Published online May 6, 2021. doi: 10.12998/wjcc.v9.i13.3114
Peer-review started: November 15, 2020
First decision: January 27, 2021
Revised: February 8, 2021
Accepted: March 3, 2021
Article in press: March 3, 2021
Published online: May 6, 2021
Bezoars are conglomerates of indigestible foreign material that can be found in the gastrointestinal tract. Gastric ulcer, gastrointestinal perforation, and intestinal obstruction are the main complications. Acute pancreatitis secondary to bezoar is rare. Here, we present a rare case of a migratory gastric bezoar complicated by acute pancreatitis and small bowel obstruction after dissolution therapy.
A-65-year-old woman underwent gastroscopy because of epigastric pain, which revealed a huge bezoar and a gastric ulcer 10 d prior. The patient was discharged with a prescription of drinking 1 L Coca-Cola daily for 6 d, without repeat gastroscopy. However, she suddenly developed epigastric pain, nausea and vomiting for 3 d. Abdominal computed tomography (CT) revealed mild inflammation of the pancreas. Magnetic resonance cholangiopancreatography showed no abnormalities in the pancreatic duct or common bile duct. The nasogastric tube still showed drainage of more than 1.6 L of dark fluid each day after symptomatic treatment. Abdominal CT re-examination suggested intestinal obstruction. Esophagogastroduodenoscopy revealed a huge yellowish hard mass in the jejunal lumen, and we used the basket and net to fragment the bezoar. She was discharged with a good outcome.
Endoscopic therapy is the first choice for gastric bezoars. When mechanical disintegration cannot be achieved, timing of repeat endoscopy is important during Coca-Cola dissolution therapy.
Core Tip: Coca-Cola dissolution therapy is as an easy, safe, and cost-effective option for gastric bezoars. Acute pancreatitis and small intestinal obstruction secondary to a migratory gastric bezoar during Coca-Cola dissolution therapy has not been previously reported. Here, we report a case of acute pancreatitis and small bowel obstruction caused by a migratory gastric bezoar after dissolution therapy.
- Citation: Wang TT, He JJ, Liu J, Chen WW, Chen CW. Acute pancreatitis and small bowel obstruction caused by a migratory gastric bezoar after dissolution therapy: A case report. World J Clin Cases 2021; 9(13): 3114-3119
- URL: https://www.wjgnet.com/2307-8960/full/v9/i13/3114.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i13.3114
Bezoars are accumulations of indigestible foreign material that can be found in the gastrointestinal tract[1]. They usually occur in patients with reduced gastric motor and delayed gastric emptying[2]. The clinical manifestations of gastric bezoars are mainly nonspecific such as dyspepsia, anorexia, epigastric pain, nausea and vomiting[3]. Major complications include gastric ulcer, gastrointestinal perforation, and intestinal obstruction[4]. Coca-Cola dissolution therapy of gastric bezoars is an easy, safe, and cost-effective option[5]. However, acute pancreatitis and small intestinal obstruction caused by a migratory gastric bezoar during Coca-Cola dissolution therapy has not been previously reported.
Here, we report a case of acute pancreatitis and small bowel obstruction caused by a migratory gastric bezoar after dissolution therapy.
A 65-year-old woman was admitted to our department with epigastric pain, nausea, and vomiting for 3 d.
The patient underwent gastroscopy because of epigastric pain, which showed a huge bezoar and a gastric ulcer 10 d prior (Figure 1). The bezoar could not be removed by endoscopy due to its large size and hardness. The patient was discharged with a prescription of drinking 1 L Coca-Cola daily for the following 6 d. However, she did not accept re-examination by gastroscopy to observe the efficacy of dissolution therapy. Subsequently, the patient was admitted to our department with epigastric pain, nausea, and vomiting for 3 d. Follow-up medical history showed that she had been ingesting persimmons frequently in the recent 2 mo.
No significant medical history was recorded such as previous gastric surgery, hyperlipidemia, or alcohol consumption.
The patient had no previous or family history of similar illnesses.
The clinical abdominal examination revealed epigastric tenderness and distension without rebound tenderness. All other vital signs were stable.
Abnormally elevated laboratory findings at admission included a leukocyte count of 14830/mm3, aspartate transaminase 60 IU/L, alanine transaminase 64 IU/L, -glutamyl transpeptidase 418 IU/L, and alkaline phosphatase 167 IU/L. Serum amylase and lipase were > 3 times higher than the upper limit of normal, at 507 IU/L and 745 IU/L, respectively.
Abdominal computed tomography (CT) revealed mild inflammation of the pancreas (Figure 2). Subsequent magnetic resonance cholangiopancreatography (MRCP) showed no abnormalities in the pancreatic duct or common bile duct.
After symptomatic treatment, including gastrointestinal decompression, fluid resuscitation and antibiotic therapy, the abdominal pain was relieved. The levels of serum transaminase, amylase and lipase were gradually reduced. However, the nasogastric tube showed drainage of > 1.6 L of dark fluid each day after admission. Abdominal CT re-examination demonstrated gastric distension and loops of small intestine with multiple gas-fluid levels, which suggested intestinal obstruction (Figure 3).
The final diagnosis was acute pancreatitis and small bowel obstruction.
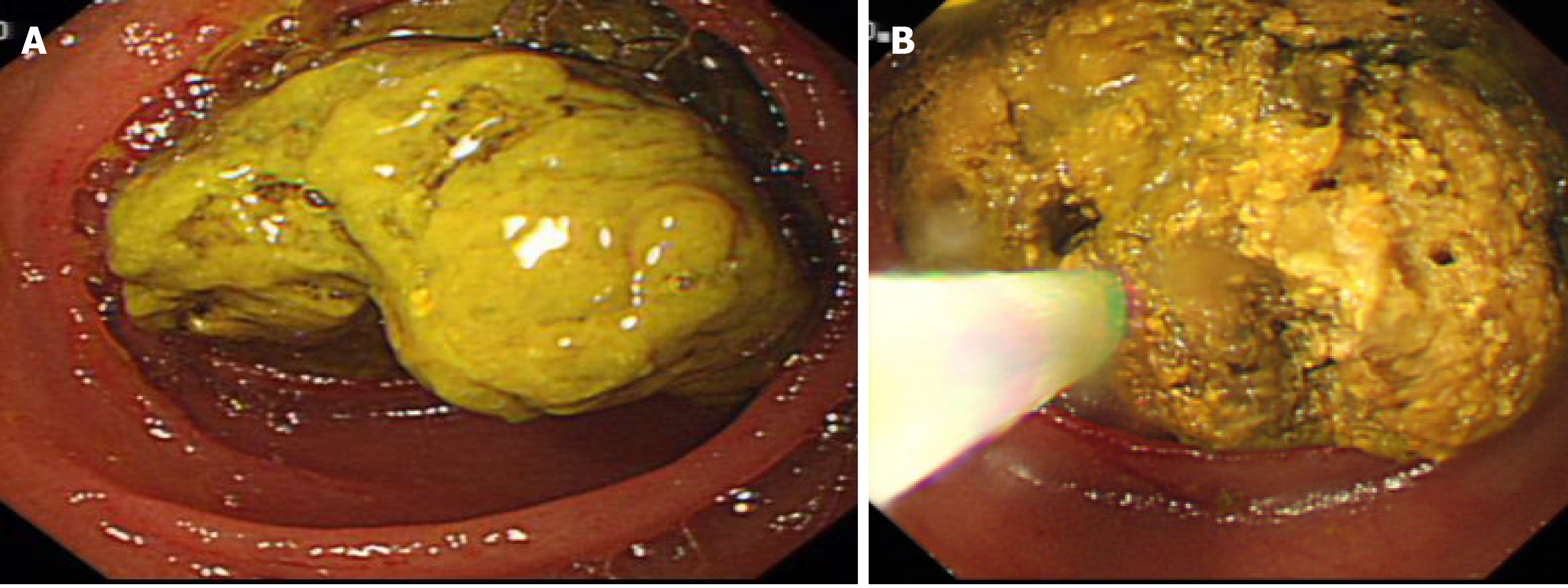
Esophagogastroduodenoscopy was performed, and a large yellowish hard mass was found in the jejunal lumen, which was suspected to have migrated from the stomach (Figure 4A). We fragmented the bezoar with the basket and net so that the endoscope could pass through the obstructed lumen (Figure 4B).
The patient was discharged in good condition after 3 d. There has been no evidence of recurrence of acute pancreatitis for 3 years during follow-up.
Bezoars can be classified into four main types depending on their component sources: phytobezoars, trichobezoars, pharmacobezoars and lactobezoars[6]. Phytobezoars are the most common type, and are composed of indigestible vegetables or fruits or other food material[7]. The predisposing factors include prior gastric surgery, excessive consumption of foods with high fiber and tannins, diabetes mellitus, mental retardation, peptic ulcer, hypothyroidism, and poor mastication[8]. The clinical symptoms of bezoars are mainly nonspecific, and some patients may be asymptomatic or present with gastrointestinal symptoms, such as epigastric pain, dyspepsia, anorexia, nausea and vomiting, which depends on the location and size of the bezoars[3,4]. Gastric ulcer, accounting for approximately 52%, is the main complication, followed by gastrointestinal perforation and intestinal obstruction[4,9]. In addition, obstruction caused by bezoars mostly occurs at the distal end of the ileum and ileocecal valve with overall rates of 0.4%-4%[10]. This may be due to migration of the gastric bezoar, and the major symptoms include abdominal pain, nausea and vomiting[11].
For our patient, no abnormalities were found in the pancreatic duct or common bile duct on abdominal CT and MRCP. However, acute pancreatitis secondary to phytobezoar has seldom been reported so far. The mechanism of acute pancreatitis in our patient may have been as follows. The migratory bezoar may have obstructed the ampulla of Vater, causing spasm and congestion of the sphincter of Oddi, which led to the occurrence of acute pancreatitis. Second, bezoar-induced small intestinal obstruction may have caused gradually increased pressure in the small bowel. The regurgitation of bile may have abnormally activated trypsin once the pressure of the intestine was higher than that of the pancreatic duct, thus inducing acute pancreatitis. Most gastric phytobezoars can be successfully treated with oral intake of Coca-Cola, through dissolving or diminishing the size or softening the bezoars. Ladas et al[5] reviewed 46 patients from 24 papers and found that 91% of patients were successfully treated with Coca-Cola, either alone or conjunction with endoscopic extraction[5]. The mechanism of Coca-Cola dissolution is not thoroughly explained. Coca-Cola has an acidity of pH 2.6, which resembles gastric acid, and may be important in digesting fiber. In addition, sodium bicarbonate mucolytic effect and the penetration of carbon dioxide (CO2) bubbles are also the important factors in the dissolving mechanism[12]. However, the CO2 bubbles could increase the pressure in the stomach temporarily, which may help to push the shrunken bezoar through the pylorus and further lead to gastric outlet obstruction or small intestinal obstruction[13]. Diospyrobezoar is a type of phytobezoar caused by persimmons, which is considered more difficult to dissolve completely by only drinking Coca-Cola compared with other types of phytobezoars because of their hard consistency[12]. In our case, migration of the diospyrobezoar resulted in small intestinal obstruction and acute pancreatitis during oral administration of Coca-Cola. The treatment of gastric bezoars includes chemical dissolution, endoscopic fragmentation and extraction, and surgery[2]. Moreover, endoscopic procedures are the preferred treatment for gastric bezoars, through using snares, baskets, biopsy forceps, microwave or laser devices, depending on the location, size and texture of the bezoars[2,6]. It is difficult to achieve mechanical disintegration when the bezoars are large or hard. Dissolution therapy should be performed first to diminish the size and soften the bezoars, followed by adjuvant endoscopic treatment. Additionally, emergency treatment such as endoscopy or surgery is needed to handle complicated small bowel obstruction[14]. In the present case, the patient was discharged with a prescription of drinking Coca-Cola daily because the bezoar was too large to be removed directly under endoscopy. Unfortunately, the migratory bezoar resulted in acute pancreatitis and small bowel obstruction after partial dissolution with Coca-Cola.
We report a case of acute pancreatitis and small bowel obstruction caused by a migratory gastric bezoar, highlighting that endoscopic treatment should be the first choice for gastric bezoars, and that timing of repeat endoscopy is crucial during Coca-Cola dissolution therapy for patients who cannot achieve mechanical disintegration.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kozarek R S-Editor: Fan JR L-Editor: Filipodia P-Editor: Xing YX
| 1. | Altintoprak F, Gemici E, Yildiz YA, Yener Uzunoglu M, Kivilcim T. Intestinal Obstruction due to Bezoar in Elderly Patients: Risk Factors and Treatment Results. Emerg Med Int. 2019;2019:3647356. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Paschos KA, Chatzigeorgiadis A. Pathophysiological and clinical aspects of the diagnosis and treatment of bezoars. Ann Gastroenterol. 2019;32:224-232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Gök AFK, Sönmez RE, Kantarcı TR, Bayraktar A, Emiroğlu S, İlhan M, Güloğlu R. Discussing treatment strategies for acute mechanical intestinal obstruction caused by phytobezoar: A single-center retrospective study. Ulus Travma Acil Cerrahi Derg. 2019;25:503-509. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Kim JH, Chang JH, Nam SM, Lee MJ, Maeng IH, Park JY, Im YS, Kim TH, Park IY, Han SW. Duodenal obstruction following acute pancreatitis caused by a large duodenal diverticular bezoar. World J Gastroenterol. 2012;18:5485-5488. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 15] [Cited by in F6Publishing: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Ladas SD, Kamberoglou D, Karamanolis G, Vlachogiannakos J, Zouboulis-Vafiadis I. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther. 2013;37:169-173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 107] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 6. | Ugenti I, Travaglio E, Lagouvardou E, Caputi Iambrenghi O, Martines G. Successful endoscopic treatment of gastric phytobezoar: A case report. Int J Surg Case Rep. 2017;37:45-47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Zwicky S, Inauen W, Pfefferkorn U. Case Report: Phytobezoar Causing Gastric Outlet Obstruction as a Late Complication After Biliopancreatic Diversion with Duodenal Switch. Obes Surg. 2020;30:3233-3235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Gökbulut V, Kaplan M, Kaçar S, Akdoğan Kayhan M, Coşkun O, Kayaçetin E. Bezoar in upper gastrointestinal endoscopy: A single center experience. Turk J Gastroenterol. 2020;31:85-90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Iwamuro M, Tanaka S, Shiode J, Imagawa A, Mizuno M, Fujiki S, Toyokawa T, Okamoto Y, Murata T, Kawai Y, Tanioka D, Okada H, Yamamoto K. Clinical characteristics and treatment outcomes of nineteen Japanese patients with gastrointestinal bezoars. Intern Med. 2014;53:1099-1105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Mohseni M, Kruse B. An Unusual Mimic of Intermittent Bowel Obstruction. Am J Case Rep. 2019;20:1920-1922. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Wang PY, Wang X, Zhang L, Li HF, Chen L, Wang B. Bezoar-induced small bowel obstruction: Clinical characteristics and diagnostic value of multi-slice spiral computed tomography. World J Gastroenterol. 2015;21:9774-9784. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 30] [Cited by in F6Publishing: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Ha SS, Lee HS, Jung MK, Jeon SW, Cho CM, Kim SK, Choi YH. Acute intestinal obstruction caused by a persimmon phytobezoar after dissolution therapy with Coca-Cola. Korean J Intern Med. 2007;22:300-303. [PubMed] [Cited in This Article: ] |
| 13. | Lu L, Zhang XF. Gastric Outlet Obstruction--An Unexpected Complication during Coca-Cola Therapy for a Gastric Bezoar: A Case Report and Literature Review. Intern Med. 2016;55:1085-1089. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 14. | Nasri B, Calin M, Shah A, Gilchrist B. A rare cause of small bowel obstruction due to bezoar in a virgin abdomen. Int J Surg Case Rep. 2016;19:144-146. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |