinics. Results of this study could be used as reference data for expanding the education of dental physiotherapy to improve clinical practice of dental hygienists.