Published online Dec 6, 2020. doi: 10.12998/wjcc.v8.i23.5988
Peer-review started: August 30, 2020
First decision: September 13, 2020
Revised: September 15, 2020
Accepted: September 25, 2020
Article in press: September 25, 2020
Published online: December 6, 2020
Since 2017, the number of magnet ingestion cases has increased year over year in our hospital. Almost all of the ingested magnetic foreign bodies were magnetic beads, and most of the patients experienced intestinal perforations, causing substantial damage.
To summarize our experience with surgical treatment of multiple magnet ingestion in children.
The data for general surgeries were collected from January 2010 to April 2020, and the clinical characteristics, treatment methods, and outcomes were summarized and analyzed. Several typical cases were selected and discussed.
Fifty-six cases of ingested magnetic foreign bodies were collected, of which 47 were magnetic beads. The average patient age was 4.7 ± 3.0 years old. The number of ingested magnetic foreign bodies ranged from 2 to 73. There were 26 cases with symptoms at the time of admission, including two cases of shock. Thirteen patients were discharged successfully following conservative treatment and 43 were treated by surgery. Laparotomy was the main method of operation. Laparoscopy was used in four cases, of which three were converted to open surgery, and one was treated successfully using surgery through the navel. Postoperative complications occurred in seven cases, incision infections were observed in six, and adhesive ileus was observed in one.
Clinicians need to summarize their experiences with treating magnetic foreign body ingestions in detail and carry out clinical research to reduce the damage to children.
Core Tip: Since 2017, the numbers of magnet ingestion has increased year over year in our hospital and most of the patients experienced intestinal perforations. We found several significant clinical features: Intestinal contents did not leak into the abdominal cavity, and gastrointestinal symptoms were caused by ileus rather than perforation, which were obviously different from intestinal perforation caused by other reasons. This means that the traditional treatment strategy cannot be used simply to deal with intestinal perforation caused by magnetic beads, and a more favorable treatment scheme should be selected according to its clinicopathological characteristics.
- Citation: Cai DT, Shu Q, Zhang SH, Liu J, Gao ZG. Surgical treatment of multiple magnet ingestion in children: A single-center study. World J Clin Cases 2020; 8(23): 5988-5998
- URL: https://www.wjgnet.com/2307-8960/full/v8/i23/5988.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i23.5988
Foreign body ingestion is a common pediatric emergency[1], and the management of which includes allowing the foreign body to be discharged by itself, emergency endoscopy, and surgical intervention[2]. The number of surgical operations accounts for 1% of the total cases[3]. Magnetic foreign bodies, button batteries, and expansion toys are the main types of foreign bodies that require surgical treatment. Since 2017, the number of magnet ingestion cases has increased year over year in our hospital. Almost all of the ingested magnetic foreign bodies were magnetic beads, and most of the patients experienced intestinal perforations, causing substantial damage. We summarized our surgical experience, with the hope of providing help for optimizing the diagnosis and treatment.
The clinical data for multiple magnet ingestions at the General Surgery Department of our Children’s Hospital in China were collected from January 2010 to April 2020. The clinical characteristics, treatment methods, outcomes, and prognoses were described and analyzed. Several typical cases were focused on and discussed.
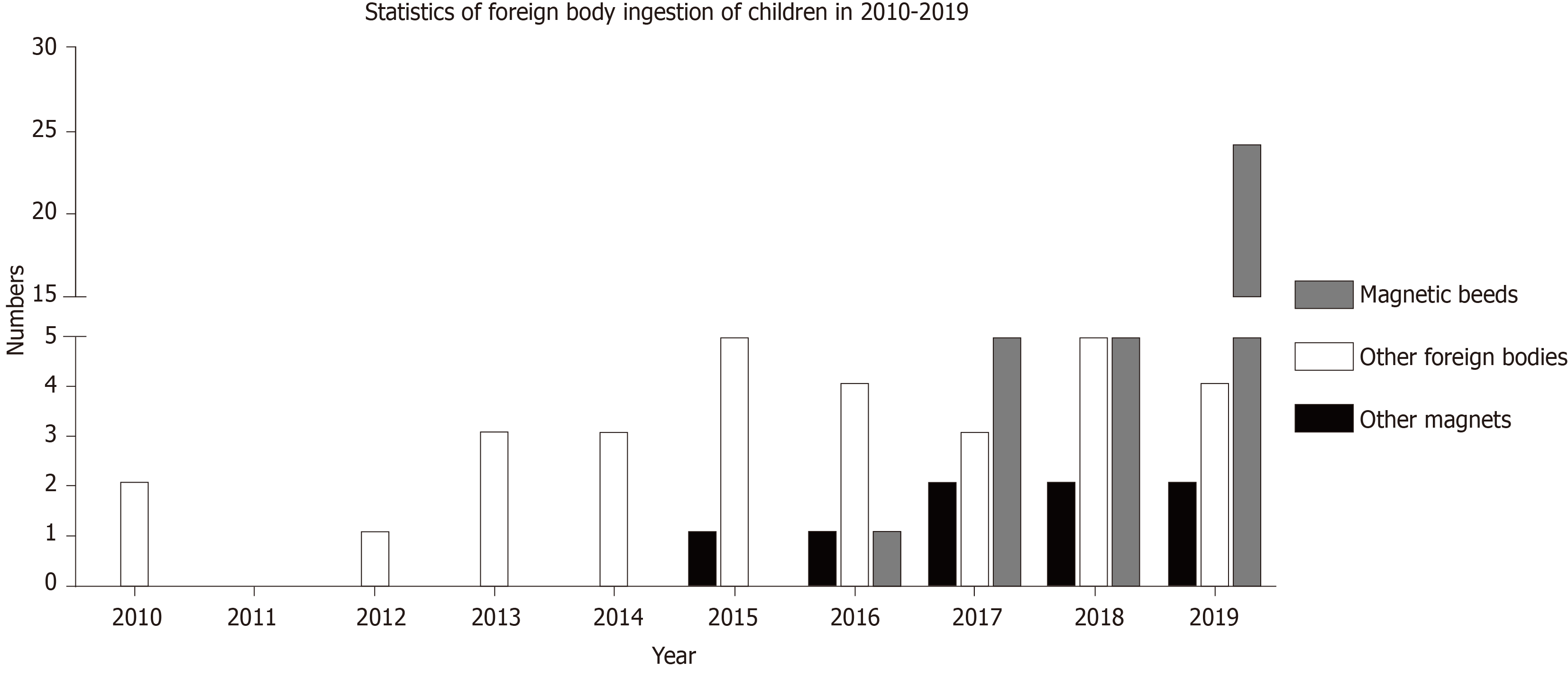
From January 2010 to April 2020, 85 patients with foreign bodies in their digestive tract were admitted to our General Surgery Department, including 56 cases with magnetic foreign bodies. Of those 56 cases, 47 were magnetic beads (Figure 1). The ratio of male to female patients was 4:1, the average age was 4.7 ± 3.0 years, and the number of swallowed magnetic foreign bodies ranged from 2 to 73. There were 45 cases whose time of swallowing could be confirmed by the parents or children, and ranged from 2 h to 18 d before admission. There were only six cases with abdominal pain (crying); 15 with abdominal pain (crying) and vomiting; three with abdominal pain (crying), vomiting, and fever; two with shock; and 30 without symptoms at the time of admission (Table 1). Twenty-six cases received emergency gastroscopy before admission, of which two cases with intestinal magnetic residues received surgical observation after a portion of the foreign magnetic bodies in the stomach were removed. One patient lacking magnetic residues received surgical observation after the magnetic beads located in the esophageal fundus were removed by gastroscopy. In 23 cases, no foreign bodies were observed in the stomach. After admission, there were two cases where all of the magnets in the stomach were removed by gastroscopy, and without surgery. In eight cases, all foreign bodies were discharged by themselves without surgery, including six cases of magnetic beads, one case of a disk magnet, and one case of a strip magnet (Table 2). In two cases, surgical observation discharged the intestinal magnetic residues after admission. Another patient with suspected esophageal gastric junction injury was discharged 1 wk after observation. The remaining 43 cases were removed by surgery, and accounted for 76.8% of the total number of magnetic foreign bodies. All patients were examined using a standing abdominal radiograph. Positive foreign bodies were observed as a shadow, and no cases of gas accumulation in the subphrenic space were observed.
| n = 56 | Proportion (Intragroup proportion)1 | |
| The time of ingestion can be confirmed | 45 | 80.4% |
| < 3 d | (33) | (73.3%) |
| 3-14 d | (7) | (15.6) |
| > 14 d | (5) | (11.1) |
| Unable to determine the time of ingestion | 11 | 19.6% |
| Having gastrointestinal symptoms | (9) | (81.8%) |
| Having no gastrointestinal symptoms | (2) | (18.2%) |
| Admission symptoms | ||
| Abdominal pain (crying) | 6 | 10.7% |
| Abdominal pain (crying) and vomiting | 15 | 26.8% |
| Abdominal pain (crying), vomiting, and fever | 3 | 5.4% |
| Shock | 2 | 3.6% |
| No symptoms | 30 | 53.6% |
| Cases without gastroscope, without surgery, whose all magnetic foreign bodies were discharged by themselves | ||||
| No. | Age (yr) | DBIG (day) | NIM | Type of magnet |
| 1 | 4 | 3, 61 | 2 | Disk magnet |
| 2 | 5 | 3 | 3 | Magnetic bead |
| 3 | 5 | 5 | 4 | Magnetic bead |
| 4 | 6 | 2 | 4 | Magnetic bead |
| 5 | 7 | 2 | 2 | Magnetic bead |
| 6 | 8 | 1 | 7 | Magnetic bead |
| 7 | 8 | 3 | 2 | Strip magnet |
| 8 | 10 | 2 | 2 | Magnetic bead |
| Cases of intestinal magnetic residue after gastroscopy, which were discharged by themselves | ||||
| No. | Age (yr) | DBIG (d) DBGD (d) | NIM/NIMR | Type of magnet |
| 1 | 10 | 2/1 | 3/1 | Magnetic bead |
| 2 | 13 | 5/4 | 4/2 | Magnetic bead |
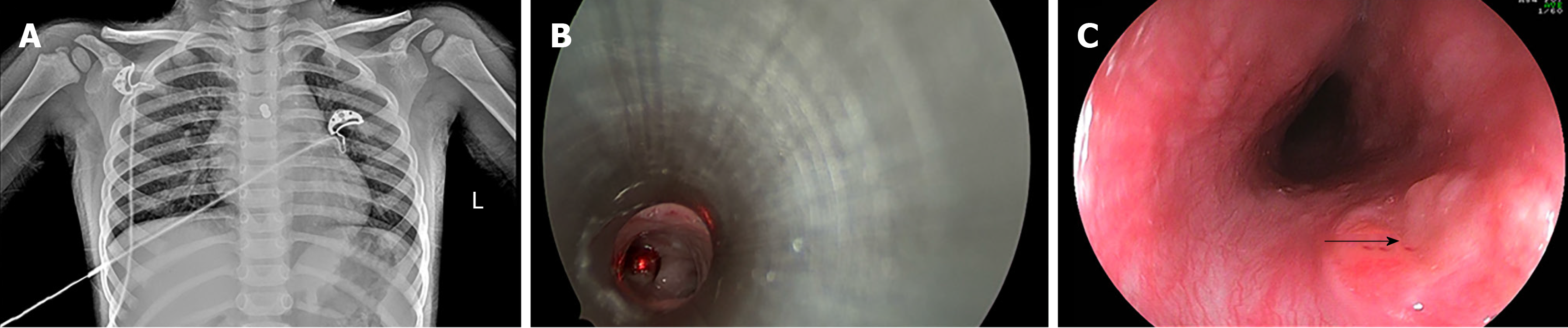
Among 43 children who underwent surgery, 36 experienced perforation of the digestive tract. Those children accounted for 83.7% of the surgical cases, and 64.3% of the total number of magnetic foreign bodies. Cases with two perforations in the digestive tract were the most prevalent, accounting for 61% of all perforation cases. The small intestine was the most frequent site for magnet adsorption (Table 3). There were 16 cases of intestinal obstruction, two cases of peritonitis, one case of intestinal necrosis caused by strangulation, 13 cases of internal fistulas, one case of esophagotracheal fistulas (Figure 2), and one case of intestinal magnetic perforation with Ascaris lumbricoides. The main surgical approach was perforation repair, while five cases received intestinal resection. A child with an esophagotracheal fistula was treated with a gastrojejunal tube and recovered after conservative treatment for 3 mo.
| Position | n = 36 | Proportion (%) |
| Small intestine-small intestine | 15 | 41.7 |
| Stomach-small intestine | 8 | 22.2 |
| Small intestine-colon | 4 | 11.1 |
| Duodenum-small intestine | 3 | 8.3 |
| Stomach-colon | 2 | 5.6 |
| Duodenum-colon | 2 | 5.6 |
| Stomach-small intestine - colon | 1 | 2.8 |
| Esophagus-trachea1 | 1 | 2.8 |
| Esophagus-stomach | 1 | 2.8% |
During surgery, it was found that magnets did not cause perforation in seven cases. In six cases, the magnetic beads were adsorbed in the same intestinal tract, where in one case, 13 magnetic beads were observed. In another case, the magnetic beads were located in two intestinal segments that were far away from each other. Thirty-nine cases underwent laparotomy and four cases underwent laparoscopy. The treatments of three of the laparoscopy cases were converted to laparotomy for the following reasons: (1) The magnetic beads were adsorbed on the back wall of the stomach and no foreign bodies were found via laparoscopy; (2) 13 magnetic beads were combined, but no intestinal perforations were observed by laparoscopy; and (3) The magnetic beads were adsorbed into the front wall of the stomach to the jejunum, and could not be removed through the umbilicus. One patient with small intestine perforation received laparoscopic surgery as his intestines could be dragged out through the umbilicus. The average length of hospital stay was 10.8 ± 3.2 d. Postoperative complications were observed in seven cases, incision infections were observed in six, and adhesive postoperative intestinal obstruction was observed in one.
Foreign bodies in the digestive tract are common in children, and 80%-90% of foreign bodies can be discharged by themselves with no medical intervention required[4]. In the clinical management of foreign body ingestion, conservative treatment is the main approach, while 10%–20% of cases require endoscopic intervention[4]. In the General Surgery Department of our hospital from 2010 to 2014, there were less than five foreign body ingestion cases admitted every year, and those cases that did present to our department primarily included needle shaped foreign bodies, followed by button batteries. In 2015, the first case of a disk magnet ingestion was admitted to the hospital, while the first treatment of a child that swallowed magnetic beads was in 2016. In the following years, the number of cases involving swallowing magnetic beads increased rapidly. In 2019, the number of cases of swallowed magnetic beads accounted for 80% of all foreign body ingestion cases at our hospital. Thus, such a prevalence require us to increase our vigilance.
We found that all of the ingested magnetic beads were toys called buckyballs that are made of neodymium magnets, and are at least 5 to 10 times more powerful than traditional magnets[5]. Buckyballs were originally designed as a type of adult decompression toy, but an increasing number of reports of swallowed rare earth neodymium magnets were observed in the late 2000s in the United States[5-7]. In 2007, the United States Consumer Product Safety Commission (CPSC) issued the first health warning concerning the products and in 2009, issued a ban on the sale of rare earth magnets to children younger than 14 years of age[8].
Unfortunately, after 2010, buckyballs were introduced by businessmen in China as an educational toy, and gradually became popular among children. However, the CPSC ban was ignored, which led to an increase in intestinal damage caused by buckyballs. From 2017 to 2019, the number of children admitted to our department who swallowed buckyballs by mistake doubled every year. What is more worrisome is that according to our statistics, the average age of ingestion of magnetic foreign bodies was 4.7 years old, which is not the age of school children who have more opportunities to contact such magnets. Rather, children who have elder brothers and sisters have become the victims of the disease. The youngest patient in our department was only 16 mo old, and the ingested buckyballs were his elder brother's toy, which led to intestine perforation. We are sure that the most effective way to reduce the increasingly high incidence of injury from magnetic foreign body ingestion is by banning the sale of powerful magnetic toys like buckyballs for minors, and making sure that children remain far away from the powerful magnetic toys in their living environments.
All cases of magnetic foreign body ingestion in our department, including 35 children with gastrointestinal perforation, exhibited no pneumoperitoneum on the preoperative abdominal standing film, and their intestinal contents were not found to enter the abdominal cavity. It can be speculated that even though the two sections of the intestinal tubes were perforated by the powerful magnetic foreign bodies, the intestinal wall around the perforation remained in a closed and tight state, and the intestinal contents did not leak from the perforation. When such a state is maintained for a long period of time, an internal fistula will form between the two intestines. This is also the theoretical basis for “magnetic press anastomotic technology” that has emerged in recent years[9].
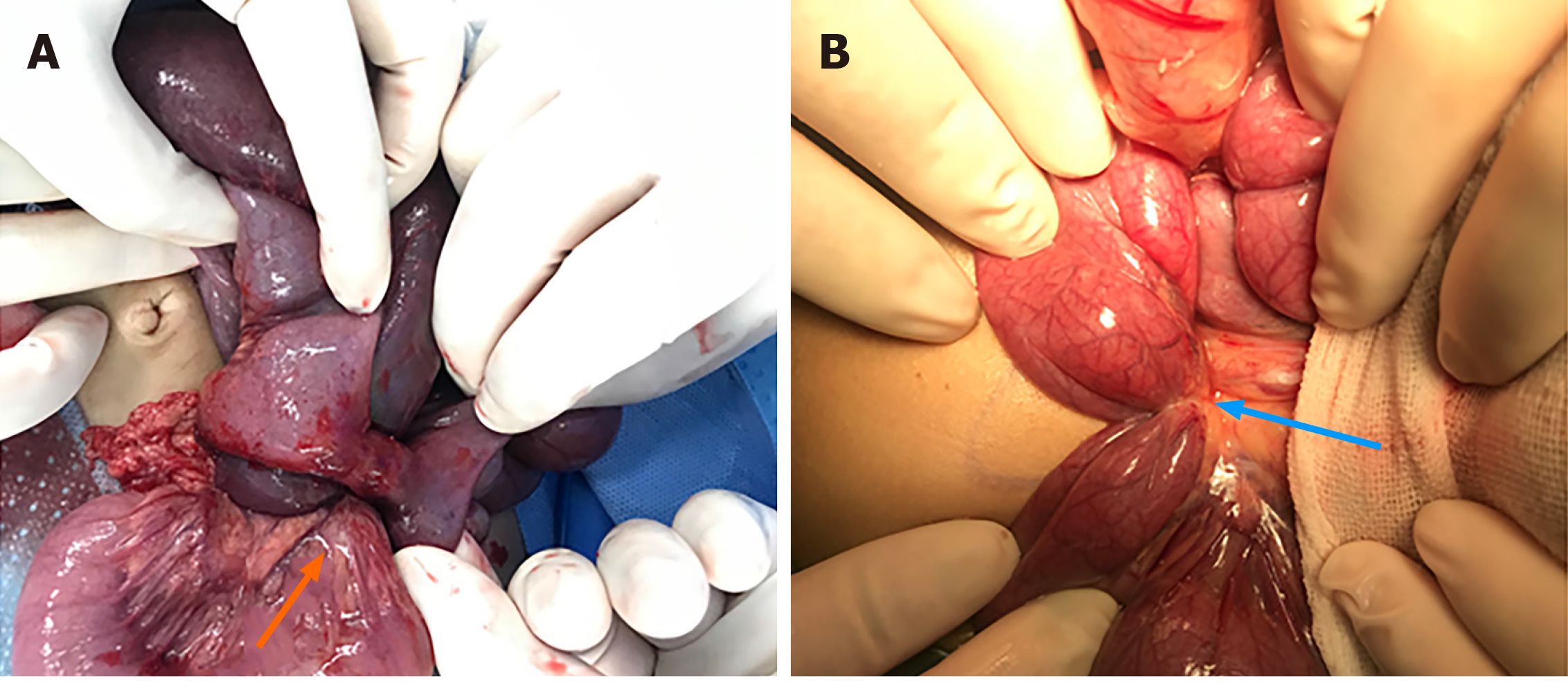
There were 30 children admitted to our department without symptoms, which accounted for 53.6% of the total patients with magnet ingestions. The other 26 patients with symptoms underwent surgery, all of whom experienced intestinal perforation. It was found during surgery that the gastrointestinal symptoms were not caused by perforation, but by mechanical intestinal obstruction due to the formation of closed loops or compression of the proximal intestinal tract. The severity of symptoms was related directly to the severity of intestinal obstruction. The related gastrointestinal symptoms were mainly abdominal pain, accompanied with vomiting, fever, and even shock (in two cases). The time since ingestion of magnets to presentation in our department was more than 2 wk in both cases with shock. Those asymptomatic patients presented to our hospital after experiencing sudden shock. It was found during operation that one case exhibited a long fistula, which compressed the proximal small intestine and caused ischemia and necrosis. Another case experienced strap formation due to inflammatory tissue hyperplasia near the fistula, which compressed the proximal small intestine to form a mechanical obstruction (Figure 3). The ascites in both cases were purulent, but the compressed intestine had not yet been perforated. Thus, it is suggested that once a clinical diagnosis that magnetic foreign bodies are located in the digestive tract is made and there are gastrointestinal symptoms, emergency surgical exploration should be performed as rapidly as possible. The more serious the symptoms of obstruction, the higher the priority of surgery.
We considered whether we could take a long-term conservative treatment approach for asymptomatic children with a small number of ingested magnets. Until the formation of an internal fistula, the magnetic foreign bodies can discharge by themselves. However, this consideration was rejected after receiving the abovementioned two children who experienced shock. Thus, we suggest that even if patients defecate the magnetic foreign body after the formation of an internal fistula, there is still a high risk of intestinal ischemic necrosis caused by intestinal adhesion or internal fistula compression, which is similar to the internal hernias caused by a failure to close the mesenteric hiatus after intestinal anastomosis.
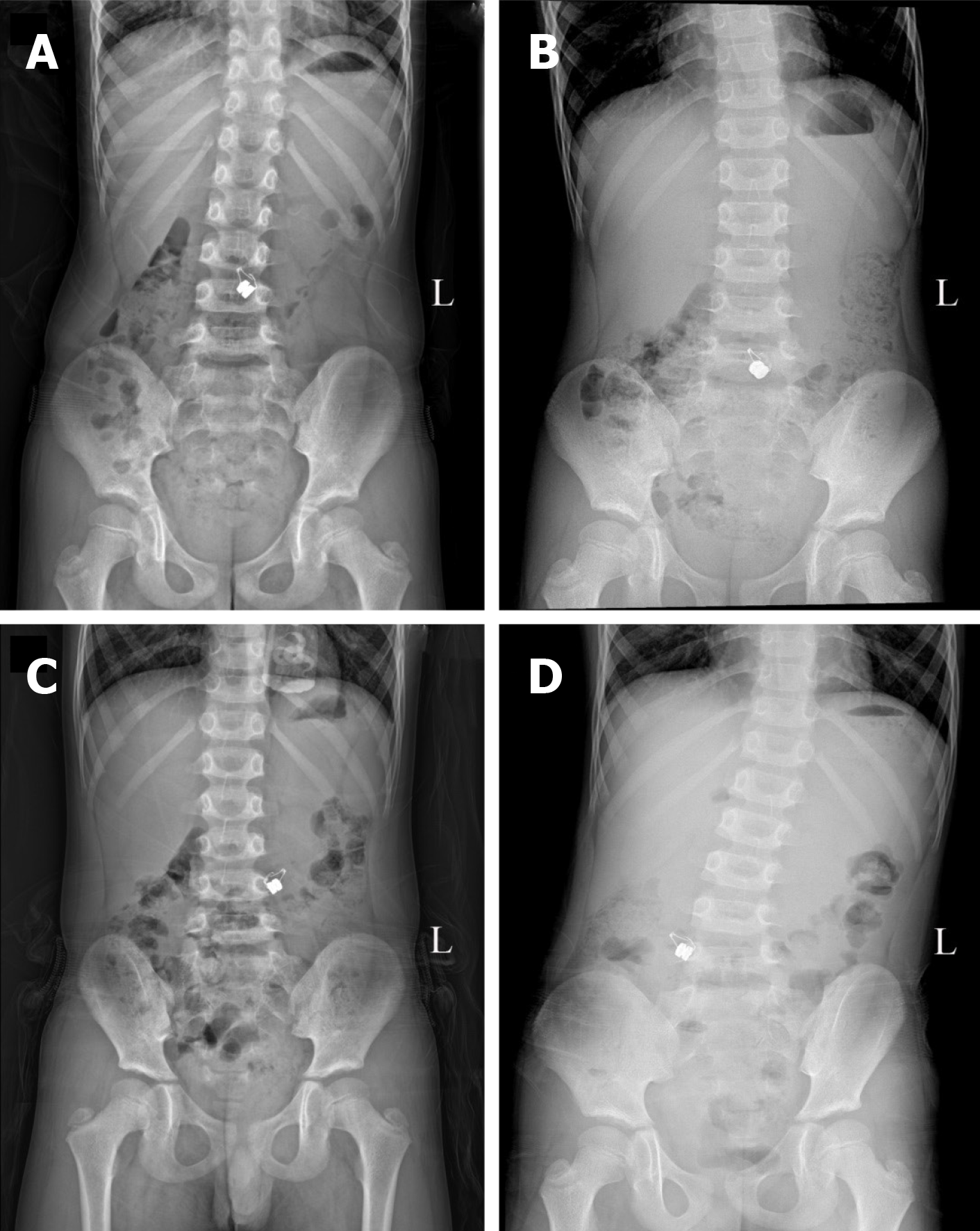
It is not guaranteed that magnetic foreign bodies will cause perforations when they enter the small intestine from the stomach. If several magnets are swallowed over a short time, or do not adsorb when they move in the intestine, they will not cause perforation. Magnets were discharged by themselves without operation in eight cases (Table 2), and one patient discharged the ingested magnets at different times after ingesting the magnets at different times (Figure 4). Combined with the five cases of intestinal magnetic bead ingestion where no perforation was observed during operation, 13 cases lacked perforation, and accounted for 25% of all intestinal magnetic foreign bodies. Thus, not all magnetic foreign bodies will cause intestinal perforation, even though they may have entered the small intestine from the stomach. Children may also discharge magnets without intervention. In addition, children swallowing magnetic foreign bodies at multiple different times may also discharge them at different times, without intestinal adsorption leading to perforation. Therefore, it is important to monitor abdominal radiographs every day.
For asymptomatic children with a changing position of the foreign body shadow, conservative observation can be performed. Table 2 shows that eight children discharged magnetic foreign bodies by themselves without surgery, with the times of discharge being concentrated around 2-3 d after swallowing. The longest time observed for magnetic bead discharge was 5 d in patient 3, while the longest time for disk magnet discharge was 6 d in patient 1. Two cases whose ingested magnetic beads in the stomach were removed before admission also discharged the residual intestinal magnetic beads after 1 d and 4 d.
In seven of ten cases, the positive foreign body shadow was located in the right lower abdomen in the final abdominal standing radiograph. The radiograph showed that the positive foreign body shadow was fixed in the right lower abdomen for 3 consecutive days in patient 1, while it was fixed in patient 3 for 2 consecutive days, suggesting that the ileocecal loop may have delayed entry of the foreign bodies into the colon. Our suggestion is as follows: For asymptomatic children whose magnetic foreign bodies enter the intestinal segment and whose abdominal standing radiograph indicates that the foreign body is still moving, conservative observation should be chosen during which most of the magnets will be discharged within 3 d. For asymptomatic children whose foreign bodies have moved previously, and then became fixed in the right lower abdomen, we suggest observing for another 3 d, as appropriate. Such patients also can consume lactulose and other catharsis agents to assist with defecation. Long-term adsorption of magnetic foreign bodies in the intestinal wall can form a strap or internal fistula, leading to acute intestinal obstruction. Thus, we suggest that if we miss the optimal conservative treatment time, surgical exploration should be considered.
The position of foreign bodies can be determined from abdominal standing radiographs, which can aid in the decision to perform gastroscopy and identify the position of the surgical incision. However, radiographs can also mislead the surgeon.
One child who swallowed two disk magnets was admitted to our department. Because the child failed to exhibit symptoms, he was initially given conservative treatment. We assessed abdominal standing radiographs for 4 consecutive days (Figure 5). The position of the foreign bodies was changing, primarily in the middle and lower abdomen. However, the magnet was not discharged by the fourth day, and thus, we performed surgery for which we made a transverse incision 2 cm below the umbilicus. Unexpectedly, no foreign bodies were found in any of the intestinal tubes. However, we could not explore the stomach due to the incision being too low. We then used intraoperative gastroscopy to investigate the location of the foreign bodies, and found two in the stomach. Following the operation, the course of the disease was traced back and it was found that the patient's abdominal standing radiographs were always assessed following eating. Thus, the expansion of the stomach and gravity caused the foreign bodies located in the great curvature of the stomach to be displayed in the middle and lower abdomen in the abdominal standing radiograph, thus interfering with the clinical assessment, which caused unnecessary damage to the child. Therefore, we suggest that foreign bodies be photographed on an empty stomach. If the foreign body shadow in the radiograph is above the L5 centrum and there are no digestive tract symptoms, gastroscopy should be initially considered. The selection of incision matters. Changes in body position and intestinal peristalsis may cause the foreign body to relocate. Thus, the C-arm machine should be used to locate the foreign body and determine the location of the incision before disinfecting after anesthesia to avoid difficulties associated with intraoperative exposure, unnecessary extension of the incision, or even a second incision. In addition, for children with an unknown number of foreign bodies prior to surgery, or suspected magnet displacement during operation, the abdominal plain radiograph should be reevaluated with the C-arm machine after the foreign bodies are removed. Such a process will ensure that no residual magnetic foreign bodies are present.
Except for two cases of gastrointestinal magnetic foreign bodies with intestinal strangulation and intestinal necrosis leading to peritonitis, there was no celiac pollution. Conversely, when the magnet was removed, it caused the intestinal contents to overflow into the abdominal cavity. Therefore, the goal of surgery is to remove the foreign body and repair the digestive tract damage without polluting the abdominal cavity.
There are two methods of surgical exploration of foreign magnetic bodies: Laparotomy and laparoscopy. The former is more commonly used and is applicable to all gastrointestinal foreign bodies, especially when the patient is in critical condition or has obvious abdominal distention. The latter is used to remove the intestinal tube through the navel after foreign bodies are detected by laparoscopy, and then complete the operation outside the abdomen. In our department, laparoscopy was used in four cases, of which three were converted to laparotomy, while one case succeeded. Table 3 shows that the most common position of adsorption was between the small intestines (41.7% of all cases), and the other positions accounted for 58.3% of cases. Magnets that were partially located in the stomach, duodenum, or colon were not easy to remove through the navel. If magnets were forcibly removed from the intestine by laparoscopy, celiac pollution, intestinal injury, residual magnet beads, tiny perforations, and mesenteric perforations may have been overlooked. Laparoscopic exploration is most suitable for children with the following: (1) Ingestion occurred more than 2 wk prior to admission; (2) No gastrointestinal symptoms are present; and (3) Only the small intestines were adsorbed by foreign bodies. Pulling the intestinal tube through the umbilicus at the location of the foreign body will not cause magnet separation and displacement, and the intestinal contents will not spill into the abdominal cavity because an internal fistula has been formed.
Until now, all of the followed patients in our hospital have had a benign prognosis and no serious complications. However, the disease has increased in prevalence in recent years, and the number of cases has increased rapidly. Thus, additional observation is required to monitor long-term complications. As their primary goal is to reduce the damage to children, clinicians need to summarize their experiences in detail and perform clinical research. Additionally, we firmly believe that a ban on buckyballs and similar magnetic toys for minors is the most effective way to reduce the incidence of foreign magnetic body ingestion.
In recent years, the incidence of magnetic foreign body ingestion has increased rapidly in our hospital. Almost all of the ingested magnetic foreign bodies were magnetic beads. Most of the patients had intestinal perforations and suffered substantial damage.
Obvious differences exist in clinical symptoms between magnetic and non-magnetic foreign body ingestion. We aimed to summarize clinical experiences and optimize the diagnosis and treatment in dealing with this condition.
To summarize the valuable surgical experiences of multiple-magnet ingestion in children, such as no leakage of the intestinal contents in the abdominal cavity, ileus related symptoms and so on.
The experiences of surgeries within the recent 10 years were collected, and the clinical characteristics, treatment, and prognosis were summarized and analyzed. Several typical cases were selected and discussed.
Through the observational study of 56 cases, we are sure that the most effective way to reduce the increasingly high incidence of injury from magnetic foreign body ingestion is to ban the sale of powerful magnetic toys like buckyballs for minors, and keep children stay far away from the powerful magnetic toys in their living environments. Furthermore, magnetic beads causing intestinal perforation without intestinal content leakage is a discovery that can be used clinically. How to make an appropriate diagnosis and treatment plan to reduce the injury on children is an urgent problem to be solved.
The key way to reduce the incidence of magnetic foreign body ingestion is to ban the sale of magnetic toys. Clinicians can try new operation methods and determine the indications of this emergency according to the characteristic that intestinal contents will not leak into the abdominal cavity because the intestines stick together tightly. Meanwhile, additional observation is required to monitor long-term complications.
The direction of the future research is to reduce the incidence of multiple magnet ingestion, relieve the injury to patients, and apply minimally invasive technique in this emergency.
The authors thank the children and their parents for allowing us to publish the collected data. The authors also thank the staff of the Department of Radiology, and the Department of Gastroenterology for their cooperation.
Manuscript source: Unsolicited manuscript
Specialty type: Pediatrics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Karakuş OZ, Lima M S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Taher H, Azzam A, Khowailed O, Elseoudi M, Shaban M, Eltagy G. A case report of an asymptomatic male child with multiple entero-enteric fistulae post multiple magnet ingestion. Int J Surg Case Rep. 2019;58:50-53. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Bauman B, McEachron K, Goldman D, Louiselle A, Zheng E, Mills D, Louie J, Segura B. Emergency Management of the Ingested Magnet: An Algorithmic Approach. Pediatr Emerg Care. 2019;35:e141-e144. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ 2nd, Waring JP, Fanelli RD, Wheeler-Harbough J. American Society for Gastrointestinal Endoscopy. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002;55:802-806. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 399] [Cited by in F6Publishing: 339] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 4. | Kramer RE, Lerner DG, Lin T, Manfredi M, Shah M, Stephen TC, Gibbons TE, Pall H, Sahn B, McOmber M, Zacur G, Friedlander J, Quiros AJ, Fishman DS, Mamula P; North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition Endoscopy Committee. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr. 2015;60:562-574. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 308] [Cited by in F6Publishing: 295] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 5. | Hussain SZ, Bousvaros A, Gilger M, Mamula P, Gupta S, Kramer R, Noel RA. Management of ingested magnets in children. J Pediatr Gastroenterol Nutr. 2012;55:239-242. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 115] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 6. | Brown JC, Otjen JP, Drugas GT. Pediatric magnet ingestions: the dark side of the force. Am J Surg. 2014;207:754-9; discussion 759. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Wildhaber BE, Le Coultre C, Genin B. Ingestion of magnets: innocent in solitude, harmful in groups. J Pediatr Surg. 2005;40:e33-e35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Consumer Product Safety Commission of United States. CPSC Warns High-Powered Magnets and Children Make a Deadly Mix. Release number 12-037. Published November. 2011; Available from: http://www.cpsc.gov/cpscpub/prerel/prhtml12/12037.html. [Cited in This Article: ] |
| 9. | Kiefer K, Hottinger H, Kahn T, Ngo M, Ben-Amotz R. Magnet ingestion in dogs: two cases. J Am Anim Hosp Assoc. 2010;46:181-185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |