Published online Nov 26, 2021. doi: 10.12998/wjcc.v9.i33.10374
Peer-review started: August 12, 2021
First decision: September 2, 2021
Revised: September 8, 2021
Accepted: September 30, 2021
Article in press: September 30, 2021
Published online: November 26, 2021
Despite being the most common intraocular malignancy among adults, choroidal melanoma is a rare cancer type, even more so when accompanied by lung cancer. We report a patient with synchronous choroid melanoma and lung cancer treated with carbon ion radiotherapy (CIRT).
A 41-year-old woman was transferred to our center with a diagnosis of choroidal melanoma in her right eye. During the examination, we found a right lung tumor that was histologically diagnosed as lung cancer. The patient was treated with CIRT for both malignant neoplasms. The CIRT dose was 70 photon equivalent doses (GyE) in five fractions for the right eye choroidal melanoma and 72 GyE in 16 fractions for the right lung cancer. At 3 mo after CIRT, the choroidal melanoma completely disappeared, as did the right lung cancer 7 mo after; the patient was in complete remission.
CIRT may be an effective treatment for double primary lung cancer and choroid melanoma.
Core Tip: Simultaneous choroidal melanoma and lung cancer are extremely rare. This report details a case of a 41-year-old woman with right-side choroidal melanoma and lung cancer treated with carbon ion radiotherapy. Seven months after treatment, the patient was in complete remission.
- Citation: Zhang YS, Hu TC, Ye YC, Han JH, Li XJ, Zhang YH, Chen WZ, Chai HY, Pan X, Wang X, Yang YL. Carbon ion radiotherapy for synchronous choroidal melanoma and lung cancer: A case report. World J Clin Cases 2021; 9(33): 10374-10381
- URL: https://www.wjgnet.com/2307-8960/full/v9/i33/10374.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i33.10374
Uveal melanoma is the most common primary ocular malignancy among adults[1] and is treated with conventional surgery or various radiotherapy techniques[2,3]. The most common radiotherapy modalities are plaque brachytherapy and proton radiotherapy (PRT)[4-6]. However, carbon ion beams conform to the prescribed dose better than proton beams because of a sharper lateral falloff. Carbon ion beams are also bio
We present a case of concurrent choroidal melanoma and lung cancer that was successfully treated with CIRT. This report follows the CARE Guidelines: Consensus-based Clinical Case Reporting Guideline Development[11].
A 41-year-old woman was referred to the Wuwei Heavy Ion Center in June 2020 with choroidal melanoma of her right eye.
The right eye melanoma was histologically confirmed via fine-needle aspiration biopsy at an eye hospital. Written informed consent was obtained from the patient for publication.
The immunohistochemical profile was C-erbB-2 (-), CK7 (+), Ki-67 (index = 25 %), Napsin A (+), P63 (-), and TTF-1 (+).
Computed tomography (CT) and magnetic resonance imaging (MRI) demonstrated that the tumor was located on the cranial side of the right eye. The patient presented with right eye malaise with gradual diminution of vision in the right eye over a period of 2 mo. After being transferred to our center, the patient's vision rapidly worsened, and she became completely blind in 15 d.
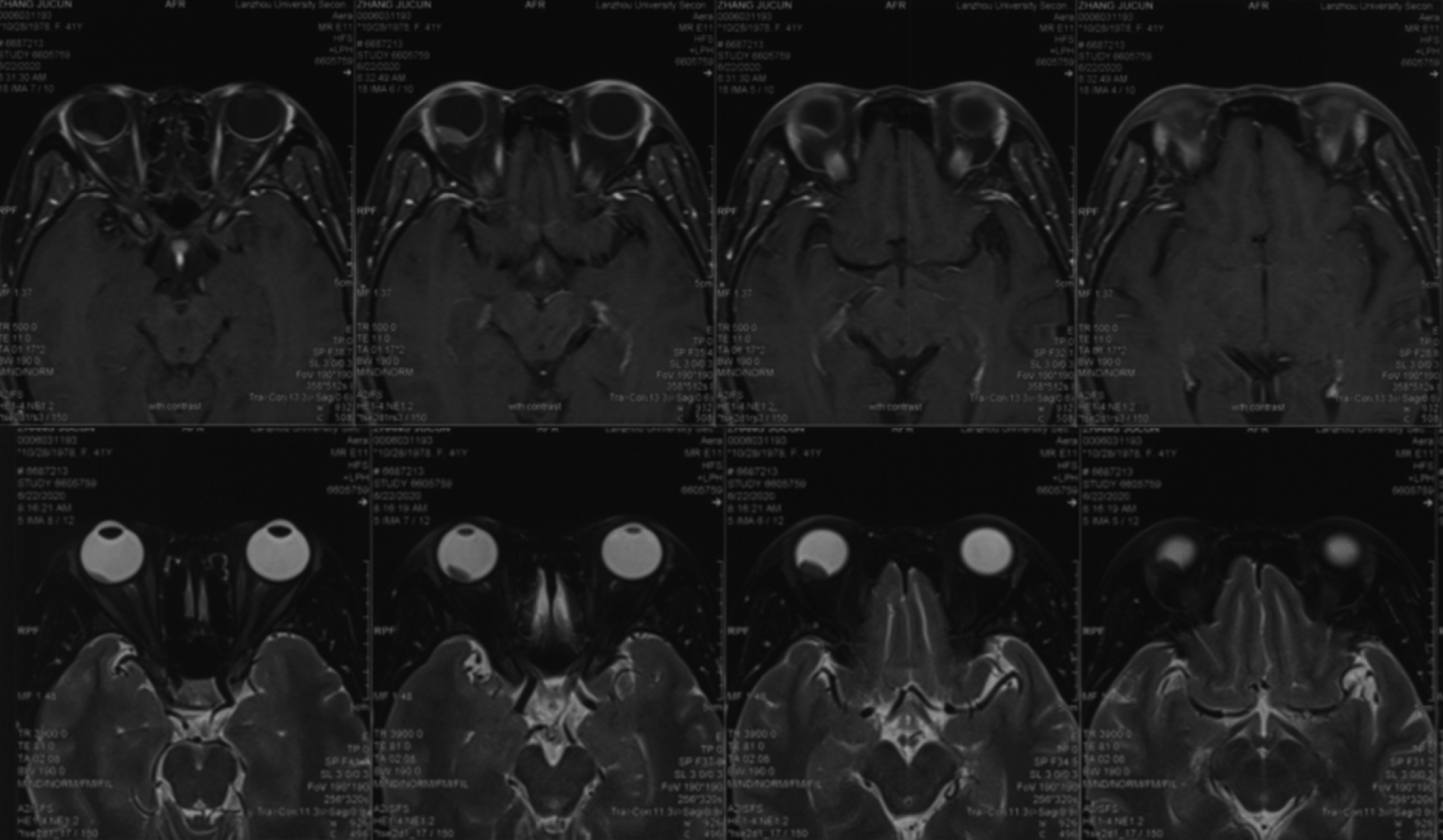
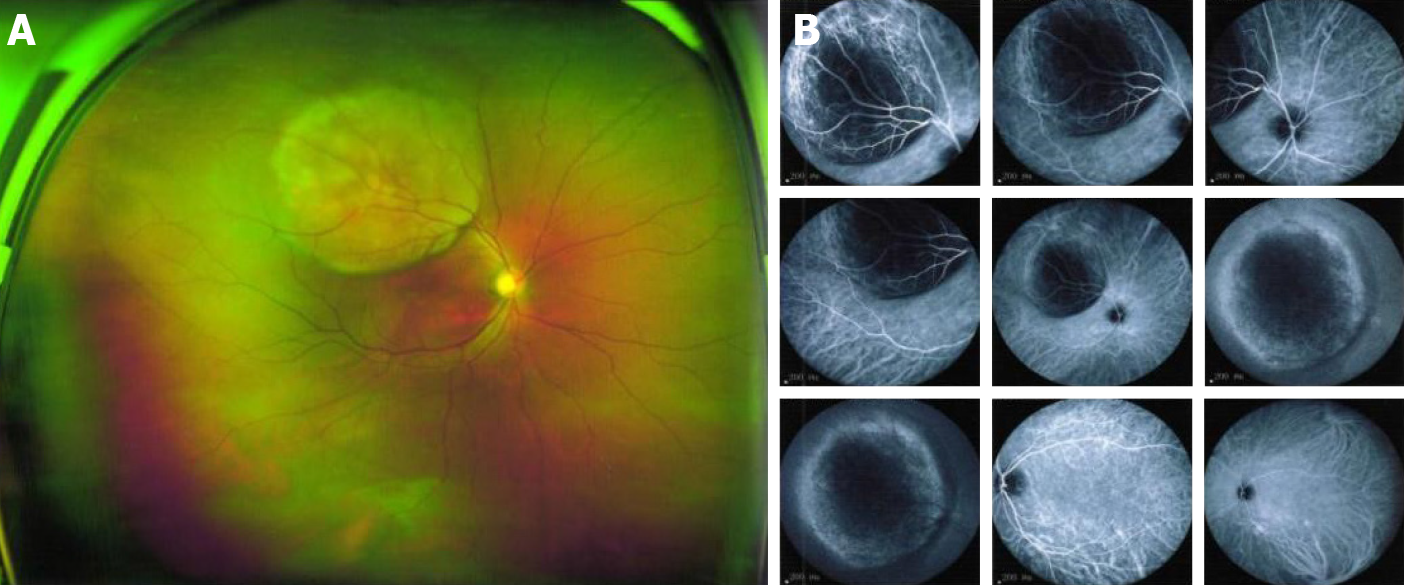
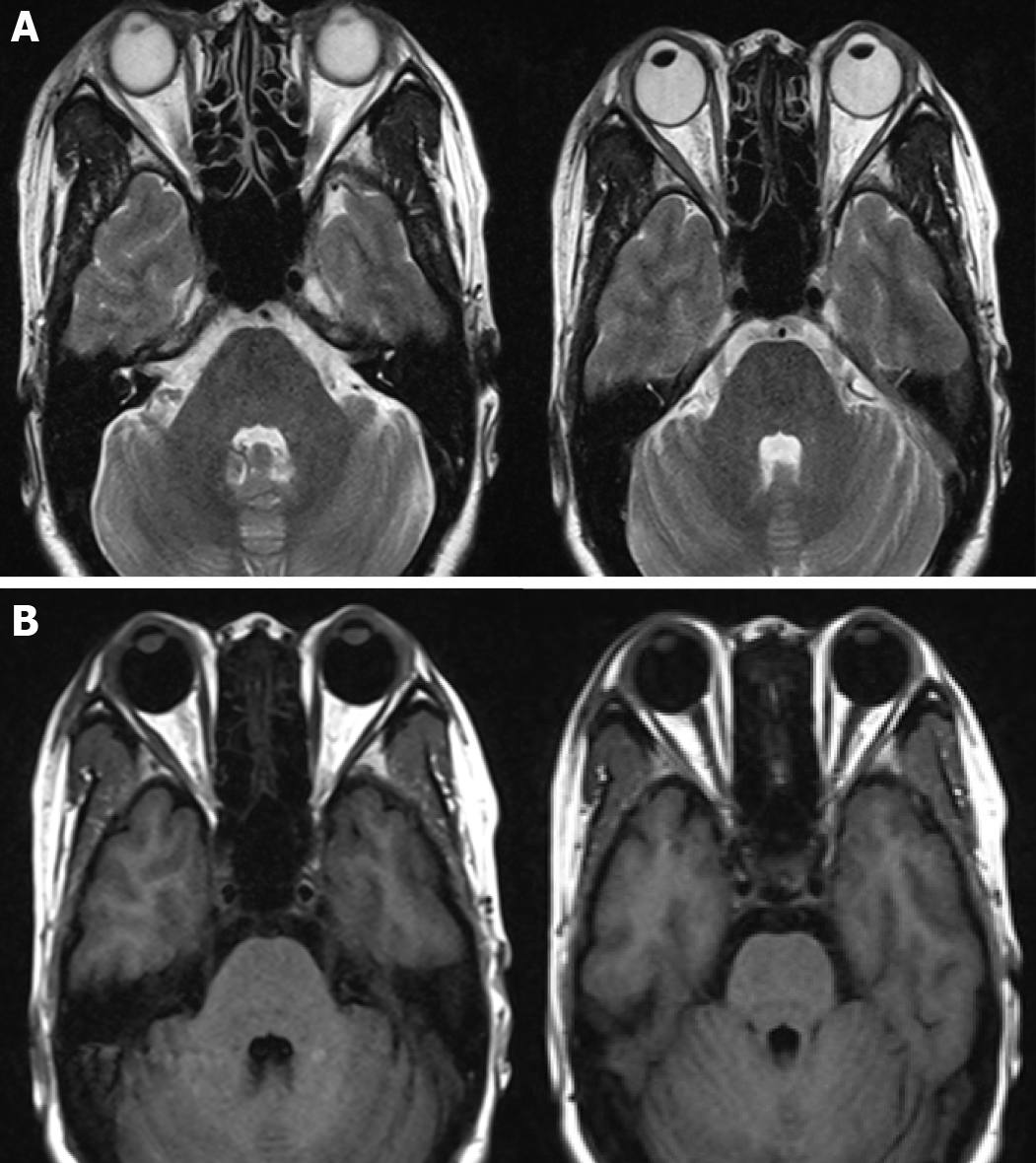
The patient underwent MRI at our hospital (3.0T; Siemens), which identified a lesion behind the right eye bulb from abnormal T1- and T2-weighted signals and high intensity on diffusion-weighted images (Figure 1). Ophthalmoscopy of the right eye showed a solid dark-gray mass in the posterior segment of the choroid with intense brown pigmentation occupying the posterior third of the vitreous chamber and mild retinal detachment at the peripheral choroidal mass rim. The mass was dome-shaped, 11.1 mm × 12.1 mm in size, and occupied a third of the posterior segment of the right eye (Figure 2). During the examination, a tumor in the lower lobe of the right lung was also observed. A multidisciplinary team discussion concluded that double primary neoplasms, ocular metastasis of lung cancer, and ocular melanoma with lung metastasis were possibilities. Subsequently, the patient underwent a lung biopsy, which indicated infiltrating acinar adenocarcinoma.
The final histologically confirmed diagnoses were: (1) choroidal melanoma of the right eye, cT2N0M0 [per the American Joint Committee on Cancer (AJCC) 8th edition]; and (2) right-sided lung cancer, infiltrating acinar adenocarcinoma, cT3N0M0, IIb (per the AJCC 8th edition), KPS: 90. CIRT for lung and eye cancer was planned after discussion with the patient and family.
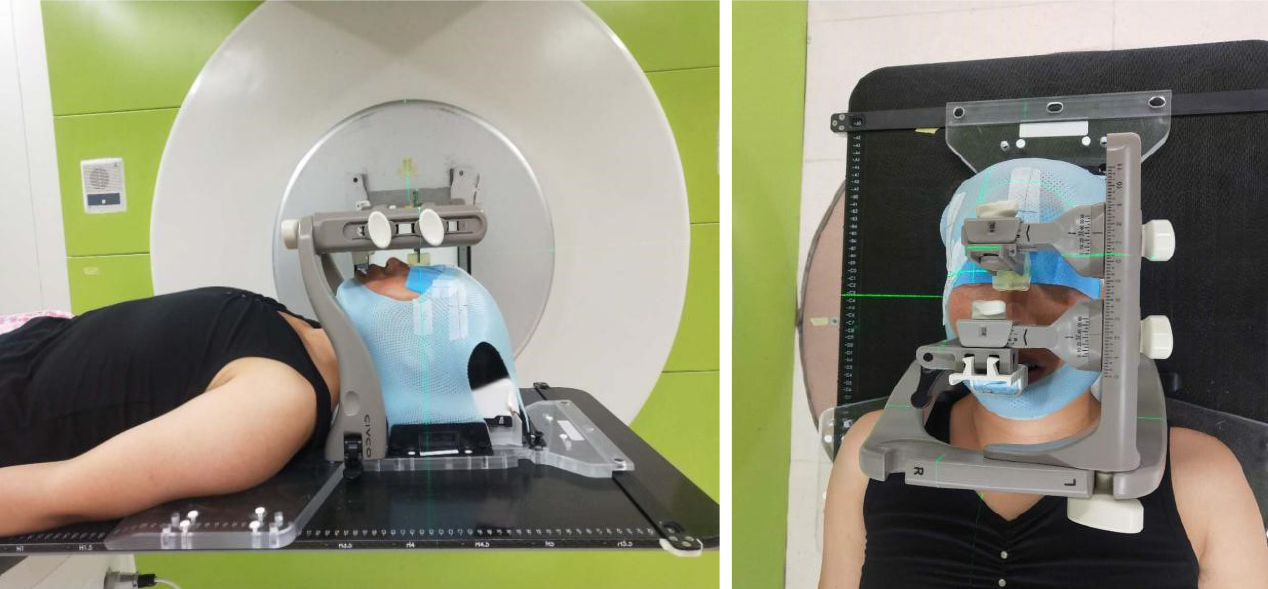
First, we treated the right eye tumor. The patient was immobilized in a supine position with a bite block device (trUpoint ARCH; CIVCO, Orange City, IA, United States) (Figure 3). A set of 1-mm thick CT images was obtained using a CT simulator. Gross tumor volume (GTV) was determined using CT images and referencing the ophthalmoscopy and MRI findings. Clinical target volume (CTV) was the GTV plus 1 mm, and planning target volume (PTV) was the CTV plus a 1.0-mm margin. CIRT was performed with the anterior and right lateral portals. The total prescribed dose was 70.0 photon equivalent doses (GyE) in 5 fractions (Fx; 2 Fxs from the anterior portal and 3 Fxs from the right lateral portal) once daily, five times per week (Monday to Friday). Carbon ion doses were expressed in GyE, defined as the physical dose multiplied by the relative biological effectiveness (RBE) of the carbon ions, which was assumed to be 3.0[12].
After completing CIRT for choroidal melanoma, we continued with treating the right-sided lung cancer. The patient was immobilized in the prone position using a customized vacuum cushion and chest thermoplastic mask. CT images were obtained using four-dimensional CT (4DCT) with 3-mm thick images. GTV was delineated based on the 4DCT images, CTV was defined as GTV plus 5 mm, ITV was defined as CTV plus the tumor motion on the 4DCT images, and PTV was expanded by 5 mm based on ITV. The CIRT plan delivered 72 GyE to the target volume in 16 Fx using the broad-beam method once daily, five times per week (Monday to Friday).
CIRT was planned using the carbon ion plan (ciPlan, version 1.0; IMP, Lanzhou, China). Treatment planning included a biologic treatment plan optimization procedure using the carbon ion Treat Plan (ciTreat) (version 1.0, IMP) treatment planning software system that considers local RBE values calculated by the ciPlan software based on the mixed beam model.
Efficacy evaluation was performed based on the Response Evaluation Criteria in Solid Tumours version 1.1 guidelines. The Common Terminology Criteria for Adverse Events (CTCAE) version 5.0 guidelines were used to evaluate adverse events. The Radiation Therapy Oncology Group (RTOG) acute radiation injury classification criteria were used to evaluate radiation damage. During and after CIRT, there were only grade 1 adverse events and no grade ≥ 2 RTOG acute effects.
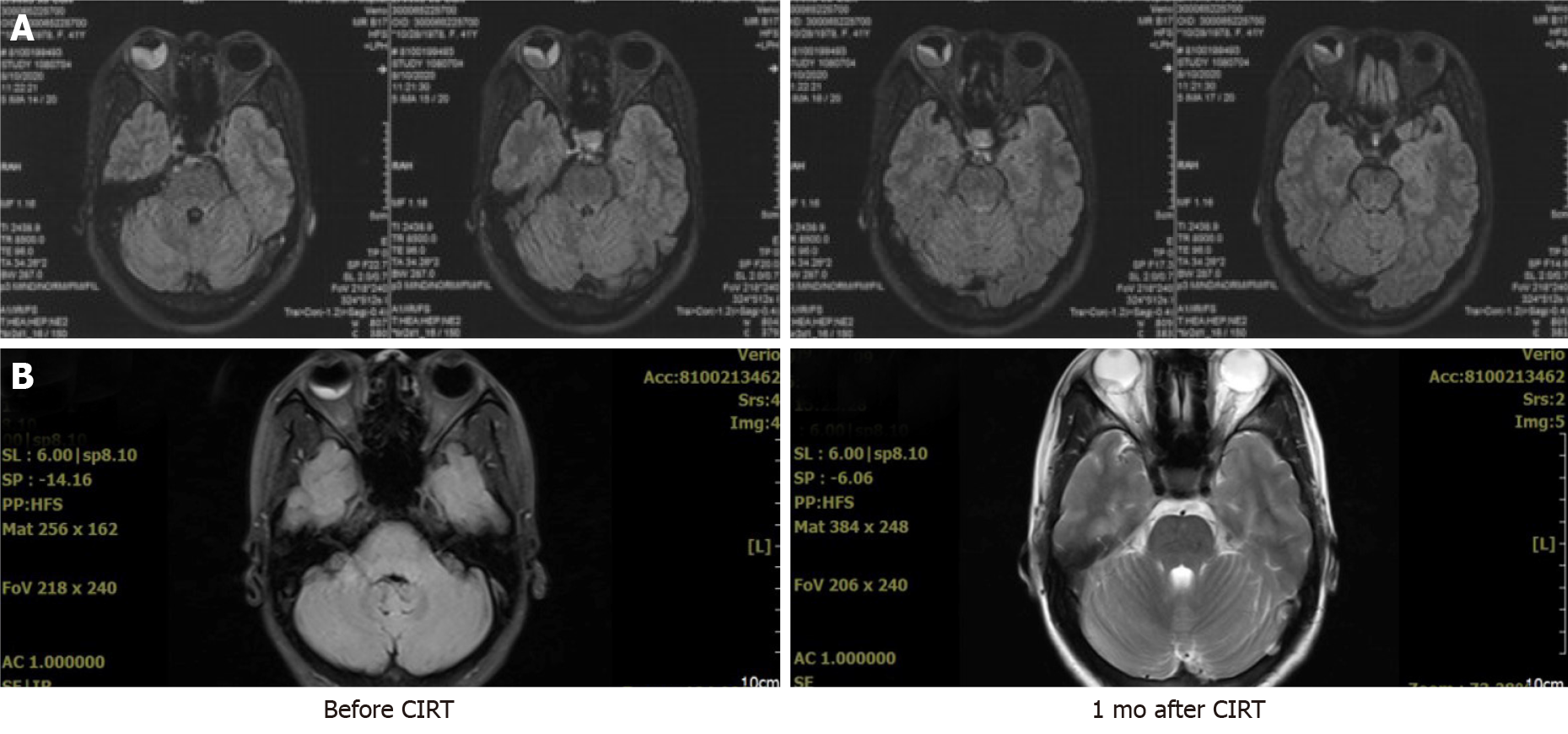
Ophthalmic examination before CIRT revealed complete loss of vision in the right eye. One month after CIRT, the patient’s right eye began to perceive light and continued to gradually improve. Table 1 presents findings of the ophthalmic examination. After 3 CIRT Fxs, mild right eye edema occurred. Upon CIRT completion, MRI demonstrated that the melanoma increased, with obvious retinal detachment (Figure 4A). One month after CIRT, the choroid tumor was smaller, and the retinal detachment was resolved (Figure 4B). Three months after CIRT, the right eye choroid tumor disappeared completely, achieving complete remission (CR) (Figure 5). The patient’s right eye vision slowly returned (Table 1).
| Right | Left | |||
| VOD | IOP, mmHg | VOS | IOP, mmHg | |
| Before CIRT | HM/30 cm | 9.8 | 1.0 | 16.4 |
| 1 mo after CIRT | Light perception | 13.9 | 1.0 | 18.8 |
| 2 mo after CIRT | Hand motions | 11.0 | 0.8 | 18.2 |
| 4 mo after CIRT | 0.02 | 14.0 | 1.0 | 15.2 |
| 6 mo after CIRT | 0.04 | 13.0 | 1.0 | 16.0 |
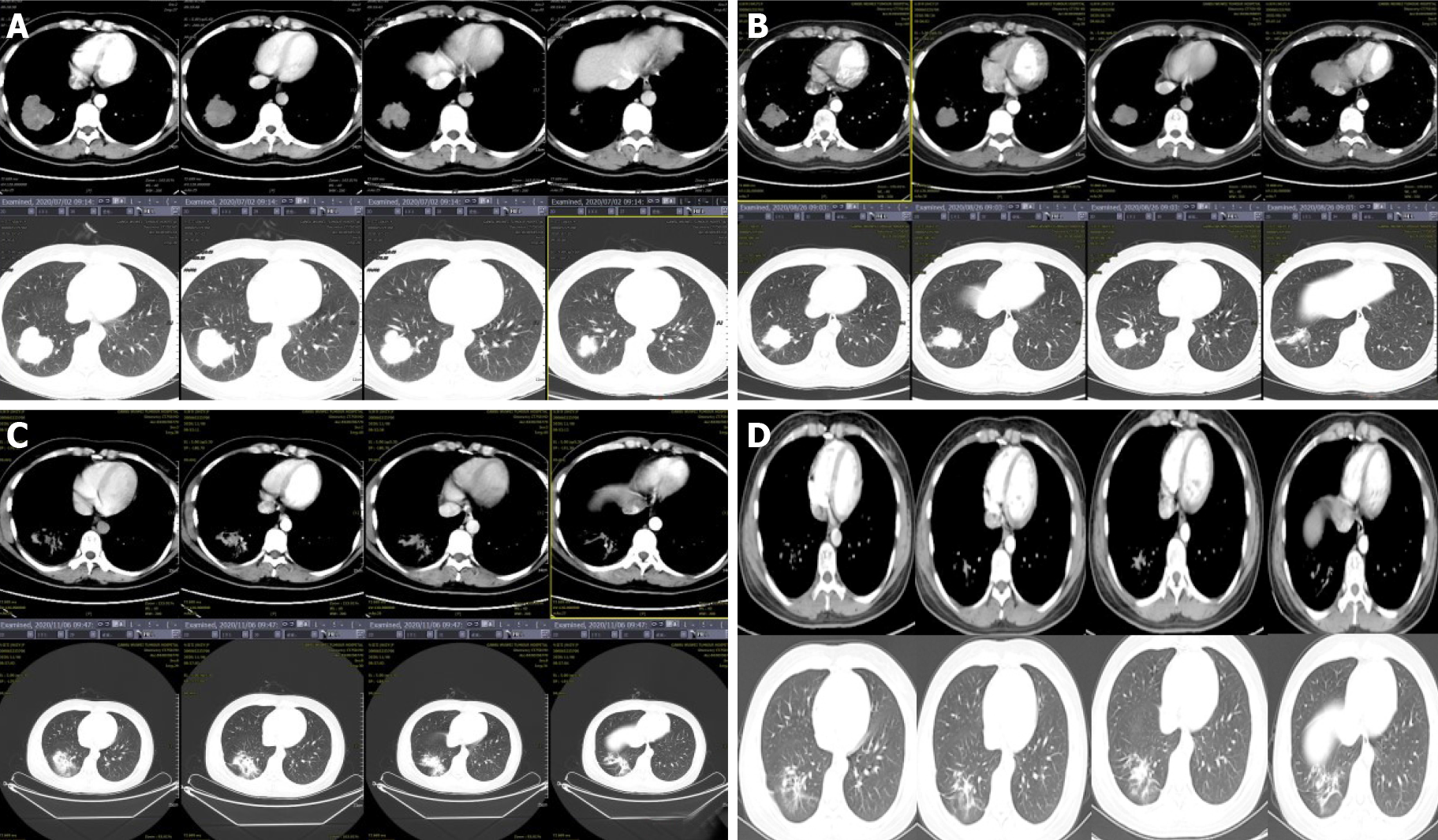
Before CIRT, the lung cancer size was 4.7 cm × 5.2 cm. After CIRT, it regressed to 4.2 cm × 3.5 cm after 1 mo, 3.6 cm × 2.5 cm after 3 mo, and completely disappeared after 7 mo, with only a small area of pulmonary fibrosis, also achieving CR (Figure 6). The CTCAE evaluation showed grade 1 radiation dermatitis and right eye edema.
We recommended that the patient receive chemotherapy and immunotherapy because of the high risk of metastasis from the two lesions. However, out of economic consideration, the patient refused further treatment and expressed that they and their family were content with the results, which already exceeded their expectations. The patient felt very satisfied with the CIRT treatment. Seven months after completing CIRT, the patient’s right eye vision was still weak, but no other treatment-related side effects were observed, and the patient felt good.
A middle vascular pigmented layer, including the iris, ciliary body, and choroid, comprises the uvea of the eye[13], and uveal tract melanomas are anterior or posterior tract lesions. Anterior tract melanomas involve the iris, and posterior tract melanomas involve the ciliary body and the choroid layer. Malignant uvea melanomas are more common in the choroid and ciliary body than in the iris.
Melanomas are highly malignant cancers[14]. There are several histological subgroups with various degrees of aggressive behavior and systemic metastases risk. Cytogenetic features, such as chromosome 3 monosomy and the mutations in the GNAQ and BAP1 genes, are also related to higher aggressiveness and systemic spread. Recently, PALB2 and MLH1 germline mutations were associated with a hereditary predisposition to the risk of uveal melanoma, and several other genes also have potential associations with uveal melanomas[15]. The clinical presentation of uveal melanoma relies on the mass location within the uveal tissue, size, pigmentation, associated bleeding, retinal detachment, inflammation, and extrascleral extension. Most patients experience decreased visual acuity and blurred vision[1]. Although there are many cutting-edge treatment techniques, visual prognosis is usually poor, and many patients develop functional blindness in the affected eye. Further, metastasis to the liver and other organs is a primary cause of death despite recent advances in medical therapy[16].
Most patients with uveal melanoma undergo enucleation. Globally, a relatively small population of patients receive some form of radiotherapy. The most common radiotherapy modalities for uveal melanoma are plaque brachytherapy and PRT. Brachytherapy is effective for small-to-medium-sized uveal melanomas with thicknesses of less than 7 mm, whereas PRT is used when the uveal melanoma is larger or closer to the optic disc or fovea, taking advantage of the Bragg peak and biological profile. Newer techniques, such as stereotactic radiosurgery with CyberKnife, achieve similar local control rates with eye retention to PRT but have a poorer post-treatment visual prognosis[17]. Carbon ion beams have unique physical and biological properties that make high-precision, high linear energy transfer (LET) radiotherapy[12]. For choroidal melanoma, high-dose radiation with excellent dose conformity is necessary for optimal results, similar to PRT and plaque brachytherapy. Therefore, we expected that CIRT was suitable for treating this tumor. Moreover, the high LET characteristics of carbon ions make it an effective treatment that is likely to achieve comparable tumor control with a lower dose than PRT. NIRS results have demonstrated that for choroidal melanoma, CIRT is at least comparable to PRT[18,19].
Multiple primary malignant neoplasms indicate the simultaneous presence of two or more primary malignancies of different histological types in the same patient, which can affect multiple tissues and organs[20]. Currently, the most accepted criteria for diagnosing primary malignant tumors are that each tumor should be histologically confirmed as malignant, occur in different parts or organs, differ regarding the histological, cytological, and morphological features and immunohistochemical phenotypes, and the possibility that one tumor is the metastasis of another must be completely excluded clinically, radiologically, and pathologically[21].
We report a case of synchronous lung cancer and choroid melanoma. Both lesions were treated with CIRT, resulting in their complete resolution. The patient is currently experiencing relapse-free survival 7 mo after completing CIRT. The treatment outcome suggests that CIRT is an effective option for synchronous double primary lung cancer and choroid melanoma, and favorable results are likely.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pandit PN S-Editor: Wang JL L-Editor: Filipodia P-Editor: Wang JL
| 1. | Singh AD, Bergman L, Seregard S. Uveal melanoma: epidemiologic aspects. Ophthalmol Clin North Am. 2005;18:75-84, viii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 189] [Cited by in F6Publishing: 197] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 2. | Shields JA, Shields CL. Management of posterior uveal melanoma: past, present, and future: the 2014 Charles L. Schepens lecture. Ophthalmology. 2015;122:414-428. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 3. | Macdonald EC, Cauchi P, Kemp EG. Proton beam therapy for the treatment of uveal melanoma in Scotland. Br J Ophthalmol. 2011;95:1691-1695. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Damato B, Kacperek A, Errington D, Heimann H. Proton beam radiotherapy of uveal melanoma. Saudi J Ophthalmol. 2013;27:151-157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Rivard MJ, Melhus CS, Sioshansi S, Morr J. The impact of prescription depth, dose rate, plaque size, and source loading on the central axis using 103Pd, 125I, and 131Cs. Brachytherapy. 2008;7:327-335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Reichstein D, Karan K. Plaque brachytherapy for posterior uveal melanoma in 2018: improved techniques and expanded indications. Curr Opin Ophthalmol. 2018;29:191-198. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Tsujii H, Kamada T, Shirai T, Noda K, Tsuji H, Karasawa K. Carbon-Ion Radiotherapy: Principles, Practices, and Treatment Planning. Springer Japan, 2014: 163-168. [DOI] [Cited in This Article: ] |
| 8. | Takahashi W, Nakajima M, Yamamoto N, Yamashita H, Nakagawa K, Miyamoto T, Tsuji H, Kamada T, Fujisawa T. A prospective nonrandomized phase I/II study of carbon ion radiotherapy in a favorable subset of locally advanced non-small cell lung cancer (NSCLC). Cancer. 2015;121:1321-1327. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Hayashi K, Yamamoto N, Nakajima M, Nomoto A, Tsuji H, Ogawa K, Kamada T. Clinical outcomes of carbon-ion radiotherapy for locally advanced non-small-cell lung cancer. Cancer Sci. 2019;110:734-741. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Karube M, Yamamoto N, Shioyama Y, Saito J, Matsunobu A, Okimoto T, Ohno T, Tsuji H, Nakano T, Kamada T. Carbon-ion radiotherapy for patients with advanced stage non-small-cell lung cancer at multicenters. J Radiat Res. 2017;58:761-764. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE guidelines: consensus-based clinical case reporting guideline development. BMJ Case Rep. 2013;2013. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 234] [Cited by in F6Publishing: 243] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 12. | Koto M, Ikawa H, Kaneko T, Hagiwara Y, Hayashi K, Tsuji H. Long-term outcomes of skull base chordoma treated with high-dose carbon-ion radiotherapy. Head Neck. 2020;42:2607-2613. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Chattopadhyay C, Kim DW, Gombos DS, Oba J, Qin Y, Williams MD, Esmaeli B, Grimm EA, Wargo JA, Woodman SE, Patel SP. Uveal melanoma: From diagnosis to treatment and the science in between. Cancer. 2016;122:2299-2312. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 251] [Cited by in F6Publishing: 229] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 14. | Shukla S, Acharya S, Dulani M. Choroid Melanoma - A Rare Case Report. J Clin Diagn Res. 2015;9:ED09-ED10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Lucena E, Goldemberg DC, Thuler LCS, de Melo AC. Epidemiology of uveal melanoma in Brazil. Int J Retina Vitreous. 2020;6:51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Furdova A, Slezak P, Chorvath M, Waczulikova I, Sramka M, Kralik G. No differences in outcome between radical surgical treatment (enucleation) and stereotactic radiosurgery in patients with posterior uveal melanoma. Neoplasma. 2010;57:377-381. [PubMed] [Cited in This Article: ] |
| 17. | Thornton S, Coupland SE, Heimann H, Hussain R, Groenewald C, Kacperek A, Damato B, Taktak A, Eleuteri A, Kalirai H. Effects of plaque brachytherapy and proton beam radiotherapy on prognostic testing: a comparison of uveal melanoma genotyped by microsatellite analysis. Br J Ophthalmol. 2020;104:1462-1466. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Hirasawa N, Tsuji H, Ishikawa H, Koyama-Ito H, Kamada T, Mizoe JE, Ito Y, Naganawa S, Ohnishi Y, Tsujii H. Risk factors for neovascular glaucoma after carbon ion radiotherapy of choroidal melanoma using dose-volume histogram analysis. Int J Radiat Oncol Biol Phys. 2007;67:538-543. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Toyama S, Tsuji H, Mizoguchi N, Nomiya T, Kamada T, Tokumaru S, Mizota A, Ohnishi Y, Tsujii H; Working Group for Ophthalmologic Tumors. Long-term results of carbon ion radiation therapy for locally advanced or unfavorably located choroidal melanoma: usefulness of CT-based 2-port orthogonal therapy for reducing the incidence of neovascular glaucoma. Int J Radiat Oncol Biol Phys. 2013;86:270-276. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69-90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23762] [Cited by in F6Publishing: 25175] [Article Influence: 1936.5] [Reference Citation Analysis (3)] |
| 21. | Fernández-Ruiz M, Guerra-Vales JM, Castelbón-Fernández FJ, Llenas-García J, Caurcel-Díaz L, Colina-Ruizdelgado F. Multiple primary malignancies in Spanish patients with hepatocellular carcinoma: analysis of a hospital-based tumor registry. J Gastroenterol Hepatol. 2009;24:1424-1430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |