Abstract
Background
Grade 3 (G3) gastroenteropancreatic (GEP) neuroendocrine neoplasms (NENs) are rare, aggressive tumors with poor prognosis. The World Health Organization 2017 and 2019 classifications further subdivided G3 NENs into G3 neuroendocrine tumors (NETs) and neuroendocrine carcinomas (NECs). Current guidelines favor medical management in most of these patients, and the role of surgical management is not well defined. We performed a systematic literature review and meta-analysis of surgical management versus nonsurgical management for G3 GEP NENs.
Materials and Methods
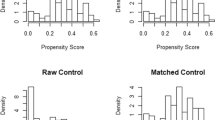
A PRISMA-compliant systematic review of the MEDLINE, Embase, Scopus, and Cochrane Library databases (end-of-search date: 16 July 2021) was conducted. Individual patient survival data were reconstructed, and random-effects meta-analyses were performed.
Results
Fourteen studies comprising 1810 surgical and 910 nonsurgical patients were systematically reviewed. Publication bias adjusted meta-analysis of 12 studies (1788 surgical and 857 nonsurgical patients) showed increased overall survival (OS) after surgical compared with nonsurgical management for G3 GEP NENs [hazard ratio (HR) 0.40, 95% confidence interval (CI) 0.31–0.53]. Subgroup meta-analyses showed increased OS after surgical management for both pancreatic and gastrointestinal primary sites separately. In another subgroup meta-analysis of G3 GEP NETs (not NECs), surgical management was associated with increased OS compared with nonsurgical management (HR 0.26, 95% CI 0.11–0.61).
Conclusions
Surgical management of G3 GEP NENs may provide a potential survival benefit in well-selected cases. Further research is needed to define which patients will benefit most from surgical versus nonsurgical management. The current literature is limited by inconsistent reporting of survival outcomes in surgical versus nonsurgical groups, tumor grade, differentiation, primary tumor site, and selection criteria for surgical and nonsurgical management.





Similar content being viewed by others
References
Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335–42. https://doi.org/10.1001/jamaoncol.2017.0589.
Pavel M, Öberg K, Falconi M, et al. Gastroenteropancreatic neuroendocrine neoplasms: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31(7):844–60. https://doi.org/10.1016/j.annonc.2020.03.304.
Klimstra DS, Modlin IR, Coppola D, Lloyd RV, Suster S. The pathologic classification of neuroendocrine tumors: a review of nomenclature, grading, and staging systems. Pancreas. 2010;39(6):707–12. https://doi.org/10.1097/MPA.0b013e3181ec124e.
Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO Classification of Tumours of the Digestive System. World Health Organization; 2010.
Sorbye H, Baudin E, Perren A. The problem of high-grade gastroenteropancreatic neuroendocrine neoplasms: well-differentiated neuroendocrine tumors, neuroendocrine carcinomas, and beyond. Endocrinol Metab Clin North Am. 2018;47(3):683–98. https://doi.org/10.1016/j.ecl.2018.05.001.
Sorbye H, Welin S, Janson ET, et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol. 2013;24(1):152–60. https://doi.org/10.1093/annonc/mds276.
Basturk O, Tang L, Hruban RH, et al. Poorly differentiated neuroendocrine carcinomas of the pancreas: a clinicopathologic analysis of 44 cases. Am J Surg Pathol. 2014;38(4):437–47. https://doi.org/10.1097/PAS.0000000000000169.
Choe J, Kim KW, Kim HJ, et al. What is new in the 2017 World Health Organization Classification and 8th American Joint Committee on cancer staging system for pancreatic neuroendocrine neoplasms? Korean J Radiol. 2019;20(1):5–17. https://doi.org/10.3348/kjr.2018.0040.
Nagtegaal ID, Odze RD, Klimstra D, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76(2):182–8. https://doi.org/10.1111/his.13975.
Garcia-Carbonero R, Sorbye H, Baudin E, et al. ENETS consensus guidelines for high-grade gastroenteropancreatic neuroendocrine tumors and neuroendocrine carcinomas. Neuroendocrinology. 2016;103(2):186–94. https://doi.org/10.1159/000443172.
Howe JR, Merchant NB, Conrad C, et al. The North American neuroendocrine tumor society consensus paper on the surgical management of pancreatic neuroendocrine tumors. Pancreas. 2020;49(1):1–33. https://doi.org/10.1097/MPA.0000000000001454.
Howe JR, Cardona K, Fraker DL, et al. The surgical management of small bowel neuroendocrine tumors: consensus guidelines of the North American neuroendocrine tumor society. Pancreas. 2017;46(6):715–31. https://doi.org/10.1097/MPA.0000000000000846.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Borbon LC, Tran CG, Sherman SK, et al. Is there a role for surgical resection of grade 3 neuroendocrine neoplasms? Ann Surg Oncol. 2022. https://doi.org/10.1245/s10434-022-12100-3.
Guyot P, Ades AE, Ouwens MJNM, Welton NJ. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 2012;12:9. https://doi.org/10.1186/1471-2288-12-9.
Wei Y, Royston P. Reconstructing time-to-event data from published Kaplan-Meier curves. Stata J. 2017;17(4):786–802.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. https://doi.org/10.1186/1745-6215-8-16.
Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ. 2010;340:c221. https://doi.org/10.1136/bmj.c221.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63. https://doi.org/10.1111/j.0006-341x.2000.00455.x.
Shi L, Lin L. The trim-and-fill method for publication bias: practical guidelines and recommendations based on a large database of meta-analyses. Medicine (Baltimore). 2019;98(23):e15987. https://doi.org/10.1097/MD.0000000000015987.
Thornblade LW, Warner SG, Melstrom L, et al. Does surgery provide a survival advantage in non-disseminated poorly differentiated gastroenteropancreatic neuroendocrine neoplasms? Surgery. 2021;169(6):1417–23. https://doi.org/10.1016/j.surg.2021.01.026.
Haugvik S-P, Janson ET, Österlund P, et al. Surgical treatment as a principle for patients with high-grade pancreatic neuroendocrine carcinoma: a Nordic multicenter comparative study. Ann Surg Oncol. 2016;23(5):1721–8. https://doi.org/10.1245/s10434-015-5013-2.
Du S, Wang Z, Sang X, et al. Surgical resection improves the outcome of the patients with neuroendocrine tumor liver metastases: large data from Asia. Medicine (Baltimore). 2015;94(2):e388. https://doi.org/10.1097/MD.0000000000000388.
Fang C, Wang W, Zhou Z, et al. Clinicopathologic characteristics and prognosis of gastroenteropancreatic neuroendocrine neoplasms: a multicenter study in South China. Chin J Cancer. 2017;36(1):51. https://doi.org/10.1186/s40880-017-0218-3.
Li MX, Li QY, Xiao M, et al. Survival comparison between primary hepatic neuroendocrine neoplasms and primary pancreatic neuroendocrine neoplasms and the analysis on prognosis-related factors. Hepatobiliary Pancreat Dis Int. 2019;18(6):538–45. https://doi.org/10.1016/j.hbpd.2019.03.009.
Schurr PG, Strate T, Rese K, et al. Aggressive surgery improves long-term survival in neuroendocrine pancreatic tumors: an institutional experience. Ann Surg. 2007;245(2):273–81. https://doi.org/10.1097/01.sla.0000232556.24258.68.
Fischer L, Kleeff J, Esposito I, et al. Clinical outcome and long-term survival in 118 consecutive patients with neuroendocrine tumours of the pancreas. Br J Surg. 2008;95(5):627–35. https://doi.org/10.1002/bjs.6051.
Busico A, Maisonneuve P, Prinzi N, et al. Gastroenteropancreatic high-grade neuroendocrine neoplasms: histology and molecular analysis, two sides of the same coin. Neuroendocrinology. 2020;110(7–8):616–29. https://doi.org/10.1159/000503722.
Crippa S, Partelli S, Bassi C, et al. Long-term outcomes and prognostic factors in neuroendocrine carcinomas of the pancreas: morphology matters. Surgery. 2016;159(3):862–71. https://doi.org/10.1016/j.surg.2015.09.012.
Asano D, Kudo A, Akahoshi K, et al. Curative surgery and Ki-67 value rather than tumor differentiation predict the survival of patients with high-grade neuroendocrine neoplasms. Ann Surg. 2020. https://doi.org/10.1097/sla.0000000000004495.
Yoshida T, Hijioka S, Hosoda W, et al. Surgery for pancreatic neuroendocrine tumor g3 and carcinoma G3 should be considered separately. Ann Surg Oncol. 2019;26(5):1385–93. https://doi.org/10.1245/s10434-019-07252-8.
Chen Y, Yang M, Wang W, Huang M, Wang L, Tian B. Long-term outcomes of World Health Organization G3 pancreatic neuroendocrine neoplasms: a retrospective study in combination of morphological and proliferative analysis. Int J Clin Exp Pathol. 2017;10(6):6385–94.
Wang Z-J, An K, Li R, et al. Analysis of 72 patients with colorectal high-grade neuroendocrine neoplasms from three Chinese hospitals. World J Gastroenterol. 2019;25(34):5197–209. https://doi.org/10.3748/wjg.v25.i34.5197.
Pommergaard H-C, Nielsen K, Sorbye H, et al. Surgery of the primary tumour in 201 patients with high-grade gastroenteropancreatic neuroendocrine and mixed neuroendocrine-non-neuroendocrine neoplasms. J Neuroendocrinol. 2021;33(5):e12967. https://doi.org/10.1111/jne.12967.
Yachida S, Vakiani E, White CM, et al. Small cell and large cell neuroendocrine carcinomas of the pancreas are genetically similar and distinct from well-differentiated pancreatic neuroendocrine tumors. Am J Surg Pathol. 2012;36(2):173–84. https://doi.org/10.1097/PAS.0b013e3182417d36.
Genc CG, Klümpen HJ, van Oijen MGH, van Eijck CHJ, Nieveen van Dijkum EJM. A nationwide population-based study on the survival of patients with pancreatic neuroendocrine tumors in the Netherlands. World J Surg. 2018;42(2):490–7. https://doi.org/10.1007/s00268-017-4278-y.
Acknowledgement
None.
Funding
Several authors (P.J.B., C.C., J.S.D., A.M.B., and J.R.H.) were supported by the Iowa SPORE for Neuroendocrine Tumors (P50 CA174521-01).
Author information
Authors and Affiliations
Contributions
IAZ: study design, literature search and study selection, data extraction, analysis and interpretation of data, drafting of the manuscript. PTT: literature search and study selection, data extraction, analysis and interpretation of data, critical revision of the manuscript. LCB: data extraction, analysis and interpretation of data, critical revision of the manuscript. SKS: analysis and interpretation of data, critical revision of the manuscript. PJB: analysis and interpretation of data, critical revision of the manuscript. Chandrikha Chandrasekharan: analysis and interpretation of data, critical revision of the manuscript. JSD: analysis and interpretation of data, critical revision of the manuscript. AMB: analysis and interpretation of data, critical revision of the manuscript. JRH: study design, literature search and study selection, analysis and interpretation of data, drafting of the manuscript.
Corresponding author
Ethics declarations
Dislcosure
The author declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ziogas, I.A., Tasoudis, P.T., Borbon, L.C. et al. Surgical Management of G3 Gastroenteropancreatic Neuroendocrine Neoplasms: A Systematic Review and Meta-analysis. Ann Surg Oncol 30, 148–160 (2023). https://doi.org/10.1245/s10434-022-12643-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12643-5