Published online Apr 6, 2022. doi: 10.12998/wjcc.v10.i10.3232
Peer-review started: November 21, 2021
First decision: December 27, 2021
Revised: January 9, 2022
Accepted: February 23, 2022
Article in press: February 23, 2022
Published online: April 6, 2022
IgA nephropathy (IgAN) is a common primary glomerular disease that leads to end-stage renal disease with poor therapy efficacy. Traditional Chinese medicine (TCM) is effective in the treatment of IgAN and has the potential to become an alternative treatment for IgAN. Professor Yan-Qin Zou is a nephropathy expert, a National Chinese Medicine Master, and an heir to the Menghe School of Medicine.
A 28-year-old man had positive urinary protein and elevated serum creatinine (Scr) results and was diagnosed with IgAN 2-3 years prior to the outpatient department visit at our hospital in 2017. Professor Zou used the following methods to treat the patient: Invigorating the spleen and tonifying the kidney, removing dampness and clearing turbidity, quickening the blood and trans
Professor Zou’s therapeutic strategy to treat IgAN using TCM was efficacious and a good reference for application.
Core Tip: IgA nephropathy (IgAN) is a common primary glomerular disease leading to end-stage renal disease with poor prognosis. Traditional Chinese medicine (TCM) is an alternative treatment for IgAN. Professor Yan-Qin Zou, one of the National Chinese Medicine Masters, has accumulated rich and unique experience in TCM diagnosis and treatment of nephropathy. This case report analyses an IgAN patient receiving TCM treatment with satisfying clinical efficacy. Professor Zou’s therapeutic strategy to treat IgAN using TCM was efficacious and a good reference for clinical application.
- Citation: Zhang YY, Chen YL, Yi L, Gao K. IgA nephropathy treatment with traditional Chinese medicine: A case report. World J Clin Cases 2022; 10(10): 3232-3240
- URL: https://www.wjgnet.com/2307-8960/full/v10/i10/3232.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i10.3232
IgA nephropathy (IgAN) is one of the most common forms of primary nephritis and is characterized by mesangial proliferation and diffused IgA deposition in the mesangium[1]. In China, IgAN accounts for 45.26% of primary glomerulonephritis cases[2]. To date, corticosteroids, immunosuppressive agents, and symptomatic treatment have been the main therapeutic strategies, but the long-term treatment efficacy and safety need to be improved[3]. Preserving the renal function remains a major challenge for nephrologists[4]. A new target, sodium-dependent glucose transporters 2 (SGLT2), has reportedly shown efficacy in IgAN, but the high incidence of urinary tract infections has limited the use of SGLT2 inhibitors[5]. Resultingly, increasing attention has been paid to traditional Chinese medicine (TCM).
TCM has a long history in the treatment of kidney diseases in Eastern Asia[6]. Over recent decades, the efficacy and safety of TCM in treating kidney diseases have improved considerably[7,8], as documented studies have confirmed[9,10]. TCM thus has the potential to become an alternative treatment for IgAN[11,12]. However, high quality studies remain scarce. Professor Yan-Qin Zou, a National Chinese Medicine Master and the fourth-generation heir of the Bo-Xiong Fei family, is a well-known nephrology expert in TCM. Professor Zou has been engaged in clinical work for nearly 60 years and has accumulated rich and unique experience in treating nephropathy using TCM methods[13].
Therapies that successfully delay the progression of IgAN remain limited. Once the condition has progressed to renal failure, there are no effective methods to stop the decline of kidney function[14]. This case report describes a patient suffering from renal failure due to IgAN. He received TCM treatment with improvement in renal function, thus demonstrating Professor Zou’s therapeutic strategy for treating IgAN. We hope this report could provide a valuable reference for the treatment of IgAN with TCM.
The patient’s chief complaint was positive urinary protein and elevated serum creatinine (Scr) levels.
A 28-year-old man had positive urinary protein (++) and elevated Scr (149 μmol/L) test results in 2014. He underwent renal biopsy in February 2015 and was diagnosed with “IgAN, mesangial proliferative glomerulonephritis with sclerosis”. Since then, the patient had been taking losartan (100 mg daily) and ketosteril (α-ketoacid tablets; 2.52 g/3 times daily). He first visited the outpatient department at our hospital on June 1, 2017. At this visit, malaise, waist soreness, acid reflux, and bubbles in the urine were the main clinical manifestations. The patient also complained of frequent urination at night. His tongue was light red with a yellow coating, his pulse was slippery (meaning that his pulse was beating freely and smoothly like the movement of abacus beads), and his pharynx was red.
The patient visited the outpatient department again on August 2, 2017. At this visit, waist soreness and fatigue were resolved. The patient’s stomach discomfort was also alleviated. However, he still had a sore throat and spermatorrhea.
At his 3rd visit on September 28, 2017, serological indexes were stable. Clinical manifestations such as waist soreness, fatigue, pharynx discomfort, spermatorrhea, and epigastric discomfort were unchanged.
At the 4th visit on October 26, 2017, serological indexes had decreased significantly. The patient’s epigastric discomfort had improved, but waist soreness remained.
At the patient’s 5th visit on November 23, 2017, his clinical symptoms including waist soreness, fatigue, spermatorrhea, and epigastric discomfort were all resolved, and the serological indexes had also decreased.
The patient has no history of a relevant illness.
The patient has no family history of a similar illness.
On admission, the patient’s blood pressure was 120/80 mmHg, and no abnormalities were detected during the physical examination, including the cardiopulmonary system. There was no edema in either lower limb.
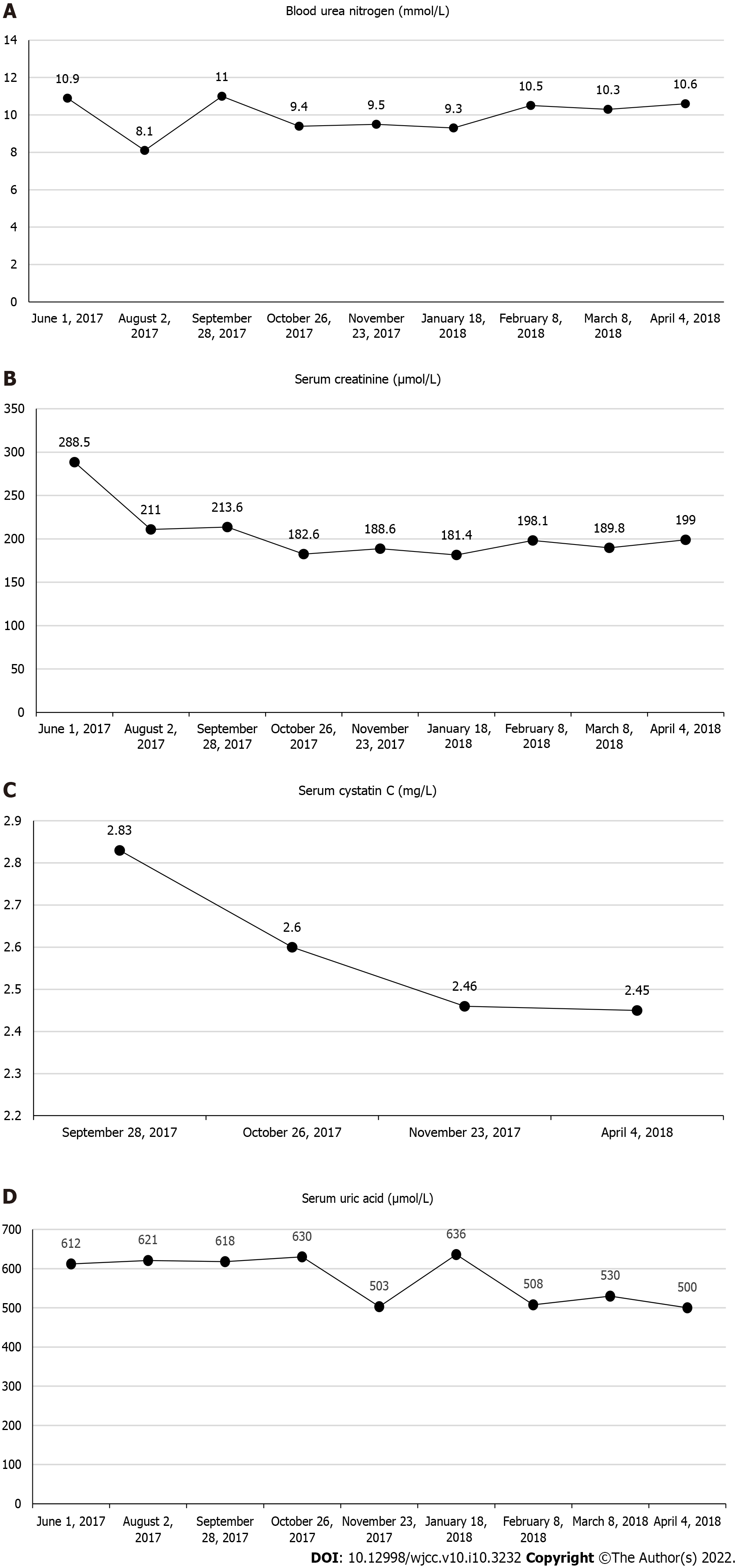
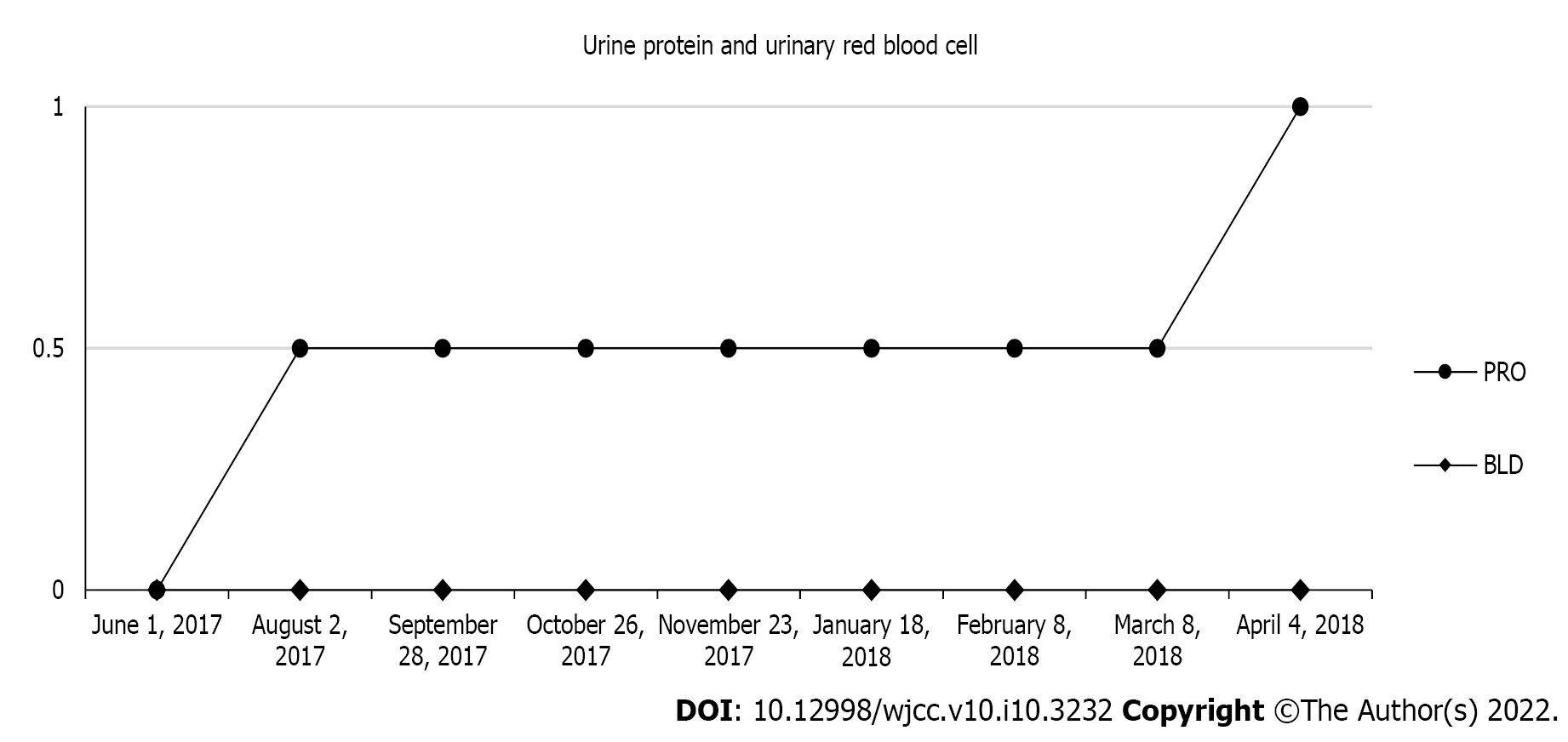
The serological and urinary indexes are shown in Table 1.
| Date | BUN (mmol/L) | Scr (μmol/L) | Cys C (mg/L) | UA (μmol/L) | PRO | BLD |
| June 1, 2017 | 10.9 | 288.5 | - | 612 | (-) | (-) |
| August 2, 2017 | 8.1 | 211 | - | 621 | (±) | (-) |
| September 28, 2017 | 11 | 213.6 | 2.83 | 618 | (±) | (-) |
| October 26, 2017 | 9.4 | 182.6 | 2.6 | 630 | (±) | (-) |
| November 23, 2017 | 9.5 | 188.6 | 2.46 | 503 | (±) | (-) |
| January 18, 2018 | 9.3 | 181.4 | - | 636 | (±) | (-) |
| February 8, 2018 | 10.5 | 198.1 | - | 508 | (±) | (-) |
| March 8, 2018 | 10.3 | 189.8 | - | 530 | (±) | (-) |
| April 4, 2018 | 10.6 | 199 | 2.45 | 500 | (+) | (-) |
Renal ultrasound showed no obvious abnormality.
Under light microscopy, a renal biopsy sample contained 25 glomeruli, among which there were 15 glomeruli with global sclerosis and no crescent. The remaining glomeruli were enlarged with approximately 90-110 cells/glomerulus. There were some mesangial areas with severe matrix hyperplasia with 2-3 cells/mesangium. The basement membrane was normal and the structure of capillary loop remained open. Complete sclerosis was seen in some glomeruli. Masson Stain was negative.
There were moderate lesions in the tubulointerstitium with indistinct tubular structure, no tubular atrophy, some swollen and degenerated tubular epithelial cells and some vacuolar degeneration. Focal fibrosis (40%) and more inflammatory cell infiltration could be seen in the interstitial area.
Immunofluorescence showed classic prominent IgA deposits.
Accordingly, the patient was diagnosed with IgAN (mesangial proliferative glomerulonephritis with sclerosis), Hass Ⅲ[15], M0E0S0T1[16].
The symptoms that were present at the patient’s first visit are described in TCM as kidney and spleen deficiency, dampness, turbidity, blood stasis, and collateral disharmony. After differentiation, Professor Zou initiated TCM therapy, namely by invigorating the spleen and tonifying the kidney, removing dampness and clearing turbidity, quickening the blood and transforming stasis, and freeing vessels and regulating collaterals.
The patient’s TCM prescription included the following: (1) Taizishen (Pseudostellaria heterophylla) 15 g; (2) Shenghuangqi (Radix astragali) 30 g; (3) Chaobaizhu (fried Rhizoma atractylodis macrocephalae) 10 g; (4) Shengyiyiren (Semen coicis) 30 g; (5) Fuling (Poria) 30 g; (6) Fushen (Poria cocos) 30 g; (7) Jiangcan (Bombyx batryticatus) 15 g; (8) Niubangzi (Fructus arctii) 10 g; (9) Huangshukuihua (Abelmoschus manihot) 30 g; (10) Shiwei (Pyrrosia sheareri) 20 g; (11) Chuanduan (Dipsacus asper) 15 g; (12) Sangjisheng (Ramulus taxilli) 15 g; (13) Yinchen (Herba artemisiae scopariae) 30 g; (14) Tufuling (Smilax glabra) 30 g; (15) Shengpuhuang (Pollen typhae) 30 g; (16) Danshen (Radix salviae miltiorrhizae) 20 g; (17) Chishao (Radix paeoniae rubra) 15 g; (18) Honghua (Flos carthaml) 10 g; (19) Wulingzhi (Trogopterus xanthipes) 30 g; (20) Shudahuang (cooked Radix et rhizoma rhei) 12 g; (21) Cheqianzi (Semen plantaginis) 30 g; (22) Donglingcao (Rabdosia rubescens) 10 g; (23) Yumixu (Zea mays) 30 g; (24) Bixie (Dioscoreae hypoglaucae) 20 g; and (25) Walengzi (Arca subcrenata) 40 g. A dose of Chinese medicinal herbs is decocted twice, and the juice is mixed. The herbs were taken twice a day.
At the patient’s 2nd visit, his clinical symptoms were resolved, and the serological indexes were improved. Professor Zou strengthened the therapy of clearing damp-heat and turbidity along with relieving pharynx discomfort and detoxifying in accordance with the abovementioned treatment principles. The patient’s prescription included the prescription from visit 1, but the amount of Tufuling (Smilax glabra) was increased to 50 g, Shudahuang (cooked Radix et rhizoma rhei) was increased to 20 g, and the following were added: (1) Zisuye (Folium perilla leaf) 30 g; (2) Tusizi (Semen cuscutae) 15 g; (3) Xuanshen (Radix scrophulariae) 10 g; (4) Jinyinhua (Flos lonicerae) 10 g; and (5) Baihuasheshecao (Oldenlandia diffusa) 30 g.
At the patient’s 3rd visit, Professor Zou strengthened the therapy of tonifying the kidney while maintaining the power of discharging turbidity and detoxifying. In addition to the initial prescription, Duzhong (Cortex eucommiae) 15 g; Huainiuxi (Radix achyranthis bidentatae) 10 g; Nvzhenzi (Fructus ligustri lucidi) 20 g and Gouqizi (Fructus lycii) 20 g were added to tonify both kidney Yin and kidney Yang. Jixuecao (Centella asiatica) 30 g; Baihuasheshecao (Oldenlandia diffusa) 30 g and Shenggancao (Radix glycyrrhizae) 6 g were added to purge turbidity and aid detoxification, which are effective for reducing creatinine. Jiangcan (Bombyx batryticatus); niubangzi (Fructus arctii); Donglingcao (Rabdosia rubescens); Bixie (Dioscoreae hypoglaucae) and Walengzi (Arca subcrenata) were removed when the abovementioned drugs were added at the third visit. Because Shudahuang (cooked Radix et rhizoma rhei) can also help to quicken the blood, transform stasis, and free the vessels, Chishao (Radix paeoniae rubra) and Honghua (Flos carthaml) were removed because there was enough power to promote blood circulation in the previous treatment.
At the 4th visit, Professor Zou strengthened the therapy to tonify the kidney and clear the pharynx, adding Duanlonggu (Os draconis) 40 g; Duanmuli (Concha ostreae) 40 g; Gouji (Cibotium barometz) 20 g and Tusizi (Semen cuscutae) 15 g to the last prescription.
At the 5th visit, the patient’s clinical symptoms were resolved, and the serological indexes were also decreased. Over the following 5 mo, Professor Zou prescribed the original treatment principles (i.e., Invigorating the spleen and tonifying the kidney, removing dampness and clearing turbidity, quickening the blood and transforming stasis, and freeing vessels and regulating collaterals).
The patient’s symptoms and discomfort were resolved. As shown in Figure 1, during the 1-year follow-up, renal function was improved as evidenced by the stable level of BUN, Scr, serum cystatin C and UA. As shown in Figure 2, urinary red blood cell remained negative, and urinary protein maintained negative or trace findings.
A typical clinical manifestation of IgAN is hematuria with or without proteinuria, hypertension, and impaired renal function[1]. Some patients with IgAN gradually progress to chronic renal failure 10-20 years after their diagnosis[17]. The efficacy of conventional therapy is limited because of side effects. Treatment using TCM is worth considering because it has shown good safety and therapeutic effects.
IgAN is in the edema and hematuria category in TCM[18]. In ancient times, doctors had a comprehensive theory on pathogenesis, diagnosis, and therapy for kidney diseases, as recorded in the Yellow Emperor’s Canon of Medicine Plain Conversation: “All dampness, swelling and turgidity is ascribed to the spleen.” Professor Zou proposes that IgAN pathogenesis is a mixture of deficiency and excess. Patients with IgAN are susceptible to outer pathogen infection because of lung Qi deficiency, in accordance with TCM theory. Qi deficiency in the kidney, spleen, and lung is the internal basis that contributes to damp-heat production as a pathological factor throughout the course of IgAN. Additionally, the long-term existence of the dampness pathogen suppresses Qi and leads to Qi stagnation. Qi stagnation makes it difficult for blood to circulate smoothly. In summary, the main cause of IgAN is derived from kidney, spleen and lung deficiency, which is accompanied by dampness, damp-heat, blood stasis and wind-pathogen. Improving deficiency and eliminating excess pathogenic factors constituted Professor Zou’s main clinical therapeutic strategy.
In this case, Professor Zou initially distinguished between deficiency syndrome and excess syndrome, giving consideration to both improving the deficiency and expelling pathogenic factors. The patient was treated on the basis of the disease stage and its course. In the early stage of therapy, pathogenic factors were prominent. Professor Zou strengthened the therapy of purging turbidity and detoxifying to gradually eliminate the damp-heat and blood stasis from the body. Malaise and waist soreness in the morning indicated kidney and spleen deficiency, while acid reflux, increased Scr and UA levels and bubbles in the urine demonstrated turbidity and dampness. She used treatment measures to tonify the kidney and spleen, purge turbidity and clear dampness, promote blood circulation and remove blood stasis. After the first treatment, the waist and stomach symptoms were relieved and serology indexes were improved. However, the patient’s throat discomfort and an increase in spermatorrhea demonstrated persisting kidney deficiency. At the following visits, the deficiency syndrome was the main target. Professor Zou strengthened the therapy of invigorating the kidney, spleen and lung to improve Qi. Throughout the disease treatment, Professor Zou focused on tonifying the kidney and spleen and clearing away damp-heat. After almost 6 mo of treatment, the patient’s symptoms were resolved, and Scr and UA levels were significantly lower. There was an increase in the UA level on January 18, 2018, which may have resulted from the previous cold or the patient’s overeating. These were not recorded and overall, the UA level trended downwards. Over the subsequent follow-up, renal function remained stable.
For herb selection, Professor Zou prefers mild and gentle herbs to invigorate the kidney and spleen because warm and hot drugs can easily hurt Yin, and greasy drugs can easily cause dampness stagnation. She uses drugs such as: (1) Taizishen (Pseudostellaria heterophylla); (2) Shenghuangqi (Radix astragali); (3) Chaobaizhu (fried Rhizoma atractylodis macrocephalae); (4) Shengyiyiren (Semen coicis), (5) Fuling (Poria); and (6) Fushen (Poria cocos). Furthermore, the mechanism of kidney diseases in TCM theory is the disorder of Yin and Yang in the lower abdomen (Xia-jiao), and it is difficult for the herbs to reach the disease center because Xia-jiao is located in the lower part of the body[19]. However, the course of kidney disease is often long and persistent. Professor Zou used a combination of herbs and larger drug doses to balance Yin and Yang in the lower abdomen. The following herbs are often used for purging turbidity and detoxifying: (1) Huangshukuihua (Abelmoschus manihot); (2) Shiwei (Pyrrosia sheareri); (3) Yinchen (Herba artemisiae scopariae); (4) Tufuling (Smilax glabra); (5) Shudahuang (cooked Radix et rhizoma rhei); (6) Cheqianzi (Semen plantaginis); (6) Donglingcao (Rabdosia rubescens); (7) Yumixu (Zea mays); (8) Bixie (Dioscoreae hypoglaucae); (9) Baihuasheshecao (Oldenlandia diffusa); (10) Xuanshen (Radix scrophulariae); and (11) Jinyinhua (Flos lonicerae). For proteinuria, drugs such as: (1) Jiangcan (Bombyx batryticatus); (2) Niubangzi (Fructus arctii); and (3) Huangshukuihua (Abelmoschus manihot) are commonly used[20-22]. Modern pharmacological research suggests that the major effects of herbal medicine are related to anti-inflammatory, antioxidative, antifibrotic and immunomodulatory pathways[6,12,23].
Most TCM practitioners consider that Qi and Yin deficiencies are the leading causes of IgAN and propose that the treatment of IgAN should be based on reinforcing Qi and replenishing Yin[24]. In contrast to the general TCM treatment, Professor Zou suggests that kidney deficiency is the most fundamental internal factor in the occurrence of IgAN and the treatment of IgAN should be based on tonifying the kidney and harmonizing other viscera. In addition, the spleen also plays an important role in the pathogenesis of IgAN. In TCM theory, the spleen governs the transportation and transformation of nutrients and water and it controls the function of spleen-qi to elevate food nutrients[17]. Tonifying the spleen is conducive to controlling proteinuria and improving metabolism. Recently, some powerful drugs, such as Leigongteng (Tripterygium wilfordii), have been proven to be protective against kidney diseases[25]. However, although these powerful drugs may have obvious short-term effects, they may easily hurt healthy Qi. Professor Zou advocates mild drugs to gradually dissipate the pathogenic factors without side effects. Unique academic thought and exquisite herbal selection reflect the power of Professor Zou as a National Chinese Medicine Master.
Herein, we report only one case, which has limited reference value to reflect Professor Zou’s treatment experience. However, we followed the patient for nearly 1 year and did not observe any subsequent disease relapse. Finally, 24-hour urine protein quantification is also an important laboratory indicator for IgAN, but we did not have access to these results because the patient did not undergo this test in the outpatient setting.
IgAN is a prevalent type of glomerular disease in most Western and Asian countries. TCM therapy uses natural medicines that can reduce proteinuria and Scr and improve symptoms such as back pain in a long-term regimen. Professor Zou is a TCM specialist in treatment of IgAN. Her main therapeutic strategies for treating this disease focus on improving deficiency and eliminating excess pathogenic factors. This case provides a specific method and an effective reference for clinical application of TCM to treat IgAN. Our findings indicate that TCM can play an important role in the treatment of IgAN and is worth consideration as a worldwide treatment option.
We thank Li W for editing the English text of a draft of this manuscript and Sun PC for helping to revise the manuscript.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cabezuelo AS, Yorioka N S-Editor: Guo XR L-Editor: Filipodia P-Editor: Guo XR
| 1. | Rodrigues JC, Haas M, Reich HN. IgA Nephropathy. Clin J Am Soc Nephrol. 2017;12:677-686. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 283] [Cited by in F6Publishing: 297] [Article Influence: 42.4] [Reference Citation Analysis (0)] |
| 2. | Li LS, Liu ZH. Epidemiologic data of renal diseases from a single unit in China: analysis based on 13,519 renal biopsies. Kidney Int. 2004;66:920-923. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 277] [Cited by in F6Publishing: 298] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 3. | Feehally J, Floege J, Tonelli M, Richard J Johnson. Comprehensive Clinical Nephrology. 6th ed. Edinburgh: Elsevier, 2019: 270. [Cited in This Article: ] |
| 4. | Nagy J, Sági B, Máté J, Vas T, Kovács T. [Considerations on the treatment of IgA nephropathy on the basis of the results of the latest studies (STOP-IgAN, TESTING, NEFIGAN)]. Orv Hetil. 2017;158:1946-1952. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, Mann JFE, McMurray JJV, Lindberg M, Rossing P, Sjöström CD, Toto RD, Langkilde AM, Wheeler DC; DAPA-CKD Trial Committees and Investigators. Dapagliflozin in Patients with Chronic Kidney Disease. N Engl J Med. 2020;383:1436-1446. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1586] [Cited by in F6Publishing: 2170] [Article Influence: 542.5] [Reference Citation Analysis (1)] |
| 6. | Li X, Wang H. Chinese herbal medicine in the treatment of chronic kidney disease. Adv Chronic Kidney Dis. 2005;12:276-281. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 65] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Zhong Y, Menon MC, Deng Y, Chen Y, He JC. Recent Advances in Traditional Chinese Medicine for Kidney Disease. Am J Kidney Dis. 2015;66:513-522. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 88] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 8. | Peng A, Gu Y, Lin SY. Herbal treatment for renal diseases. Ann Acad Med Singap. 2005;34:44-51. [PubMed] [Cited in This Article: ] |
| 9. | Zhang L, Li P, Xing CY, Zhao JY, He YN, Wang JQ, Wu XF, Liu ZS, Zhang AP, Lin HL, Ding XQ, Yin AP, Yuan FH, Fu P, Hao L, Miao LN, Xie RJ, Wang R, Zhou CH, Guan GJ, Hu Z, Lin S, Chang M, Zhang M, He LQ, Mei CL, Wang L, Chen X. Efficacy and safety of Abelmoschus manihot for primary glomerular disease: a prospective, multicenter randomized controlled clinical trial. Am J Kidney Dis. 2014;64:57-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 10. | Li W, He W, Xia P, Sun W, Shi M, Zhou Y, Zhu W, Zhang L, Liu B, Zhu J, Zhu Y, Zhou E, Sun M, Gao K. Total Extracts of Abelmoschus manihot L. Attenuates Adriamycin-Induced Renal Tubule Injury via Suppression of ROS-ERK1/2-Mediated NLRP3 Inflammasome Activation. Front Pharmacol. 2019;10:567. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Lu WI, Lu DP. Impact of chinese herbal medicine on american society and health care system: perspective and concern. Evid Based Complement Alternat Med. 2014;2014:251891. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Wojcikowski K, Johnson DW, Gobe G. Herbs or natural substances as complementary therapies for chronic kidney disease: ideas for future studies. J Lab Clin Med. 2006;147:160-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Yi L, Zhou EC, Gao K, Zhong Y, Li HW. Traditional Chinese Medicine Master Zou Yanqin’s Experience on Treating Chronic Kidney Disease with the Academic Thought of “Harmonizing and Mild Therapeutic Method”. Nanjing Zhongyiyao Daxue Xuebao. 2020;36:552-556. [Cited in This Article: ] |
| 14. | Ammirati AL. Chronic Kidney Disease. Rev Assoc Med Bras (1992). 2020;66 Suppl 1:s03-s09. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 103] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 15. | Haas M. Histologic subclassification of IgA nephropathy: a clinicopathologic study of 244 cases. Am J Kidney Dis. 1997;29:829-842. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 327] [Cited by in F6Publishing: 292] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 16. | Working Group of the International IgA Nephropathy Network and the Renal Pathology Society; Cattran DC, Coppo R, Cook HT, Feehally J, Roberts IS, Troyanov S, Alpers CE, Amore A, Barratt J, Berthoux F, Bonsib S, Bruijn JA, D'Agati V, D'Amico G, Emancipator S, Emma F, Ferrario F, Fervenza FC, Florquin S, Fogo A, Geddes CC, Groene HJ, Haas M, Herzenberg AM, Hill PA, Hogg RJ, Hsu SI, Jennette JC, Joh K, Julian BA, Kawamura T, Lai FM, Leung CB, Li LS, Li PK, Liu ZH, Mackinnon B, Mezzano S, Schena FP, Tomino Y, Walker PD, Wang H, Weening JJ, Yoshikawa N, Zhang H. The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int. 2009;76:534-545. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 786] [Cited by in F6Publishing: 839] [Article Influence: 55.9] [Reference Citation Analysis (0)] |
| 17. | Wang HY. Nephrology. 3rd ed. Beijing: People’s Health Publishing House, 2008: 993, 1001. [Cited in This Article: ] |
| 18. | Zuo YF. A Newly Compiled Practical English-Chinese Library of Traditional Chinese Medicine Internal Medicine of Traditional Medicine. 1st ed. Shanghai: Publishing House of Shanghai University of Traditional Chinese Medicine, 2002: 260. [Cited in This Article: ] |
| 19. | Zuo YF. A Newly Compiled Practical English-Chinese Library of Traditional Chinese Medicine Basic Theory of Traditional Medicine. 1st ed. Shanghai: Publishing House of Shanghai University of Traditional Chinese Medicine, 2002: 62-63, 81-82. [Cited in This Article: ] |
| 20. | Hu M, Yu Z, Wang J, Fan W, Liu Y, Li J, Xiao H, Li Y, Peng W, Wu C. Traditional Uses, Origins, Chemistry and Pharmacology of Bombyx batryticatus: A Review. Molecules. 2017;22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Gao Q, Yang M, Zuo Z. Overview of the anti-inflammatory effects, pharmacokinetic properties and clinical efficacies of arctigenin and arctiin from Arctium lappa L. Acta Pharmacol Sin. 2018;39:787-801. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 108] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 22. | Li N, Tang H, Wu L, Ge H, Wang Y, Yu H, Zhang X, Ma J, Gu HF. Chemical constituents, clinical efficacy and molecular mechanisms of the ethanol extract of Abelmoschus manihot flowers in treatment of kidney diseases. Phytother Res. 2021;35:198-206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 23. | Tapsell LC, Hemphill I, Cobiac L, Patch CS, Sullivan DR, Fenech M, Roodenrys S, Keogh JB, Clifton PM, Williams PG, Fazio VA, Inge KE. Health benefits of herbs and spices: the past, the present, the future. Med J Aust. 2006;185:S1-S24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 272] [Cited by in F6Publishing: 265] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 24. | Wang XH, Lang R, Liang Y, Zeng Q, Chen N, Yu RH. Traditional Chinese Medicine in Treating IgA Nephropathy: From Basic Science to Clinical Research. J Transl Int Med. 2021;9:161-167. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 25. | Zhong Y, Deng Y, Chen Y, Chuang PY, Cijiang He J. Therapeutic use of traditional Chinese herbal medications for chronic kidney diseases. Kidney Int. 2013;84:1108-1118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 114] [Article Influence: 10.4] [Reference Citation Analysis (0)] |