Published online Apr 6, 2019. doi: 10.12998/wjcc.v7.i7.881
Peer-review started: November 26, 2018
First decision: January 8, 2019
Revised: February 24, 2019
Accepted: March 16, 2019
Article in press: March 16, 2019
Published online: April 6, 2019
Congenital bronchobiliary fistula is a rare developmental abnormality with an abnormal fistula between the respiratory system and biliary tract. The aim of this report is to analyze and summarize the clinical features and experience of diagnosing and treating congenital bronchobiliary fistula (CBBF) occurring in the neonatal period.
The onset of symptoms was 3 d after birth in our patient with progressive cyanosis and respiratory distress, and a large amount of green fluid was noticed in her respiratory secretion. We performed computed tomography (CT), fiberoptic bronchoscopy, and cholangiography to make a diagnosis, as well as fistulography with a bronchoscope for the first time. These examinations provided us with valuable images to make a correct diagnosis. The fistula was dissected and removed with excellent results. Surgical removal of the fistula was successful, and the baby recovered well and was discharged. She has been followed for 4 mo without any signs of discomfort.
The main symptom of CBBF is bile-like sputum. CT, bronchoscopy, fistulography, and intraoperative cholangiography can provide important evidence for diagnosis. Surgical resection of the fistula is the first choice of treatment.
Core tip: Congenital bronchobiliary fistula is a rare developmental abnormality with an abnormal fistula between the respiratory system and biliary tract. We summarize the clinical data, and review related papers on it. The aim of this report is to analyze and summarize the clinical features and experience of diagnosing and treating congenital bronchobiliary fistula occurring in the neonatal period.
- Citation: Li TY, Zhang ZB. Congenital bronchobiliary fistula: A case report and review of the literature. World J Clin Cases 2019; 7(7): 881-890
- URL: https://www.wjgnet.com/2307-8960/full/v7/i7/881.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i7.881
Congenital bronchobiliary fistula (CBBF) is a rare developmental abnormality with an abnormal fistula between the respiratory system (trachea or bronchus) and biliary tract. Patients with this anomaly may develop symptoms at any time from neonate age to adulthood, but most of them present with signs of apnea, bilious saliva, and choking, within just a few days after birth. Generally, the earlier the symptoms appear, the more serious the condition is. CBBF is often accompanied by biliary tract developmental anomalies, such as biliary atresia. Surgical resection of the fistula is the ultimate choice of treatment. Presently, this anomaly is believed to be caused by abnormal development of the foregut[1-3]. In this paper, we describe a patient with CBBF who showed the symptom of apnea at 3 d after birth, summarize the clinical data, and review the related papers on CBBF.
Intermittent cyanosis for 3 d.
A full-term female baby of 5 d was referred to our hospital because of intermittent cyanosis. She secreted a large amount of yellowish and green saliva and started choking since 3 d of age. Respiratory distress became increasingly severe after admission, so tracheal intubation and a ventilator were applied thereafter. After intubation, yellowish green fluid kept flowing out of the tracheal tube. Gas-troesophageal reflux complicated by a tracheoesophageal fistula was considered first, but nasogastric depression produced colorless fluid, which was not in accordance with the aforementioned findings.
Jaundice.
Total bilirubin 172.4 μmol/L.
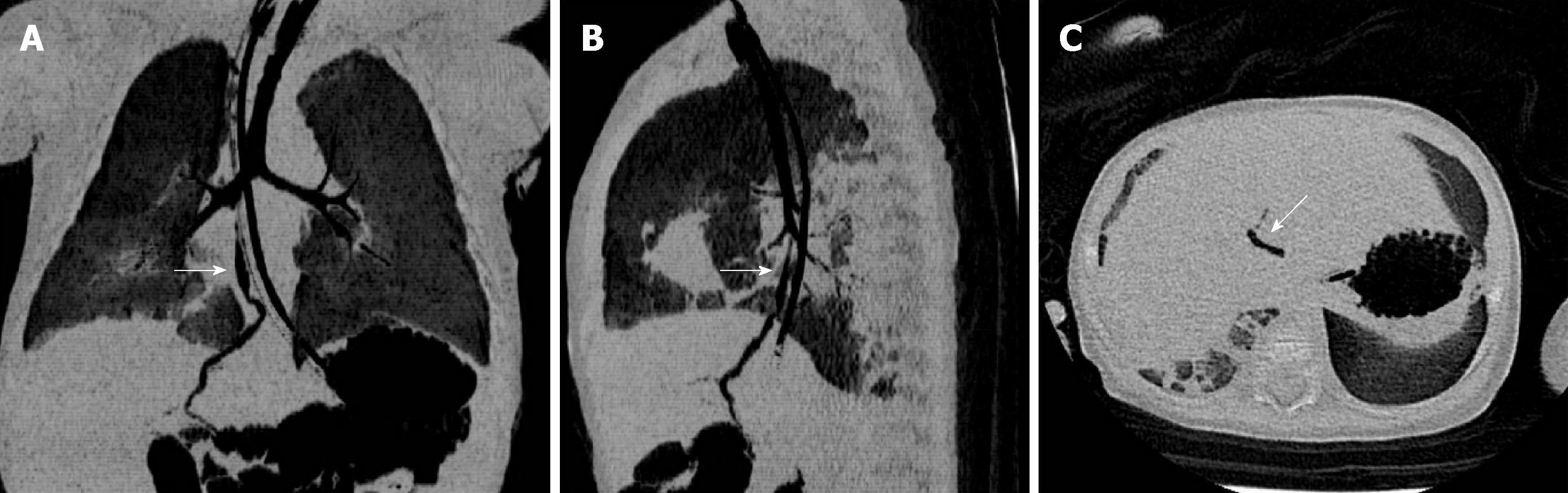
We performed 3-dimensional (3D) computed tomography (CT) of the baby’s chest. Her trachea and esophagus were reconstructed, and an abnormal fistula originated from the right bronchus; the fistula formed down along the esophagus and passed through the diaphragm into the intrahepatic biliary tract at the site of the esophageal hiatus. Gas was noticed in the intrahepatic biliary tract and common hepatic duct. Furthermore, pneumonia was evident in both lungs, especially in the lower lobes (Figure 1A-C). CBBF was diagnosed accordingly.
During the ultrasonographic examination, we discovered an abnormal fistula similar to that detected by CT. Ultrasonography also detected an accumulation of gas in both intrahepatic bile ducts, the common hepatic duct, and gallbladder, and gas bubbles in the biliary system moved with the patient’s breathing. No signs of biliary atresia were noticed during the ultrasonographic examination.
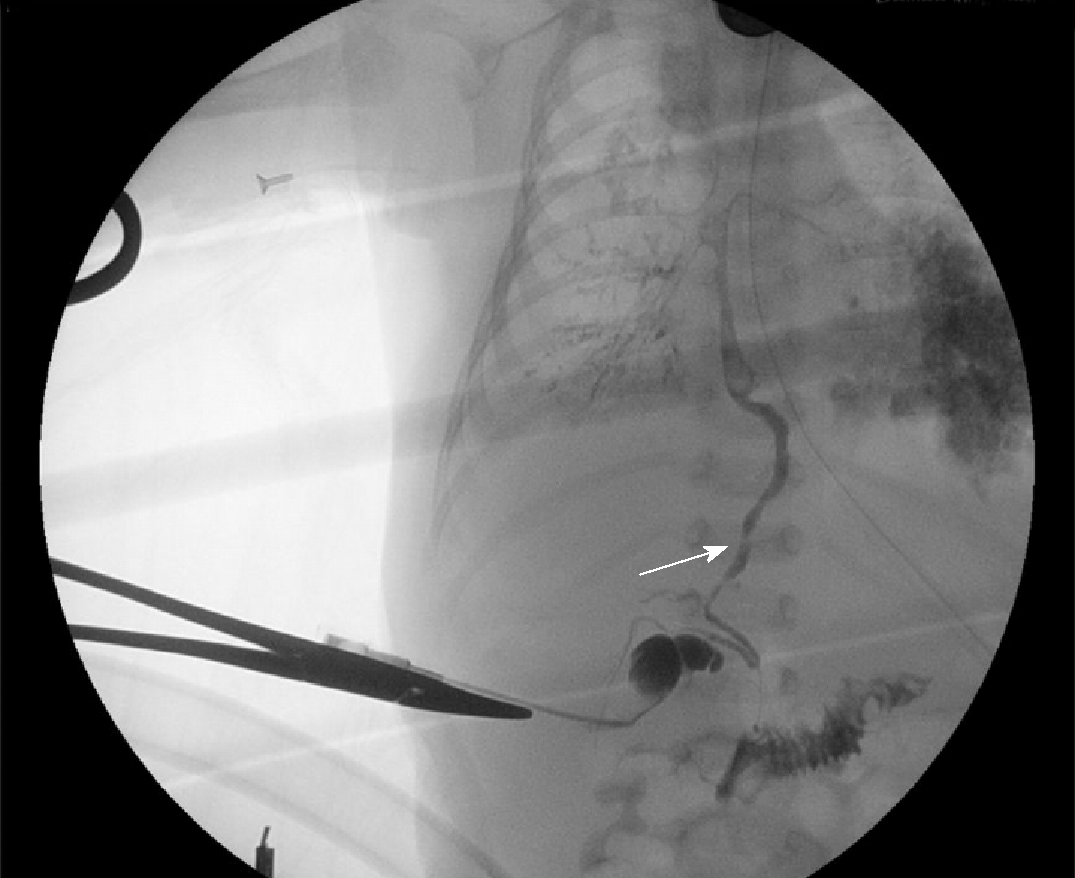
Flexible fiberoptic bronchoscopy showed an abnormal opening at the right main bronchus; contrast was injected via the opening, and beside radiography was performed, which showed the outlines of the fistula, biliary tract, gallbladder, and duodenum (Figure 2).
Congenital bronchobiliary fistula.
We initially performed laparoscopic biliary tract exploration and cholangiography to rule out biliary tract malformations. We found that the gallbladder was filled with green viscous bile, and the distal bile duct was patent. The abnormal fistula that bridged the intrahepatic bile duct and right bronchus was visible (Figure 3). Then, we performed posterolateral right thoracotomy at the sixth intercostal space. Green bile salt was deposited extensively beneath the visceral pleura. We dissected the mediastinal pleura and detected the fistula alongside the esophagus. The fistula formed down from the right bronchus to the right side of the hiatus, and it was about 4 mm in diameter and as soft as the esophagus. We punctured the lumen but produced nothing; then 10 mL of methylene blue was injected into the gallbladder, and the blue material was noticed subsequently at the puncture site and intratracheal tube (Figure 4). The fistula was confirmed accordingly. We separated the fistula and dissected it from the bronchus to the hiatus; both ends were securely ligated and sutured. Lastly, a thoracic drainage tube was placed.
On the day 3 postoperatively, the child was successfully weaned from the ventilator. She was in good condition with satisfactory pulmonary expansion and feeding tolerance. We attempted to remove the thoracic drainage tube but failed; subsequently, the baby developed pneumothorax and subcutaneous emphysema, which were considered due to improper operation, so the tube was reinserted. On day 7 postoperatively, the child developed cholestasis with a total bilirubin level of 71.6 μmol/L and conjugated bilirubin level of 58.1 μmol/L. Ultrasonography showed mild obstruction of the extrahepatic bile duct and slight dilation of the common bile duct. Two possibilities were considered: first, the extrahepatic bile duct was not patent enough to drain all the bile produced by the liver sufficiently; and second, in-flammation and edema caused by the operation resulted in partial obstruction of the bile duct. Methylprednisolone was administered, and her bilirubin level decreased to normal range 3 d later. On day 10 postoperatively, growing chylous fluid was noticed in the drainage, so the oral feeding was withdrawn accordingly. Ten days later, the drainage gradually decreased, oral feeding was resumed without adverse reactions, and the drainage tube was removed. The baby recovered well and was discharged. She has been followed for 4 mo without any signs of discomfort.
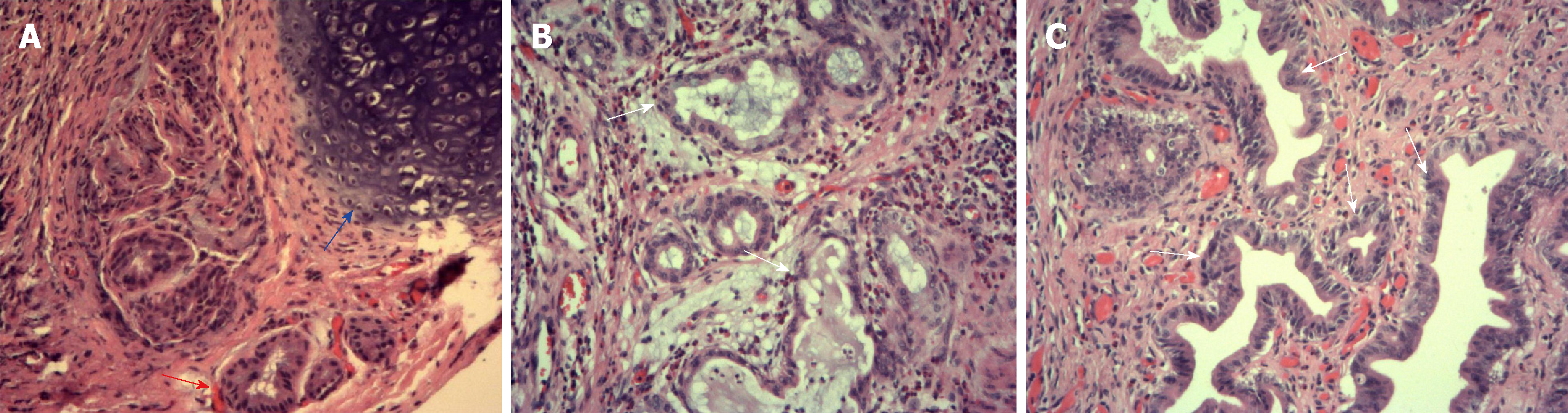
A microscopic examination was performed separately for three parts of the removed fistula. Scattered mature and naive hyaline cartilage surrounded by clustered bronchial glands could be seen at the part near to the bronchus. Hyperplasia, angulation, aggregation, and columniation of the biliary glandular epithelial cells were found at the biliary end. The middle part was characterized by scattered, clustered glands, columniation of the glandular epithelia, squamous metaplasia, and cartilaginous tissue around the bronchial glands (Figure 5A-C).
CBBF can manifest as a series of symptoms caused by an abnormal connection between the hepatic duct and trachea or bronchus. The onset time and severity of symptoms are related to the diameter of the fistula; therefore, the symptoms can appear at any age from newborn to adulthood. However, most of them occur in newborns and infants. The main clinical features of CBBF are recurrent coughing, bilious sputum, or bile-stained sputum in tracheal intubation. Patients generally develop progressive dyspnea, cyanosis, severe pneumonia, respiratory distress syndrome, and even apnea; shortly after birth, mechanical ventilation is often needed. Bile-stained expectoration is the most typical sign among the aforementioned symptoms. It has been often misdiagnosed as an esophagotracheal fistula, gastroesophageal reflux, aspiration pneumonia, or high intestinal obstruction[4,5].
The first findings on CBBF were reported in 1952 by Neuhauser et al[6]. Altogether, there were 43 additional cases reported in English and 1 in Chinese thereafter (Table 1), and CBBF was more common in women than in men. An abnormal fistula can be opened at different positions around the carina: right main bronchus (20/44, 45.4%), carina (19/44, 43.2%), and left main bronchus (5/44, 11.4%). Fistulas generally passed through the esophageal hiatus and entered into the abdominal cavity; all fistulas communicated with the intrahepatic bile duct (left hepatic duct), except one fistula that opened at the common bile duct[7].
| N | Year | Author | PMID | Type of fistula | Age | Sex | Diagnostic method | Operative method | Complications | Therapeutic effects |
| 1 | 2018 | Netto et al[36] | Tracheal carina | 21 d | F | CT | Surgical excision and ligation + selective left hepatectomy | None | Recovered after the hospital stay | |
| 2 | 2016 | Pérez et al[7] | 27606661 | Right main bronchus | 22 d | M | Bronchus examination and CT | Laparoscopic excision + left hepatectomy and cholangiopancreatostomy | Biliary dysplasia | Followed for 1 yr, normal |
| 3 | 2016 | Kwon et al[37] | 27000583 | Right main bronchus | 17 yr | M | Bronchus examination and CT and MR imaging | Laparoscopic resection and ligation | None | Followed for 10 mo, normal |
| 4 | 2015 | Kumar et al[38] | 26628766 | Right main bronchus | 3 yr | F | Bronchus examination | Surgical excision and ligation | None | Survived |
| 5 | 2015 | Kim et al[24] | 25555959 | Tracheal carina | 17 yr | M | Bronchus examination and CT | Surgical excision and ligation | None | Survived |
| 6 | 2015 | Mo et al[25] | 25617079 | Right main bronchus | 66 yr | M | Bronchus examination and CT | Wedge resection of the lung + resection of the intrahepatic tumor | Intrahepatic ductal papillary mucinous tumors | Survived |
| 7 | 2015 | Yu et al[26] | 27307938 | Tracheal carina | 5 d | M | Bronchus examination and CT | Right thoracotomy + Kasia procedure | Biliary dysplasia | Followed for 6 mo, normal |
| 8 | 2011 | Hodgdon et al[27] | 21827062 | Right main bronchus | 52 yr | F | CT | Surgical excision and ligation | None | Survived |
| 9 | 2011 | Sachdev et al[10] | 21516501 | Tracheal carina | 2 yr 10 mo | M | Bronchus examination and CT | Surgical excision and ligation | None | Followed for 1 yr, normal |
| 10 | 2011 | Kumagai et al[28] | 21297506 | Tracheal carina | 2 mo | F | Bronchus examination and MR imaging | Surgical excision and ligation | None | Followed for 7 mo, normal |
| 11 | 2010 | Tan et al[29] | 20672712 | Right main bronchus near carina | 51 yr | F | Bronchus examination and CT | Surgical excision and ligation | None | Recovered after the hospital stay |
| 12 | 2010 | Croes et al[30] | 20385268 | Tracheal carina | 3 d | F | Bronchus examination | Surgical excision and ligation | Biliary dysplasia | Survived |
| 13 | 2009 | Najdi et al[31] | 19586763 | Tracheal carina | 6 d | F | Bronchus examination and CT | Surgical excision and ligation | Meconium aspiration syndrome | Died on day 2 after surgery |
| 14 | 2009 | Günlemez et al[22] | 19101328 | Left main bronchus | 9 d | F | CT | Surgical excision and ligation | Extrahepatic biliary atresia | Followed for 9 mo, normal |
| 15 | 2008 | Uramoto et al[3] | 18628589 | Tracheal carina | 65 yr | F | Bronchus examination and CT | No surgery | Lung cancer | Died of lung cancer within 28 mo since diagnosis |
| 16 | 2008 | Chawla et al[20] | 18478221 | Tracheal carina | < 28 d | M | CT | Surgical excision and ligation | Biliary dysplasia | followed for 6 mo, normal |
| 17 | 2005 | Aguilar et al[32] | 16021209 | Tracheal carina | 6 yr | F | Bronchus examination | Surgical excision and ligation | None | Survived |
| 18 | 2004 | Hourigan et al[33] | 14605784 | Right main bronchus | 13 d | M | MR imaging | Right thoracotomy + Kasia procedure | Biliary dysplasia | Survived |
| 19 | 2002 | DiFiore et al[15] | 12149705 | Right main bronchus | < 28 d | M | Intuition intraoperatively | Surgical removal + right diaphragmatic hernia repair | Right diaphragmatic hernia | Survived |
| 20 | 2000 | Duong et al[17] | 10741248 | Tracheal carina | 3 yr | F | Bronchus examination | Surgical excision and ligation | None | Survived |
| 21 | 2000 | Tommasoni et al[14] | 10922138 | Tracheal carina | 1 yr 9 mo | F | Bronchus examination | Nissen procedure + surgical excision and ligation | Gastroesophageal reflux | Followed for 6 yr, normal |
| 22 | 2000 | Tommasoni et al[14] | 10922138 | Tracheal carina | 2 yr 6 mo | M | Bronchus examination and angiography | Surgical excision and ligation | Funnel chest | Followed for 4 yr, normal |
| 23 | 1998 | Fischer et al[34] | 9854540 | left main Bronchus | 16 d | F | Bronchus examination | Surgical excision and ligation | None | Survived |
| 24 | 1996 | Egrari et al[35] | 8783103 | Tracheal carina | 3 d | F | Bronchus examination | Surgical excision and ligation | None | Survived |
| 25 | 1996 | Nishimura et al[39] | 8741536 | Right main bronchus | 57 yr | F | CT | Surgical excision and ligation | None | Died |
| 26 | 1994 | Ferkol et al[19] | 8194299 | Left main bronchus | 23 d | M | Bronchus examination | Surgical excision and ligation | Biliary dysplasia | Died |
| 27 | 1995 | Tekant et al[5] | 8035264 | Tracheal carina | 15 d | F | Bronchus examination | Surgical excision and ligation | Biliary dysplasia | Survived |
| 28 | 1993 | Gauderer et al[4] | 8468661 | Tracheal carina | 2 yr | M | Bronchus examination | Surgical excision and ligation | Biliary dysplasia | Survived |
| 29 | 1990 | Yamaguchi et al[40] | 2371608 | Right main bronchus | 32 yr | M | Bronchus examination | Surgical excision and ligation | None | Survived |
| 30 | 1989 | Mavunda et al[41] | Left main bronchus | 1 yr | F | CT | Surgical excision and ligation | None | Survived | |
| 31 | 1988 | de Carvalho et al[42] | 3206388 | Right main bronchus | 32 yr | F | CT | Surgical excision and ligation | None | Followed for 1 yr, normal |
| 32 | 1987 | Levasseur et al[1] | 3632120 | Tracheal carina | 22 yr | F | Bronchus examination | Surgical excision and ligation | None | Survived |
| 33 | 1986 | Lindahl et al[18] | 3746610 | Right main bronchus | 15 d | F | Bronchus examination | Surgical excision and ligation | None | Survived |
| 34 | 1985 | Chang et al[9] | 4001424 | Right main bronchus | 12 h | M | Bronchus examination | Surgical excision and ligation | None | Survived |
| 35 | 1984 | Chan et al[12] | 6697133 | Right main bronchus | 4 d | F | Not mentioned | Surgical excision and ligation | Biliary dysplasia | Died |
| 36 | 1976 | Kalayoğlu et al[11] | 957073 | Right main bronchus | 4 d | F | Not mentioned | Surgical excision and ligation | None | Died |
| 37 | 1974 | Cuadros et al[43] | Tracheal carina | 6 yr | M | Bronchus examination | Surgical excision and ligation | None | Survived | |
| 38 | 1971 | Sane et al[8] | 5573334 | Right main bronchus | 4 wk | F | Bronchus examination | Surgical excision and ligation | None | Survived |
| 39 | 1970 | Wagget et al[44] | Left main bronchus | 3 wk | F | Bronchus examination | Surgical excision and ligation | Biliary dysplasia | Survived | |
| 40 | 1968 | Weitzman et al[45] | 5667415 | Right main bronchus | 2 yr 9 mo | M | Bronchus examination | Surgical excision and ligation | None | Survived |
| 41 | 1966 | Stigol et al[2] | 5902432 | Right main bronchus | 1 yr 2 mo | F | Bronchus examination | Surgical excision and ligation | None | Survived |
| 42 | 1963 | Enjoji et al[46] | Right main bronchus | 7 mo | M | Biopsy | No surgery | Biliary dysplasia | Died | |
| 43 | 1952 | Neuhauser et al[6] | 14914166 | Right main bronchus | 5 mo | F | Bronchus examination | No surgery | None | Died |
| 44 | 2013 | Zheng et al[23] | Tracheal carina | 27 d | F | Bronchus examination and CT | Surgical excision and ligation | Biliary atresia | Survived |
The pathogenesis of this disease is not clear yet. Abnormal development of the bronchial bud, which fuses with the bile duct, was regarded as the cause of the anomaly. Other reports postulated that CBBF was the result of digestive tract duplication and the upper respiratory tract[1,6,8-10].
As in most reports, the proximal part of the fistula had the characteristics of the respiratory tract, consisting of cartilage, pulmonary epithelia, glands, and smooth muscle, whereas the distal part was similar to the gastrointestinal tract. In our case, by examining the proximal, middle, and distal parts of the fistula, we found scattered mature hyaline cartilage, relatively naive cartilage, and clusters of bronchial glands at the bronchus end; whereas, glandular epithelia of the bile duct and interstitial cholestasis were found at the distal part of the fistula. In the middle part, the lumen was partly covered by pseudo-ciliated columnar epithelia. Cartilage rings lay beneath the mucosa. Co-existing single-layer columnar epithelium could also be seen in the same field. These histological findings could further verify the pathogenesis of CBBF.
CBBF was often complicated by biliary atresia, diaphragmatic hernia, esophagus atresia, and tracheoesophageal fistula, and the incidence of biliary malformation in this group was about 30%[11-15]. As long as this possibility was considered, the diagnosis of CBBF was not difficult. Magnetic resonance imaging, 3D-CT reconstruction, bronchoscopy, and ultrasonography can provide valuable clues. Bronchoscopy was the most common method for making a diagnosis, as it can be used to find the abnormal opening of the fistula and the overflowing bile via the opening[13,14,16-19]. 3D-CT reconstruction can accurately detect the existence of the fistula, which is of great significance for diagnosing CBBF. In the present case, the CT scan provided us with the first evidence of the abnormal fistula. Then fiberoptic bronchoscopy was performed, and a contrast dye was injected into the fistula once the opening was confirmed. Next, a radiographic examination was conducted; thus, the opening, shape, and connection of the fistula were all confirmed. The result of our treatment was excellent, and to our knowledge, this method has not been reported previously.
Surgical resection was the ultimate treatment of choice, but a specific method must be considered according to different anatomical structures[20-22]. According to previous reports, different kinds of operative methods have been used, such as hepatic lobectomy, anastomosis of the gallbladder or intestine with abnormal fistulas, and fistula resection. We think that it is necessary to consider whether there is a biliary tract anomaly when preparing an operative plan. If a biliary anomaly exists, biliary reconstruction must be considered[4,14]. We performed laparoscopic cholangiography first during the operation to exclude biliary atresia, and achieved a satisfactory result. We performed thoracotomy subsequently, and explored and identified the fistula in the mediastinum; the fistula formed down the right side of the esophagus. We punctured the lumen for assurance because there are many important structures nearby, and then we injected methylene blue into the gallbladder; the dye was seen flowing out of the puncture site, thus the fistula was confirmed. Because the extrahepatic biliary tract was normal, reconstruction was unnecessarily considered. Instead, we just separated the fistula and ligated and sutured it at the upper end and at the hiatus, and then the fistula was removed.
The overall mortality of CBBF was 15.91% (7/44) according to the literature, and three patients died of respiratory complications without surgery. Our patient experienced chylothorax shortly after thoracotomy, which may be due to injury of the thoracic duct when we dissected the fistula at the hiatus. Fortunately, she recovered after short-term conservative management. Cholestasis was another main complication encountered postoperatively, and ultrasonography showed slight dilatation of the bile duct. We evaluated her conditions and prescribed methy-lprednisolone. Cholestasis resolved after three doses; therefore, we deduced that the jaundice may have been due to temporary inflammation of the biliary tract.
Most surgeons may not encounter CBBF in their professional career considering its rarity. Its clinical symptoms are typical and special such as bile-stained expectoration. As long as surgeons have some insight into this kind of condition, its diagnosis and treatment are not difficult, and the prognosis would be excellent for most patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fekaj E, Balta AZ, Barik R S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Levasseur P, Navajas M. Congenital tracheobiliary fistula. Ann Thorac Surg. 1987;44:318-319. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Stigol LC, Traversaro J, Trigo ER. Carinal trifurcation with congenital tracheobiliary fistula. Pediatrics. 1966;37:89-91. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 3. | Uramoto H, Kawano O, Sugimoto M, Yamagata H, Kohrogi H. Congenital bronchobiliary fistula in a 65-year-old woman. Intern Med. 2008;47:1367-1370. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Gauderer MW, Oiticica C, Bishop HC. Congenital bronchobiliary fistula: management of the involved hepatic segment. J Pediatr Surg. 1993;28:452-455. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Tekant GA, Joseph VT, Cheah SL. Congenital tracheobiliary fistula. J Pediatr Surg. 1994;29:594-595. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Neuhauser EB, Elkin M, Landing B. Congenital direct communication between biliary system and respiratory tract. AMA Am J Dis Child. 1952;83:654-659. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Pérez CG, Reusmann A; Collaborators. [Congenital broncho-biliary fistula: a case report]. Arch Argent Pediatr. 2016;114:e350-e353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Sane SM, Sieber WK, Girdany BR. Congenital bronchobiliary fistula. Surgery. 1971;69:599-608. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 9. | Chang CC, Giulian BB. Congenital bronchobiliary fistula. Radiology. 1985;156:82. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Sachdev A, Chugh K, Krishana A, Gupta D. Congenital tracheobiliary fistula: a case report with review of literature. Pediatr Surg Int. 2011;27:899-905. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Kalayoğlu M, Olcay I. Congenital bronchobiliary fistula associated with esophageal atresia and tracheo-esophageal fistula. J Pediatr Surg. 1976;11:463-464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 31] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Chan YT, Ng WD, Mak WP, Kwong ML, Chow CB. Congenital bronchobiliary fistula associated with biliary atresia. Br J Surg. 1984;71:240-241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Barlocco EG, Valletta EA, Cecchetto G, Previtera C, Giusti F, Mastella G. Tracheobiliary fistula: troublesome diagnoses in two children. Pediatr Pulmonol. 1992;14:243-246. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Tommasoni N, Gamba PG, Midrio P, Guglielmi M. Congenital tracheobiliary fistula. Pediatr Pulmonol. 2000;30:149-152. [PubMed] [Cited in This Article: ] |
| 15. | DiFiore JW, Alexander F. Congenital bronchobiliary fistula in association with right-sided congenital diaphragmatic hernia. J Pediatr Surg. 2002;37:1208-1209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Bringas Bollada M, Cabezas Martín MH, Martínez Sagasti F, Ortuño Andériz F. [Congenital bronchobiliary fistula diagnosed in adult age]. Med Intensiva. 2006;30:475-476. [PubMed] [Cited in This Article: ] |
| 17. | Duong M, Lund-Sørensen K, Sveinbjørnsson I, Mortensen PM. [Congenital tracheobiliary fistula]. Ugeskr Laeger. 2000;162:1085-1086. [PubMed] [Cited in This Article: ] |
| 18. | Lindahl H, Nyman R. Congenital bronchobiliary fistula successfully treated at the age of three days. J Pediatr Surg. 1986;21:734-735. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Ferkol T, McDowell KM, Gauderer MW, Alpert SE. Sinopulmonary manifestations of congenital bronchobiliary fistula. Clin Pediatr (Phila). 1994;33:181-184. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Chawla SC, Jha P, Breiman R, Farmer D, Gooding C. Congenital tracheobiliary fistula diagnosed with contrast-enhanced CT and 3-D reformation. Pediatr Radiol. 2008;38:999-1002. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Na KJ, Jung JC, Hwang Y, Lee HJ, Park IK, Kang CH, Jang JY, Kim YT. Minimally Invasive Surgical Repair for Congenital Bronchobiliary Fistula in an Adult. Ann Thorac Surg. 2016;101:1584-1587. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Günlemez A, Tugay M, Elemen L, Türker G, Gürcan NI, Demir H, Gürbüz Y, Hosten T. Surgical experience in a baby with congenital broncho-biliary fistula. Ann Thorac Surg. 2009;87:318-320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Li K, Zheng S, Xiao XM, Cao Y, Wang LS. Neonatal congenital bronchobiliary fistula:a case report and literature review. Chin J Pediatr Surg. 2013;34:447-449. [DOI] [Cited in This Article: ] |
| 24. | Kim JS, Suh JH, Park CB, Yoon JS. Congenital tracheobiliary fistula in an adolescent patient. Ann Thorac Surg. 2015;99:328-331. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Mo A, Brat G, Spolverato G, Pawlik TM. Intraductal papillary mucinous neoplasm of the liver: GI image. J Gastrointest Surg. 2015;19:792-794. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Yu H, Stavas JM, Joseph M. Congenital tracheobiliary fistula combined with hypoplastic common hepatic duct: Management by percutaneous transhepatic drainage. Radiol Case Rep. 2015;6:564. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Hodgdon IA, Thurston RS. Bronchobiliary fistula: a case report. J La State Med Soc. 2011;163:148-150. [PubMed] [Cited in This Article: ] |
| 28. | Kumagai T, Higuchi R, Riko M, Hiramatsu C, Sugimoto T, Okutani T, Yoshikawa N, Watanabe T, Takifuji K. Neonatal tracheobiliary fistula diagnosed by MR cholangiopancreatography. J Pediatr Gastroenterol Nutr. 2011;52:370-372. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Tan Q, Zheng B, Wang J. [A case report of congenital bronchobiliary fistula in adults]. Zhongguo Fei Ai Za Zhi. 2010;13:87-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 30. | Croes F, van Nieuwaal NH, van Heijst AF, van Enk GJ. Congenital tracheobiliary fistula. J Pediatr Surg. 2010;45:E9-11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Najdi T, Sibai H, Zineddine A, Sakhi A, Habzi A, Lahbabi MS, Benomar S. [Congenital bronchobiliary fistula: a case report]. Arch Pediatr. 2009;16:1137-1141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Aguilar C, Cano R, Camasca A, Gonzáles J, Rivera J, Del Pino T, Untiveros A. Congenital bronchobiliary fistula detected by cholescintigraphy. Rev Gastroenterol Peru. 2005;25:216-218. [PubMed] [Cited in This Article: ] |
| 33. | Hourigan JS, Carr MG, Burton EM, Ledbetter JC. Congenital bronchobiliary fistula: MRI appearance. Pediatr Radiol. 2004;34:348-350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 34. | Fischer JD. Bronchobiliary fistula: a case report. Can J Surg. 1998;41:470-472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 35. | Egrari S, Krishnamoorthy M, Yee CA, Applebaum H. Congenital bronchobiliary fistula: diagnosis and postoperative surveillance with HIDA scan. J Pediatr Surg. 1996;31:785-786. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Netto AS, Silva PCM, Vicentine FPP, Takamatsu FY, Gonzalez AM, Succi JE, Martins JL. Congenital tracheo-biliary fistula: staged surgical treatment. JPS Case Reports. 2018;32:11-13. [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Na KJ, Jung JC, Hwang Y, Lee HJ, Park IK, Kang CH, Jang JY, Kim YT. Minimally Invasive Surgical Repair for Congenital Bronchobiliary Fistula in an Adult. Ann Thorac Surg. 2016;101:1584-1587. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 38. | Kumar P, Mehta P, Ismail J, Agarwala S, Jana M, Lodha R, Kabra SK. Brocho-biliary fistula: A rare complication after ruptured liver abscess in a 3½ year old child. Lung India. 2015;32:489-491. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | Nishimura S, Nakagawa Y, Sakata T, Suga M, Ando M. [Bronchobiliary fistula]. Nihon Kyobu Shikkan Gakkai Zasshi. 1996;34:689-693. [PubMed] [Cited in This Article: ] |
| 40. | Yamaguchi M, Kanamori K, Fujimura M, Watanabe Y, Matsuda T. Congenital bronchobiliary fistula in adults. South Med J. 1990;83:851-852. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 41. | Mavunda K, Heiba S, Oiticica C, Sfakianakis GN, Birriel JA, Mckey RM. Congenital bronchobiliary fistula. Diagnosis by hepatobiliary scintigraphy. Respiratory Care. 1989;34:731-733. [Cited in This Article: ] |
| 42. | de Carvalho CR, Barbas CS, Guarnieri RM, de Campos JR, Filomeno LT, Saldiva PH, Barbas Filho JV. Congenital bronchobiliary fistula: first case in an adult. Thorax. 1988;43:792-793. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 43. | Cuadros J, Arkansay A, Nistral M, Montereo J. Fistula tra`queobiliar conge′nita. An Esp Pediatr. 1974;7:256–262. [Cited in This Article: ] |
| 44. | Wagget J, Stool S, Bishop HC, Kurtz MB. Congenital bronchobiliary fistula. J Pediatr Surg. 1970;5:566-569. [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 27] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 45. | Weitzman JJ, Cohen SR, Woods LO, Chadwick DL. Congenital bronchobiliary fistula. J Pediatr. 1968;73:329-334. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 46. | Enjoji M, Nakamura Y, Watanabe H. A case report-congenital biliotracheal fistula with trifurcation of bronchi. Annales paediatrici. 1963;200:321. [Cited in This Article: ] |