Published online Oct 26, 2019. doi: 10.12998/wjcc.v7.i20.3296
Peer-review started: April 30, 2019
First decision: September 9, 2019
Revised: September 19, 2019
Accepted: September 25, 2019
Article in press: September 25, 2019
Published online: October 26, 2019
The de Winter electrocardiography (ECG) pattern is a sign that implies proximal left anterior descending coronary artery occlusion in patients with chest pain. The previous view was that the de Winter ECG pattern is static.
A 65-year-old man presented with sudden chest pain at rest associated with diaphoresis for 55 min. The first ECG showed only T-wave inversion in III and aVF leads. Another ECG was performed at the 100th minute, showing upsloping ST segments depressed with tall and symmetrical T waves in the precordial leads; the J point was raised by 0.1 mV at the aVR lead. The patient was referred to our catheterization laboratory. A third ECG showed ST segment elevation by 0.2 mV in the I and aVL leads. The patient underwent emergency coronary angiography, which revealed complete proximal left anterior descending coronary (LAD) occlusion. The second patient presented with a 1-h history of sudden-onset, severe, substernal crushing chest pain. The first ECG showed ST-segment elevation (0.1–1.7 mV) in I, aVL, and precordial leads. The patient was referred to the catheterization laboratory. On arrival, his symptoms alleviated, and ECG showed that the ST-segments had significantly fallen back. The third ECG showed a typical de Winter pattern. Coronary angiography revealed 99% stenosis of the middle LAD.
The de Winter ECG pattern is transient and dynamic, and it reflects proximal or mid-LAD subtotal occlusion rather than total occlusion.
Core tip: The de Winter electrocardiography pattern is a sign that implies proximal left anterior descending coronary artery occlusion in patients with chest pain. The classic thinking of the de Winter pattern is that it represents a static situation. Our cases demonstrate that de Winter and ST-segment elevation myocardial infarction represent a dynamic spectrum that may evolve in either direction, i.e., toward coronary vessel occlusion or toward thrombolysis.
- Citation: Lin YY, Wen YD, Wu GL, Xu XD. De Winter syndrome and ST-segment elevation myocardial infarction can evolve into one another: Report of two cases. World J Clin Cases 2019; 7(20): 3296-3302
- URL: https://www.wjgnet.com/2307-8960/full/v7/i20/3296.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i20.3296
The de Winter electrocardiography (ECG) pattern is a sign that implies proximal left anterior descending coronary artery occlusion in patients with chest pain. The previous view was that the de Winter ECG pattern is static. We show that de Winter and ST-segment elevation myocardial infarction can evolve into one another.
Case 1: A 65-year-old man presented with sudden chest pain at rest associated with diaphoresis. He had no complaint of abdominal pain, bloody stools, or weight loss.
Case 2: A 50-year-old man presented with sudden-onset, severe, substernal crushing chest pain radiating to the left shoulder and back, accompanied by diaphoresis. He had no complaint of bloody stools, cough, or hemoptysis.
Case 1: The patient’s symptoms started 55 min ago and did not alleviate throughout the course of the disease.
Case 2: The patient’s symptoms started 1 h ago, when he was referred to our Emergency Department, and alleviated, but chest pain recurred after 81 min.
Case 1: He has a history of hypertension for 26 years and diabetes for 12 years.
Case 2: He has a history of hyperlipidemia for 4 years.
Case 1: The patient’s temperature was 36.7 °C, heart rate was 80 bpm, respiratory rate was 14 breaths per minute, blood pressure was 111/75 mmHg, and the oxygen saturation was 98% while the patient was breathing ambient air. The S1 and S2 were normal and there was no evidence of a heart murmur on cardiac examination.
Case 2: The patient’s temperature was 37.4 °C, heart rate was 96 bpm, respiratory rate was 20 breaths per minute, blood pressure was 103/85 mmHg, and oxygen saturation was 98% on ambient air. The S1 and S2 heart sounds were normal and there was no murmur on cardiac auscultation.
Case 1: His troponin T level was 0.049 ng/mL (normal value: 0.010–0.023), myoglobin level was 45 μg/L (normal value: 20–80), pro-BNP was 94 μg/L (normal value: < 300), CK-MB was 3.4ng/L (normal value: 0- 7.2), and D-dimer was 338 μg/L (normal value: < 500).
Case 2: His troponin I level was 20.93 ng/mL (normal value: 0.000-0.080), myoglobin level was 5520.2 ng/mL (normal value: 0-154.9), BNP was 75.5 pg/mL (normal value: < 100), CK-MB was 146.7 ng/mL (normal value: 0-7.2), D-dimer was 5.14 μg/mL (normal value: 0.00-0.55).
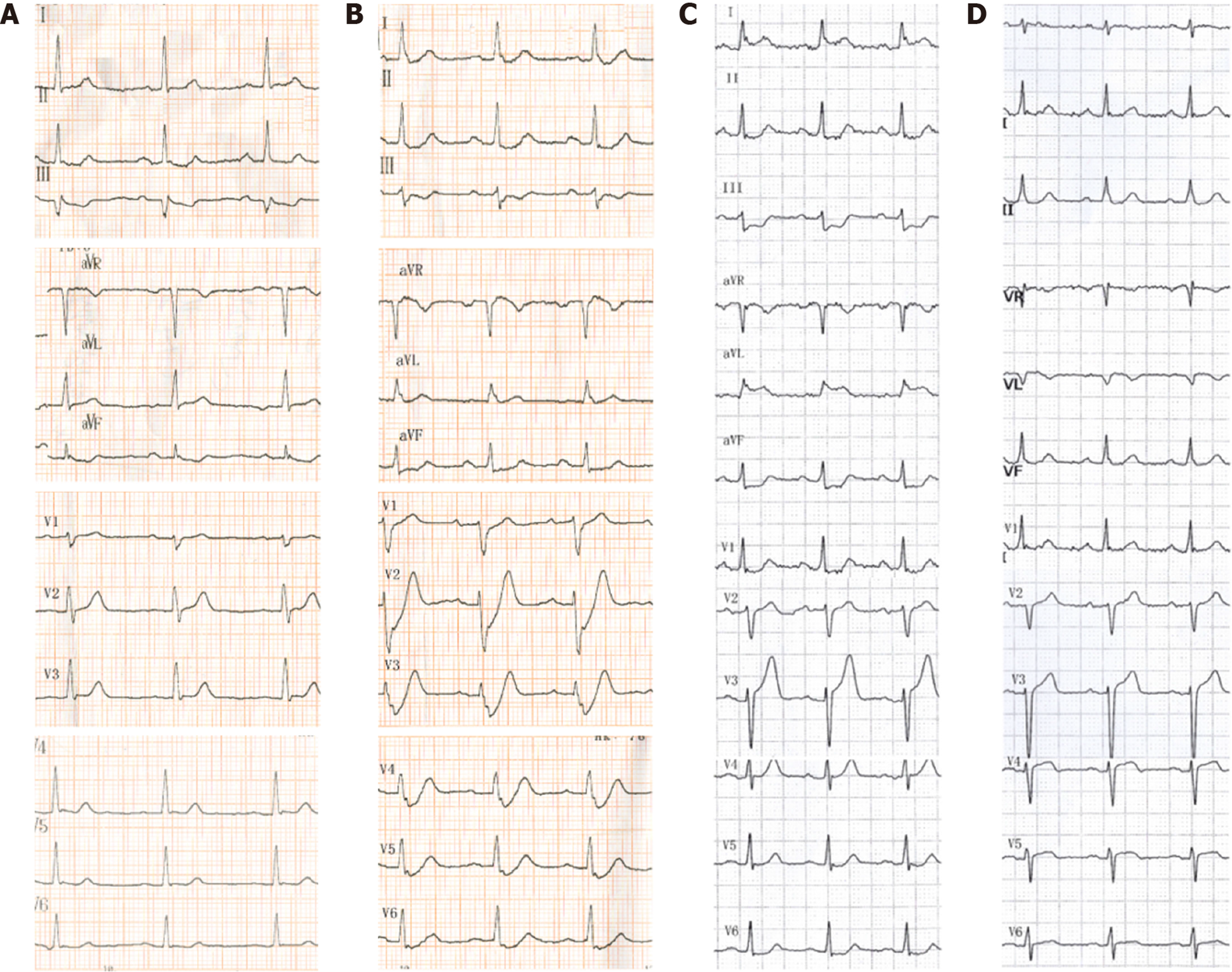
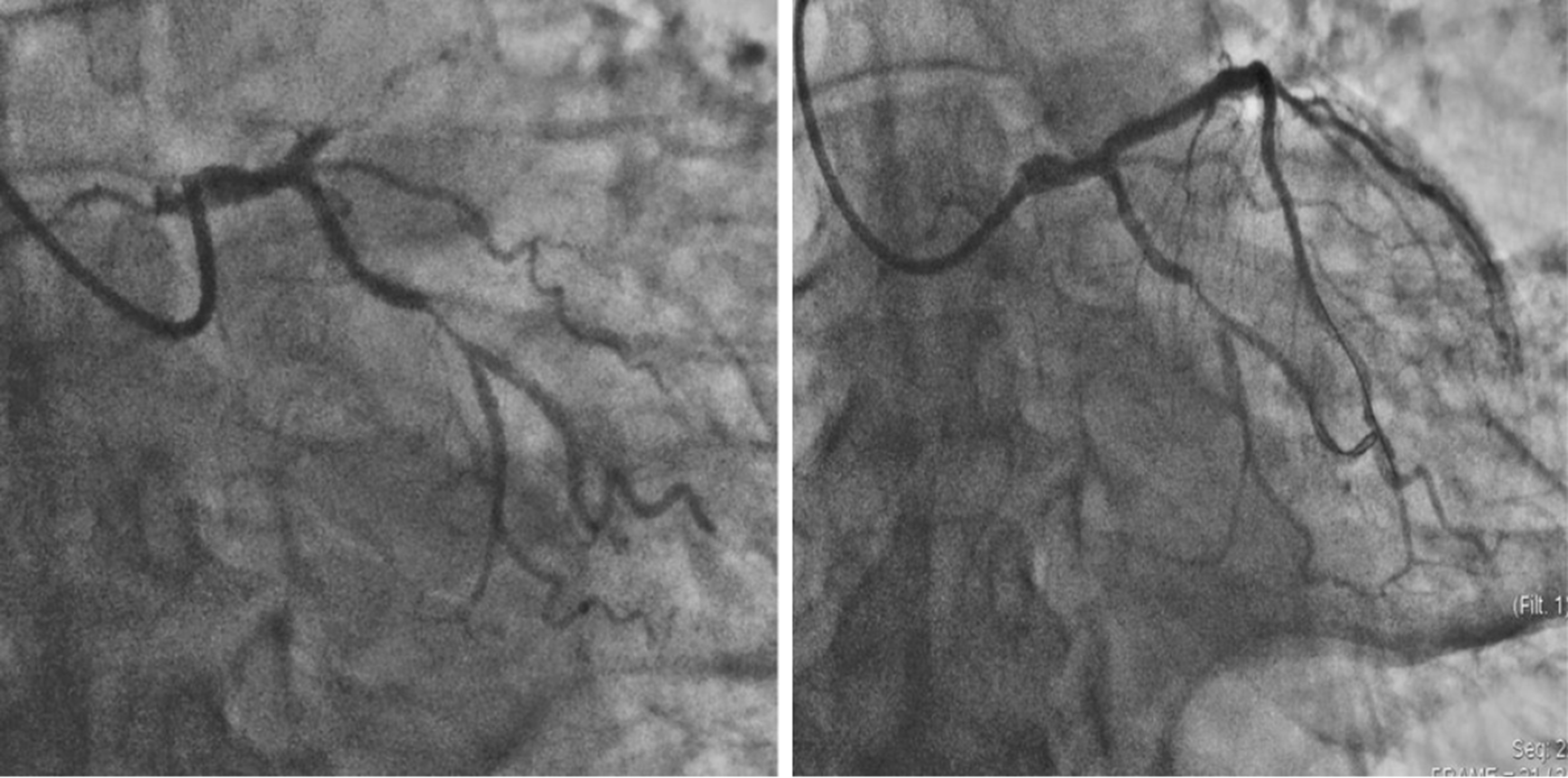
Case 1: The first ECG (Figure 1A), performed immediately in the emergency department, showed only T-wave inversion in the III and aVF leads. Another ECG (Figure 1B) was performed at the 100th minute, showing upsloping ST segments depressed by > 0.1 mV in the V1-V6 leads, with tall and symmetrical T waves in the precordial leads; the J point was raised by 0.1 mV in the aVR lead, and there was a loss of precordial R-wave progression. A third ECG, performed at hospital arrival (Figure 1C), showed ST segment elevation by 0.2 mV in the I and aVL leads. The emergency coronary angiography revealed multi-vessel disease and complete proximal left anterior descending coronary (LAD) occlusion (Figure 2). The post-procedural ECG is shown in Figure 1D.
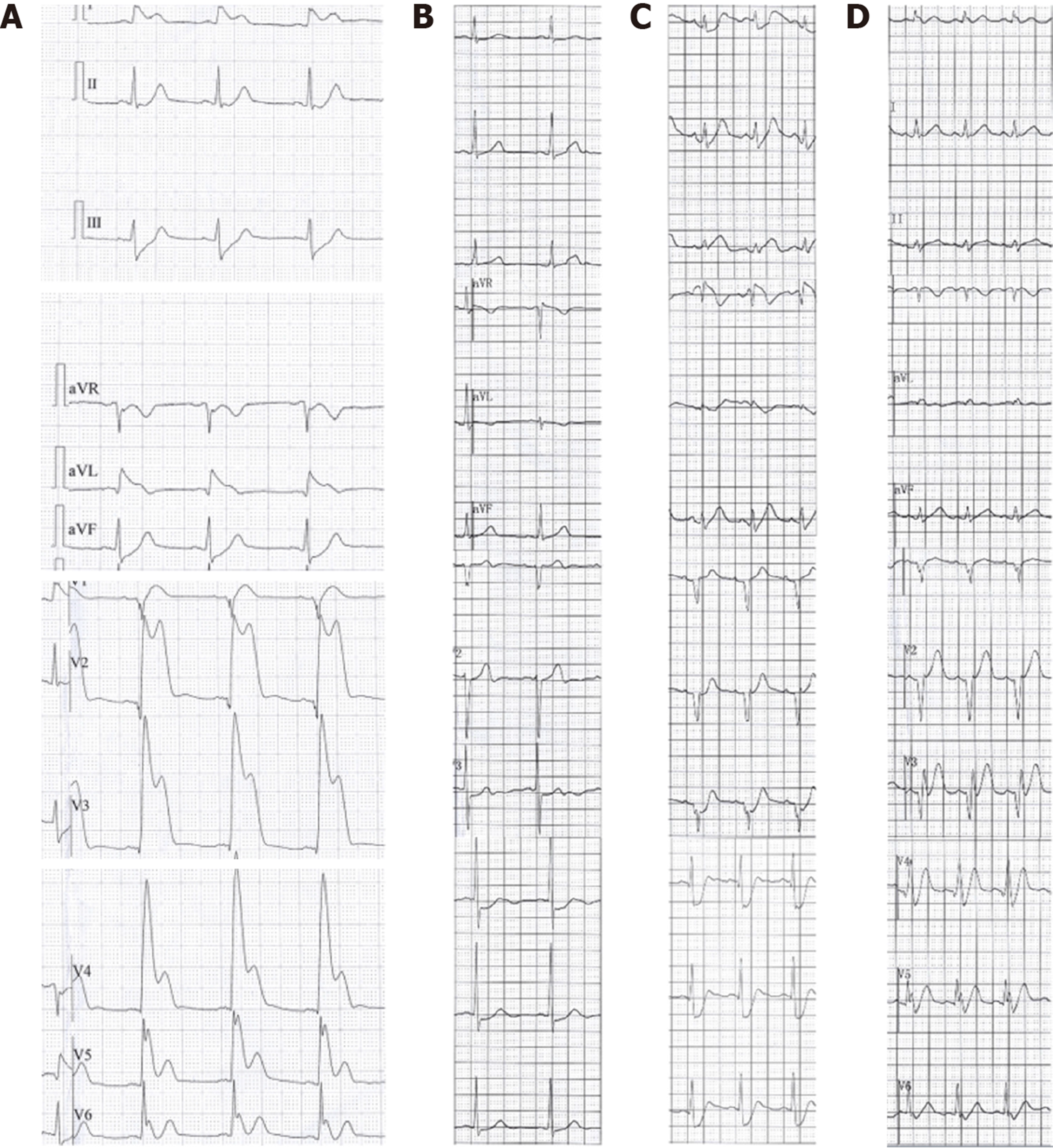
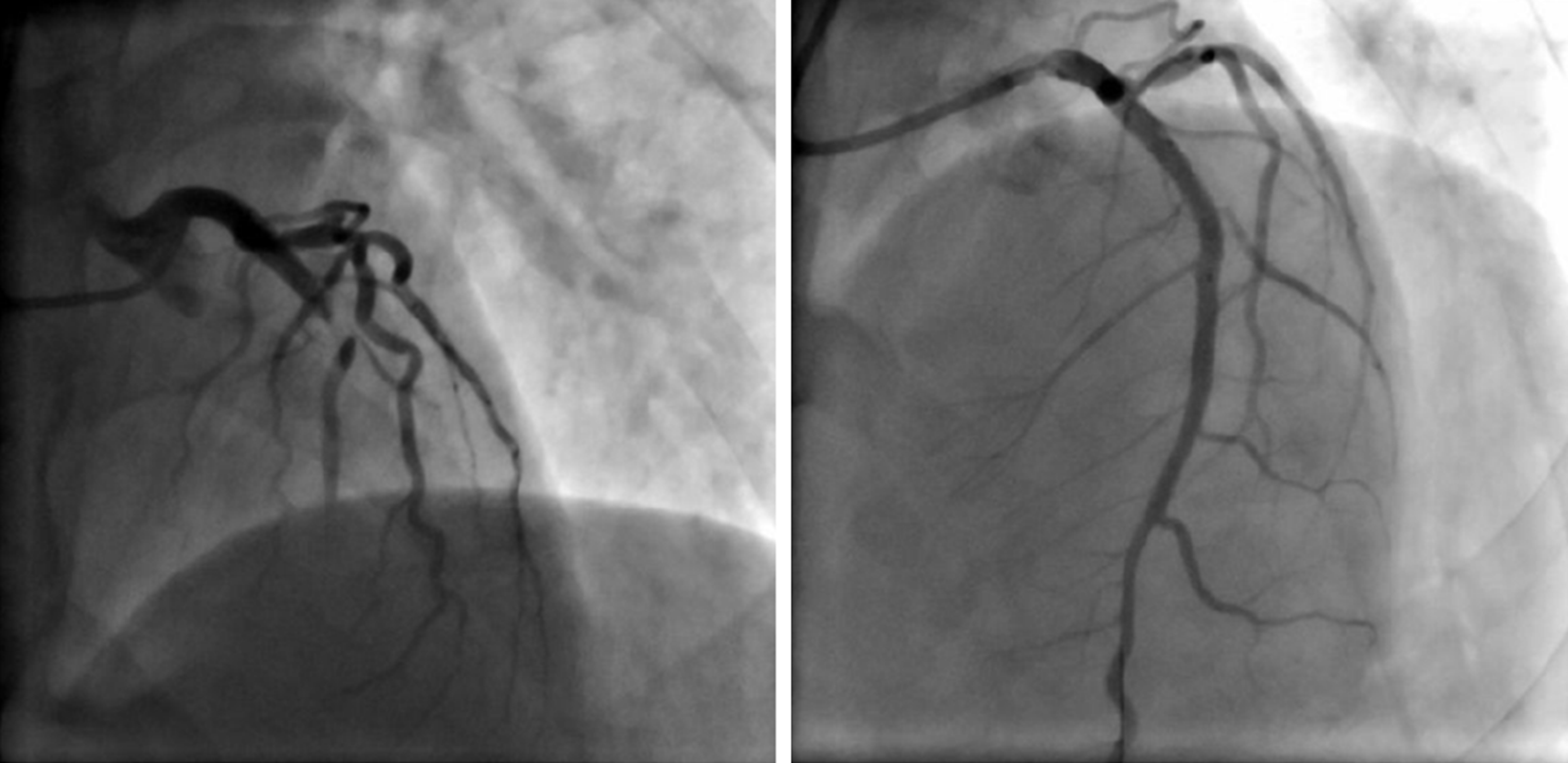
Case 2: The first ECG showed ST-segment elevation (0.1–1.7 mV) in I, aVL, and precordial leads (Figure 3A). The second ECG showed that the ST-segments had significantly fallen back (Figure 3B). The patient experienced chest pain recurrence after 81 min, and ECG showed a typical de Winter pattern (Figure 3C). The pre-emergency coronary angiography ECG is shown in Figure 3D. Coronary angiography revealed 99% stenosis of the middle LAD (Figure 4).
According to the symptoms and the electrocardiograms and coronary angiograms, this patient was diagnosed with de Winter syndrome at first, which then evolved to ST-segment elevation myocardial infarction (STEMI).
According to the symptoms and the electrocardiograms and coronary angiograms, this patient was diagnosed with STEMI at first, which then evolved to de Winter syndrome.
The patient underwent percutaneous coronary intervention in the LAD using a 3.0 mm × 38 mm stent.
The lesion was treated with a drug-eluting stent (3.5 mm × 18 mm).
No complications occurred in hospital, and the patient was discharged free of chest pain 5 d later. During outpatient follow-up, he had no characteristic clinical symptoms. No evidence of myocardial ischemia was noted in the routine examinations.
No complications developed during hospitalization, and the patient was discharged on the ninth day of hospitalization. During outpatient follow-up, he had no characteristic clinical symptoms. No evidence of myocardial ischemia was noticed in the routine examinations.
The de Winter ECG pattern (ST-segment upsloping depression and tall, positive symmetrical T waves; ST-elevation (1–2 mm) in lead aVR; a loss of precordial R-wave progression; and QRS complexes not widened or slightly widened) was first described by de Winter in 2008[1]. The key diagnostic features of the de Winter ECG pattern include the follow two points: (A) ST-segment upsloping depression > 1 mm with tall and positive symmetrical T waves in the precordial leads; and (B) ST-segment elevation in the aVR lead[2-4]. The previous view of this ECG pattern was that it is static and indicates complete proximal LAD occlusion[1,4]. However, our two cases demonstrate that the ECG pattern of de Winter syndrome and STEMI can evolve into one another. The first patient evolved from de Winter syndrome to STEMI after 72 min, and coronary angiography revealed complete proximal LAD occlusion. The second patient transformed from STEMI to de Winter syndrome after 2 h, and a 99% middle LAD stenosis was confirmed by coronary angiography. Goebel et al[5] reported a case of de Winter pattern progressing to STEMI within several hours and Lam et al[6] described a patient who spontaneously transformed from STEMI to de Winter pattern before emergency angiography and reperfusion therapy, which are similar to our present cases. Therefore, we believe that the de Winter ECG pattern reflects a coronary thrombus in formation which, however, has not completely occluded the coronary arteries. The ECG pattern of STEMI changes to the de Winter syndrome owing to autolysis of the intracoronary thrombus. Therefore, we believe the de Winter ECG pattern is transient, and either progresses to STEMI when the thrombus continues to form and completely occludes the coronary arteries, or the thrombus autolyzes and the ECG tends to become normal. Zhao et al[7] also showed spontaneous recanalization of the thrombus in a patient with de Winter syndrome. Pica et al[8] reported a case of acute stent thrombosis with de Winter ECG pattern, after thrombectomy and ballooning, the de Winter ECG pattern with typical ECG evolution as STEMI. What’s more, our second patient showed an elevated D-dimer value of 5.14 ug/mL, which reflected autolysis of the intracoronary thrombus. In essence, de Winter syndrome may be a thrombotic disease. The two patients with de Winter syndrome reported by Rao et al[9] and Pranata et al[10], who were treated successfully with thrombolytic therapy, support this opinion.
The de Winter ECG pattern is transient and dynamic, and it reflects proximal or mid-LAD subtotal occlusion rather than total occlusion. Physicians and others who attend patients with chest pain should be able to early recognize this STEMI-equivalent ECG pattern and need to perform urgent angiography and reperfusion therapy to improve the clinical outcomes of these patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hochholzer W S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Liu JH
| 1. | de Winter RJ, Verouden NJ, Wellens HJ, Wilde AA; Interventional Cardiology Group of the Academic Medical Center. A new ECG sign of proximal LAD occlusion. N Engl J Med. 2008;359:2071-2073. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 251] [Cited by in F6Publishing: 237] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 2. | Martínez-Losas P, Fernández-Jiménez R. de Winter syndrome. CMAJ. 2016;188:528. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | de Winter RW, Adams R, Verouden NJ, de Winter RJ. Precordial junctional ST-segment depression with tall symmetric T-waves signifying proximal LAD occlusion, case reports of STEMI equivalence. J Electrocardiol. 2016;49:76-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Verouden NJ, Koch KT, Peters RJ, Henriques JP, Baan J, van der Schaaf RJ, Vis MM, Tijssen JG, Piek JJ, Wellens HJ, Wilde AA, de Winter RJ. Persistent precordial "hyperacute" T-waves signify proximal left anterior descending artery occlusion. Heart. 2009;95:1701-1706. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 5. | Goebel M, Bledsoe J, Orford JL, Mattu A, Brady WJ. A new ST-segment elevation myocardial infarction equivalent pattern? Prominent T wave and J-point depression in the precordial leads associated with ST-segment elevation in lead aVr. Am J Emerg Med. 2014;32:287.e5-287.e8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Lam RPK, Cheung ACK, Wai AKC, Wong RTM, Tse TS. The de Winter ECG pattern occurred after ST-segment elevation in a patient with chest pain. Intern Emerg Med. 2019;14:807-809. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Zhao YT, Wang L, Yi Z. Evolvement to the de Winter electrocardiographic pattern. Am J Emerg Med. 2016;34:330-332. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Pica S, Ballestrero G, Pistis G, Crimi G. Acute stent thrombosis unveils two electrocardiogram patterns in a patient with 'De Winter T-waves' anterior myocardial infarction. Eur Heart J. 2016;37:2735. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Rao MY, Wang YL, Zhang GR, Zhang Y, Liu T, Guo AJ, Li L, Zhou K, Wang M. Thrombolytic therapy to the patients with de Winter electrocardiographic pattern, is it right? QJM. 2018;111:125-127. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Pranata R, Huang I, Damay V. Should de Winter T-Wave Electrocardiography Pattern Be Treated as ST-Segment Elevation Myocardial Infarction Equivalent with Consequent Reperfusion? A Dilemmatic Experience in Rural Area of Indonesia. Case Rep Cardiol. 2018;2018:6868204. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |