Abstract
Background
Little is known about the surgical patterns of American Indian/Alaska Native (AI/AN) breast cancer patients. The purpose of this study is to determine whether there are disparities in breast cancer surgery and radiation therapy between non-Hispanic AI/AN (NH-AI/AN) women and non-Hispanic White (NHW) women.
Methods
Data from the National Program of Cancer Registries of the Centers for Disease Control and Surveillance, Epidemiology, and End Results were used for this cross-sectional study. Female patients with invasive breast cancer diagnosed 2010–2015 were stratified by race/ethnicity, surgical procedure, radiation, and region. Percentage distributions of mastectomy and lumpectomy were compared overall and by region and stage.
Results
From 2010 to 2015 there were 3292 NH-AI/AN women and 165,225 NHW women diagnosed with breast cancer. For early stage (AJCC stage 1 and 2), NH-AI/AN women had overall significantly higher percentage of mastectomy (41% vs 34.4%, p < 0.001) and significantly lower percentage of lumpectomy (59% vs 65.6%) compared with NHW women, without significant differences in post-lumpectomy radiation (71% vs 70%). There were regional variations, notably in the Northern Plains, where the percentage of mastectomy for early-stage disease was 48.9% for NH-AI/AN women versus 35.9% for NHW women, and in Alaska with 47% for NH-AI/AN women versus 33.3% for NHW women (p < 0.001). There were no overall significant differences in type of surgery or radiation for late-stage disease between groups.
Conclusion
This is the first study to show disparities in surgical management of NH-AI/AN women with breast cancer. For early-stage disease, NH-AI/AN women undergo a higher percentage of mastectomy. Future clinical directions could focus on the factors that drive awareness, decision-making, and access to breast conservation.
Similar content being viewed by others
AI/AN women currently have the worst breast cancer survival outcomes amongst any racial group in the USA.1,2,3,4,5 Randomized trials with long-term follow-up have demonstrated that although recurrence is higher after lumpectomy alone, the survival is equivalent for patients treated with mastectomy or breast-conserving therapy (BCT), which consists of lumpectomy followed by radiation.6,7,8,9,10 This has established a surgical choice for women, but disparities persist in surgical procedures performed for different groups, even after controlling for stage of disease.11 BCT has been consistently found to have decreased complications and pain and better recovery and quality of life.12,13,14,15,16 There is evidence that women from racial minority groups have lower rates of BCT, breast reconstruction, and contralateral prophylactic mastectomy.11,17,18,19,20 While data exist for other groups, surgical patterns for AI/AN women have not been examined.
The purpose of this study is to provide a descriptive overview of surgical disparities between AI/AN and White women by US geographic region. Therefore, we evaluated the difference in distribution of surgical procedure (mastectomy and lumpectomy), as well as BCT (lumpectomy plus radiation) between the two populations by region and patient characteristics utilizing cancer registry data that has been linked with the Indian Health Service (IHS) patient registration database for the purposes of reducing racial misclassification in AI/AN populations.21,22
Methods
We utilized data from population-based central cancer registries participating in the National Program of Cancer Registries of the Centers for Disease Control and Prevention (CDC) and Surveillance, Epidemiology, and End Results (SEER) program of the National Cancer Institute (NCI).23,24 Because the study did not involve human participants, institutional review board approval was not necessary.
Women diagnosed with primary invasive breast cancer defined by World Health Organization (WHO) International Classification of Diseases for Oncology, 3rd edition [ICD-O-3: C50.0-C50.9 excluding lymphomas, leukemia, and Kaposi sarcomas (9050-9055, 9140, 9590-9992)] from 2010 to 2015 were included.25 AJCC staging information was available only during these diagnosis years.26 Cases reported through autopsy or death certificate only, those with unknown or missing surgical status, or where radiation treatment information was not available in the database (Connecticut, Hawaii, Iowa, and New Mexico) were excluded (total AI/AN N = 619). Cancer cases in this study period have met the standard for high-quality data according to the United States Cancer Statistics.27
Efforts to reduce racial misclassification of the AI/AN population in cancer databases have been described elsewhere.21 Briefly, all cases from each registry were linked with the IHS patient registration database to identify AI/AN cases with race misclassified as non-AI/AN. These linkages were conducted using LinkPlus, a probabilistic software program developed by the CDC that utilizes key patient identifiers (social security number, first name, last name, date of birth, etc.).28 In an effort to further improve race classification, this study focuses on IHS Purchased/Referred Care Delivery Area (PRCDA) counties.21,22 These counties contain or are located adjacent to federally recognized lands where AI/AN women are more likely to access IHS services. Linkages in these areas provide more accurate correction for AI/AN racial misclassification for a portion of the AI/AN population (Fig. 1). During previous analyses, it was discovered that updated bridged intercensal population estimates substantially overestimated AI/AN populations of Hispanic origin.29 To avoid underestimating incidence in AI/AN populations, we limited analyses to non-Hispanic AI/AN populations. The non-Hispanic White population was chosen as the referent. For conciseness, hereafter, non-Hispanic AI/AN is abbreviated as NH-AI/AN, and non-Hispanic White as NHW in reference to the study data.
Geographic regions and purchased/referred care delivery areaa counties by region. aCounties that contain federally recognized tribal lands or are adjacent to tribal lands. Race classification for the AI/AN population is more accurate in these counties. Percent regional coverage of AI/AN in PRCDA counties to AI/AN in all counties: northern plains 54.2%; Alaska 100%; southern plains 56.5%; southwest 83.8%; Pacific coast 60.2%; East 16.4; Total US 53.0%
Stage at diagnosis, using AJCC 7th edition was categorized into five groups: stage I, II, III, and IV and unknown stage.26 For this analysis, stage was further categorized into early (AJCC stage I and II) versus late (AJCC stage III, IV) because these groupings are clinically relevant for management and prognosis. Tumor subtype was classified based on estrogen receptor (ER) and progesterone receptor (PR) status. ER and PR status were combined into one of three categories (combination of collaborative stage (CS) site-specific factor 1 and CS site-specific factor 2): hormone positive (cases with ER+ or PR+ or borderline ER or PR), hormone negative (ER—and PR—cases), and unknown hormone receptor status. Unknown status included ER− cases where PR test results were unknown/missing, PR− cases where ER test results were unknown/missing, and cases where both ER and PR test results were unknown or missing. Human epidermal growth factor/neu receptor (HER2) data were not sufficient for evaluation. Tumor size was categorized as < 2 cm, 2 to < 5 cm, and > 5 cm according to the “CS Tumor Size” variable. Lymph node status was categorized as positive, negative, or unknown based on the combination of “CS Lymph Codes” or “Regional Lymph Nodes Examined.” Surgical treatment was categorized based on SEER surgery codes, RX Summ Surgery Primary Sites.
Statistical Analysis
Average annual age-adjusted incidence rates were calculated using the direct method.30 Rates are expressed per 100,000 and adjusted by 19 age groups to the 2000 US standard population (Census P25-1130).31 Rate ratios (RR) with 95% confidence intervals (CI) were calculated for comparison of incidence rates between NH-AI/AN and NHW populations, overall and regional, according to methods described by Tiwari et al. using SEER*Stat software 8.3.2.32,33 Denominators for rate calculations were derived from population estimates from the US Bureau of the Census. Data were suppressed when fewer than six cases were reported. SEER*Stat was used to calculate frequencies and percentage distributions of patient characteristics including age (< 50 years, 50–69 years, 70+ years), stage, operation, radiation, lymph node status, ER/PR status, and tumor size, between NH-AI/AN and NHW populations by regions. Tests for statistical significance (chi-squared) were calculated using SAS version 9.4. Long-term trends in mastectomy by race for the years 2005–2015 were estimated by joinpoint regression with software developed by the NCI (Joinpoint Regression Program, version 4.7.0).34
Results
From 2010 to 2015 there were a total of 3292 NH-AI/AN women and 165,225 NHW women diagnosed with breast cancer (Table 1). The majority who underwent lumpectomy had early-stage disease (94% NH-AI/AN women, 95.7% NHW women). There were near-equal distributions of postlumpectomy radiation (68.9% NH-AI/AN women, 68.3% NHW women). Supplementary Table 1 presents more detailed characteristics by surgery status.
Breast cancer incidence rates by region and stage are described in Table 2. NH-AI/AN women had a statistically significant lower incidence of breast cancer compared with NHW women, all stages and all regions combined (RR 0.90, 95% CI 0.87–0.93). Incidence rates varied by region, with NH-AI/AN women from Alaska (RR 1.33, CI 1.18–1.50) and Southern Plains (RR 1.28, CI 1.20–1.38) having significantly higher incidence, while NH-AI/AN women from the Pacific Coast (RR 0.89, CI 0.83–0.96), East (RR 0.63, CI 0.54–0.67), and Southwest (RR 0.57, CI 0.51–0.62) had significantly lower incidence. For early-stage disease, incidence was significantly lower for NH-AI/AN women compared with NHW women, all regions combined (RR 0.86, CI 0.83–0.90). Incidence of late-stage disease was higher for NH-AI/AN women, all regions combined (RR 1.08, CI 1.01–1.17).
Distribution of surgical treatment by stage, region, and race is presented in Table 3. For early-stage breast cancer, a significantly higher percentage of NH-AI/AN women were treated with mastectomy (41% versus 34.4%, p < 0.001). For late-stage breast cancer, there was no significant differences in type of surgery performed. In the Northern Plains, 48.9% of NH-AI/AN women underwent mastectomy for early-stage disease, compared with 35.9% for NHW women (p < 0.001) (Table 3). In Alaska, the percentages were 47% for NH-AI/AN women versus 33.3%% for NHW women (p < 0.001). There were no significant differences in distribution of early-stage mastectomy in the remaining regions.
For those undergoing lumpectomy with complete treatment information, distribution of radiation was also calculated to assess differences in BCT (Table 3). There were no overall differences in postlumpectomy radiation between groups for early- or late-stage disease. Regional analysis showed that in the Northern Plains (84.3% versus 77.5%, p = 0.04), Alaska (71.4% versus 59.9%, p = 0.03), and Southwest (55.4% versus 43.6%, p = 0.004), a higher percentage of NH-AI/AN women with early-stage breast cancers received postlumpectomy radiation.
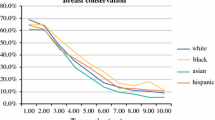
The percentage of NH-AI/AN women who underwent mastectomy was stable 2005–2015 (Fig. 2A). For NHW women, the mastectomy trend increased significantly from 2005 to 2010 (APC 1.8), then decreased significantly from 2010 to 2015 (APC—3.0). The APC for mastectomy varied by disease stage and time frame (Fig. 2B). For early-stage disease, the APC decreased for NH-AI/AN women (1.3) during the time period, but increased (2005–2010), plateaued (2010–2014), then decreased (2014–2015) for NHW women. For late-stage disease, the APC for mastectomy remained level for NH-AI/AN women but increased (2005–2013) before decreasing (2013–2015) for NHW women.
Trends in mastectomya, by race and stageb, 2005–2015, non-Hispanic AI/ANc and non-Hispanic white females, PRCDA counties: a mastectomy trends, overall, NH AI/AN and NHW, b mastectomy trends by stage, NH AI/AN and NHW. aSurgical treatment according to SEER surgery codes, breast, RX summ-surg prim site 01–24 (lumpectomy), 30–80 (mastectomy), code 00 and > 80 excluded from analysis. bAJCC 7 staging, Early stage: I, II. Late stage; III, IV; excluding Paget’s disease. cAI/ANrace is reported by NPCR and SEER registries or through linkage with the HIS patient registration database. Includes only AI/AN of non-Hispanic origin
Discussion
By using cancer registry data linked with the IHS patient registration database, we detected differences in the surgical management of breast cancer for NH-AI/AN and NHW women. NH-AI/AN women with early-stage breast cancer had significantly higher reported use of mastectomy compared with NHW women (41% versus 34.4%, p < 0.001). These differences were prominent for NH-AI/AN women from the Northern Plains and Alaska, where 47–49% received mastectomy compared with 33–36% of NHW women in the same region. When BCT was implemented, we found no overall differences in postlumpectomy radiation between NH-AI/AN and NHW women, but did identify three regions where NH-AI/AN women were more likely than NHW women to undergo postlumpectomy radiation, a trend seen elsewhere in lower socioeconomic groups.35 Disparities in breast cancer screening, stage, and morbidity/mortality have been examined previously for AI/AN women compared with the general population; 1,2,3,4,5,36,37 however, we believe this is the first study to specifically examine disparities in breast cancer surgery for AI/AN women.
Cancer Disparities
Research has demonstrated that AI/AN patients are less likely to receive guideline-concordant cancer care related to surgery, adjuvant therapy, and surveillance.3,4,5,38 These are important factors considering that AI/AN patients have the worst cancer survival rates of any US ethnic group.4,39 SEER analyses have shown that AI/AN women are less likely to receive standard adjuvant chemotherapy for breast cancer,3,5,37,38,40 and other data have likewise shown a lower likelihood of receiving guideline-concordant preoperative biopsy, adjuvant therapy, and post-therapy surveillance, and higher likelihood of significant treatment delays.3,4,5,37,40 Endocrine therapy for breast cancer has been shown to be less optimally used in women from other minority groups, but these studies did not include AI/AN women.41 In a chart review of Navajo patients with breast cancer, 30% did not receive standard care, which was attributed to cultural, structural, and geographic challenges.42,43
Surgical Disparities
Differences in surgery have been noted for other minority women. Hispanic and African American women have been shown to have higher mastectomy rates.44 Two studies of Hispanic women with early-stage disease showed lower odds of lumpectomy.45,46 A study of Medicare beneficiaries in Alabama found that residents with lower socioeconomic status (SES) were more likely to undergo mastectomy and postlumpectomy radiation, similar to our findings.35 AI/AN women have been shown to have longer lengths of stay and half the likelihood of outpatient breast surgery.47,48 Other studies have shown lower rates of breast reconstruction for racial minorities,20,44,49 but information on postmastectomy reconstruction was not available for the present study.
After a steady increase in BCT in the 1990s, a phenomenon of increased bilateral mastectomies occurred with differences related to race and SES, and a further inflection after Angelina Jolie’s highly publicized surgery in 2013.9,50,51 In a study on patterns of contralateral prophylactic mastectomy (CPM), White women had 50% greater likelihood of CPM compared with minority women and those privately insured had 62% greater likelihood.52 This trend of White and privately insured women electing mastectomy when eligible for lumpectomy might be narrowing the disparity in our study, which is noteworthy since the findings remained robust. Research has shown rurality affects reconstruction as patients from surgical deserts are significantly less likely to receive reconstruction.49 The lower reconstruction rates for rural women and minorities suggest that AI/AN women are similarly vulnerable.
There are documented advantages of BCT compared with mastectomy. From a systems perspective, the cost of lumpectomy is lower, particularly compared with mastectomy with reconstruction, although the radiation fees associated with BCT can variably impact the cost savings.53,54 From the patient’s perspective, BCT has been consistently cited to have fewer complications, less pain, faster recovery, more favorable cosmetics, and better preserved sexuality, body image, and quality of life.6,7,12,13,14,15,16,55 In consideration of the potential differences in cost and quality of life, in addition to the known equivalent survival, the higher mastectomy rate of 41% for NH-AI/AN women compared with 34% for NHW women with early-stage breast cancer is not only statistically significant but possibly clinically significant across these parameters. Addressing this disparity in the Northern Plains and Alaska where the difference is particularly prominent might have even greater clinical impact for these regions. AI/AN women with early-stage disease undergoing mastectomy for what might otherwise be treated with lumpectomy may be disproportionately impacted on these measures, though it must be acknowledged that selection of mastectomy might occur for clinical reasons.
Radiation Disparities
Radiation therapy (RT) is a critical component of BCT as it lowers local recurrence compared with lumpectomy alone and provides survival outcomes comparable to mastectomy.56 RT is costly and delivered at specialty centers, most often urban. Conventional RT requires daily visits for up to 7 weeks, which can be prohibitive to those on rural, tribal lands.56,57 Prior research has shown a relationship between mastectomy and RT accessibility, with one study finding a 44% greater likelihood of mastectomy for remote patients.57,58,59 We had hypothesized that higher mastectomy for AI/AN women might be driven by lower access to RT; however, our data showed nonsignificant differences in RT between NH-AI/AN and NHW women overall, and increased utilization in three regions. We do not have detailed RT data in terms of course length, or whole-breast versus partial-breast irradiation (PBI). A study examining PBI, which can be delivered in 5 days, found that AI/AN women used PBI more than twice as often as their urban counterparts.56 With limited RT data available, the primary purpose of this study was to characterize differences in surgical treatment.
Geographic Barriers
The georemote location of reservations is another factor potentially contributing to surgical disparities.2,38 Prior studies show longer travel time to breast imaging facilities may influence actual breast cancer treatment, wherein greater distance is associated with higher probability of mastectomy, as well as decreased postlumpectomy radiation.11,59,60,61,62,63,64 Distance may be contributing to NH-AI/AN women’s selection of mastectomy as it may be the better individual choice if distance to a radiation facility is prohibitive to lumpectomy. In a study of over 92 million women, AI/AN women had longer median travel times to all breast imaging modalities compared with all racial/ethnic groups.64 AI/AN women have been widely documented to underutilize screening services with geography a key factor.1,36,64,65 Compounding geography, inclement weather heightens barriers as women with greater travel distances are less likely to undergo mammogram during winter.64,66 Of note, the two regions in our study where NH-AI/AN women had the highest percentages of mastectomy are the Northern Plains and Alaska, which have notorious winters and rurality. There are many benefits to concentrating resources at high-volume centers; however, their urban location can adversely skew treatment for rural patients.61 This can be particularly exacerbated for AI/AN patients because the IHS does not have onsite oncology facilities and can only refer patients to tertiary cancer centers through Purchased Referred Care.2,3,38 Geographic distance becomes further problematic in that those in rural areas with less financial means, relevant for AI/AN populations, may not have transportation or time from work for extended travel to maintain treatment.38
Limitations
While this study utilized the most accurate, up-to-date data for cancer incidence in NH-AI/AN populations, there are limitations. Because racial misclassification was addressed through linkage with the IHS, these corrections for misclassification applied only to persons who are members of federally recognized tribes and accessed services through the IHS. The exclusion of Hispanic AI/AN persons and data from some registries may disproportionately impact AI/AN data from certain regions. Individuals living in urban non-PRCDA areas are also not represented in this data; future analyses will be needed to address these limitations. While we evaluated several clinical characteristics, this study is descriptive in nature, and therefore we were unable to take into account potential confounding by other factors between race/ethnicity and surgical treatment. Additionally, RT data may be underreported in cancer registries.67 The present RT analysis is limited to those with complete data, therefore future efforts to more fully characterize RT are needed. Lastly, we did not have information regarding comorbidities or anatomic factors that might influence appropriateness of one operation over the other.
Conclusions
This study demonstrates that NH-AI/AN women with early-stage disease are undergoing mastectomy at higher percentage than NHW women. We contribute a new and important finding that there are surgical disparities in breast cancer for NH-AI/AN women. In terms of BCT, our study also shows that, when lumpectomy is selected, it is consistently followed by radiation for both groups overall, but with key regional differences. Northern Plains, Alaska, and Southwest had statistically significant higher rates of postlumpectomy radiation for NH-AI/AN women. How these regions succeed at standard BCT for NH-AI/AN women who prefer it would be important knowledge for other service areas. Future directions in breast cancer care for AI/AN women could consider the personal and systems factors that lead to increased mastectomy and how access to BCT might be improved for those who otherwise prefer it. Partnerships between academic/tertiary centers and tribal facilities, mobile screening units, telemedicine, patient navigation, transportation assistance, utilization of accelerated or partial-breast irradiation, all with cultural and linguistic sensitivity at the forefront, are avenues to increase AI/AN access to BCT. Dismantling cancer disparities is a complex, multilevel task demanding multidisciplinary collaboration, but it is of utmost importance for AI/AN women who endure a legacy of colonization, displacement, and poverty, all of which negatively impact health including cancer detection, treatment, and survivorship.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Change history
19 September 2021
The authors’ affiliations have been updated.
References
Daley CMFM, Nazir N, James AS, Brokenleg S, Braiuca S, Greiner KA, Choi WS. Breast cancer screening practices among American Indian and Alaska Natives in the Midwest. J Health Disparities Res Pract. 2011;4(3):75–81.
Goodwin EA, Burhansstipanov L, Dignan M, Jones KL, Kaur JS. The experience of treatment barriers and their influence on quality of life in American Indian/Alaska Native breast cancer survivors. Cancer. 2017;123(5):861–8.
Javid SH, Varghese TK, Morris AM, et al. Guideline-concordant cancer care and survival among American Indian/Alaskan Native patients. Cancer. 2014;120(14):2183–90.
Markin A, Habermann EB, Zhu Y, et al. Cancer surgery among American Indians. JAMA Surg. 2013;148(3):277–284; discussion 284.
Simianu VV, Morris AM, Varghese TK Jr, et al. Evaluating disparities in inpatient surgical cancer care among American Indian/Alaska Native patients. Am J Surg. 2016;212(2):297–304.
Anderson C, Islam JY, Elizabeth Hodgson M, et al. Long-term satisfaction and body image after contralateral prophylactic mastectomy. Ann Surg Oncol. 2017;24(6):1499–506.
Chatterjee A, Pyfer B, Czerniecki B, Rosenkranz K, Tchou J, Fisher C. Early postoperative outcomes in lumpectomy versus simple mastectomy. J Surg Res. 2015;198(1):143–8.
Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–41.
Mamtani A, Morrow M. Why are there so many mastectomies in the United States? Annu Rev Med. 2017;68:229–41.
Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347(16):1227–32.
Yang RL, Wapnir I. Hispanic breast cancer patients travel further for equitable surgical care at a comprehensive cancer center. Health Equity. 2018;2(1):109–16.
Grogan S, Mechan J. Body image after mastectomy: a thematic analysis of younger women’s written accounts. H Health Psychol. 2017;22(11):1480–90.
Ng ET, Ang RZ, Tran BX, et al. Comparing quality of life in breast cancer patients who underwent mastectomy versus breast-conserving surgery: a meta-analysis. Int J Environ Res Public Health. 2019;16(24).
Sinnadurai S, Kwong A, Hartman M, et al. Breast-conserving surgery versus mastectomy in young women with breast cancer in Asian settings. BJS Open. 2019;3(1):48–55.
Tait RC, Zoberi K, Ferguson M, et al. Persistent Post-mastectomy pain: risk factors and current approaches to treatment. J Pain. 2018;19(12):1367–83.
Turk KE, Yilmaz M. The effect on quality of life and body image of mastectomy among breast cancer survivors. Eur J Breast Health. 2018;14(4):205–10.
Hampton T. Studies address racial and geographic disparities in breast cancer treatment. JAMA. 2008;300(14):1641.
Shavers VL, Brown ML. Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst. 2002;94(5):334–57.
Tseng JF, Kronowitz SJ, Sun CC, et al. The effect of ethnicity on immediate reconstruction rates after mastectomy for breast cancer. Cancer. 2004;101(7):1514–23.
Yang RL, Newman AS, Reinke CE, et al. Racial disparities in immediate breast reconstruction after mastectomy: impact of state and federal health policy changes. Ann Surg Oncol. 2013;20(2):399–406.
Espey DK, Wiggins CL, Jim MA, Miller BA, Johnson CJ, Becker TM. Methods for improving cancer surveillance data in American Indian and Alaska Native populations. Cancer. 2008;113(5 Suppl):1120–30.
Jim MA, Arias E, Seneca DS, et al. Racial misclassification of American Indians and Alaska Natives by Indian Health service contract health service delivery area. Am J Public Health. 2014;104(Suppl 3):S295-302.
Hankey BF, Ries LA, Edwards BK. The surveillance, epidemiology, and end results program: a national resource. Cancer Epidemiolo Biomark Prevent Public Am Assoc Cancer Res Cospons Am Soc Prevent Oncol. 1999;8(12):1117–21.
Thoburn KK, German RR, Lewis M, Nichols PJ, Ahmed F, Jackson-Thompson J. Case completeness and data accuracy in the centers for disease control and prevention’s national program of cancer registries. Cancer. 2007;109(8):1607–16.
Fritz A, Percy C, Jack A. International classification of diseases of oncology. Geneva, Switzerland: World Health Organization; 2000.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–4.
United States Cancer Statistics Publication Criteria. https://www.cdc.gov/cancer/uscs/technical_notes/criteria/index.htm. Accessed October 2020.
Link plus: A suite of publicly available software programs for collecting and processing cancer registry data. Centers for disease control and prevention, national center for chronic disease prevention and health promotion, U.S. Deaprtment of Health and Human Services; 2005.
Arias E, Schauman WS, Eschbach K, Sorlie PD, Backlund E. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Statist Ser 2 Data Eval Methods Res. 2008(148):1–23.
Rothman KJ, Greenland S. Modern Epidemiology. 2nd ed. Philadelphia, PA: Lippincott, Williams and Wilkins; 1998.
Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2000 Statist Notes. 2001(20):1–9.
Surveillance research program, national cancer institute SEER*stat software (seer.cancer.gov/seerstat) version 8.3.8.
Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006;15(6):547–69.
Joinpoint regression program, version 4.7.0—April 2020; Statistical methodology and applications branch, surveillance research program, national cancer institute.
White A, Richardson LC, Krontiras H, Pisu M. Socioeconomic disparities in breast cancer treatment among older women. J Womens Health (Larchmt). 2014;23(4):335–41.
Eberth JM, Huber JC Jr, Rene A. Breast cancer screening practices and correlates among American Indian and Alaska native women in California, 2003. Women’s Health Issues. 2010;20(2):139–45.
Wilson RT, Adams-Cameron M, Burhansstipanov L, et al. Disparities in breast cancer treatment among American Indian, Hispanic and non-Hispanic White women enrolled in Medicare. J Health Care Poor Underserved. 2007;18(3):648–64.
Guadagnolo BA, Petereit DG, Coleman CN. Cancer care access and outcomes for american indian populations in the United States: challenges and models for progress. Sem Radiat Oncol. 2017;27(2):143–9.
Emerson MA, Banegas MP, Chawla N, et al. Disparities in prostate, lung, breast, and colorectal cancer survival and comorbidity status among urban American Indians and Alaskan Natives. Cancer Res. 2017;77(23):6770–6.
Adams SV, Bansal A, Burnett-Hartman AN, et al. Cancer treatment delays in American Indians and Alaska Natives enrolled in Medicare. J Health Care Poor Underserved. 2017;28(1):350–61.
Roberts MC, Wheeler SB, Reeder-Hayes K. Racial/Ethnic and socioeconomic disparities in endocrine therapy adherence in breast cancer: a systematic review. Am J Public Health. 2015;105(Suppl 3):e4–15.
Bea JW, de Heer H, Kinslow B, et al. Perceptions of cancer causes, prevention, and treatment among Navajo cancer survivors. J Cancer Ed. 2020;35(3):493–500.
Flum DR, Stuart S, Wilcox M. Processes and outcomes of care among navajo women with breast cancer. JAMA. 2003;290(15):1996–7.
Mets EJ, Chouairi FK, Gabrick KS, Avraham T, Alperovich M. Persistent disparities in breast cancer surgical outcomes among hispanic and African American patients. Eur J Surg Oncol. 2019;45(4):584–90.
Kurian AW, Lichtensztajn DY, Keegan TH, Nelson DO, Clarke CA, Gomez SL. Use of and mortality after bilateral mastectomy compared with other surgical treatments for breast cancer in California, 1998–2011. JAMA. 2014;312(9):902–14.
Morris CR, Cohen R, Schlag R, Wright WE. Increasing trends in the use of breast-conserving surgery in California. Am J Public Health. 2000;90(2):281–4.
Parsons HM, Habermann EB, Stain SC, Vickers SM, Al-Refaie WB. What happens to racial and ethnic minorities after cancer surgery at American College of Surgeons National Surgical Quality Improvement Program hospitals? J Am Coll Surg. 2012;214(4):539-547; discussion 547-539.
Salasky V, Yang RL, Datta J, et al. Racial disparities in the use of outpatient mastectomy. J Surg Res. 2014;186(1):16–22.
Vora H, Chung A, Lewis A, et al. Reconstruction among patients undergoing mastectomy: the effect of surgical deserts. J Surg Res. 2018;223:237–42.
Huang J, Chagpar AB. Quality of life and body image as a function of time from mastectomy. Ann Surg Oncol. 2018;25(10):3044–51.
Liede A, Cai M, Crouter TF, Niepel D, Callaghan F, Evans DG. Risk-reducing mastectomy rates in the US: a closer examination of the Angelina Jolie effect. Breast Cancer Res Treat. 2018;171(2):435–42.
Grimmer L, Liederbach E, Velasco J, Pesce C, Wang CH, Yao K. Variation in contralateral prophylactic mastectomy rates according to racial groups in young women with breast cancer, 1998 to 2011: a report from the national cancer data base. J Am Coll Surg. 2015;221(1):187–96.
Pataky RE, Baliski CR. Reoperation costs in attempted breast-conserving surgery: a decision analysis. Curr Oncol. 2016;23(5):314–21.
Smith BD, Jiang J, Shih YC, et al. Cost and complications of local therapies for early-stage breast cancer. J Natl Cancer Inst. 2017;109(1).
Reghunathan MTP, Sbitany H, Srinivasa D. Abstract: breast reconstruction effects on past mastectimy pain syndrome: a meta-analysis. PRS Global Open. 2018;6(9):171–2.
Billar JA, Sim MS, Chung M. Increased use of partial-breast irradiation has not improved radiotherapy utilization for early-stage breast cancer. Ann Surg Oncol. 2014;21(13):4144–51.
Gillespie EF, Matsuno RK, Xu B, et al. Geographic disparity in the use of hypofractionated radiation therapy among elderly women undergoing breast conservation for invasive breast cancer. Int J Radiat Oncol Biol Phys. 2016;96(2):251–8.
Goyal S, Chandwani S, Haffty BG, Demissie K. Effect of travel distance and time to radiotherapy on likelihood of receiving mastectomy. Ann Surg Oncol. 2015;22(4):1095–101.
Voti L, Richardson LC, Reis IM, Fleming LE, Mackinnon J, Coebergh JW. Treatment of local breast carcinoma in Florida: the role of the distance to radiation therapy facilities. Cancer. 2006;106(1):201–7.
Albornoz CR, Cohen WA, Razdan SN, et al. The Impact of Travel Distance on Breast Reconstruction in the United States. Plast Reconstruct Surg. 2016;137(1):12–8.
Boscoe FP, Johnson CJ, Henry KA, et al. Geographic proximity to treatment for early stage breast cancer and likelihood of mastectomy. Breast. 2011;20(4):324–8.
Elkin EB, Ishill NM, Snow JG, et al. Geographic access and the use of screening mammography. Med Care. 2010;48(4):349–56.
Onega T, Cook A, Kirlin B, et al. The influence of travel time on breast cancer characteristics, receipt of primary therapy, and surveillance mammography. Breast Cancer Res Treat. 2011;129(1):269–75.
Onega T, Hubbard R, Hill D, et al. Geographic access to breast imaging for US women. J Am Coll Radiol. 2014;11(9):874–82.
Tangka FK, Subramanian S, Mobley LR, et al. Racial and ethnic disparities among state Medicaid programs for breast cancer screening. Prevent Med. 2017;102:59–64.
Onitilo AA, Liang H, Stankowski RV, et al. Geographical and seasonal barriers to mammography services and breast cancer stage at diagnosis. Rural Remote Health. 2014;14(3):2738.
Malin JL, Kahn KL, Adams J, Kwan L, Laouri M, Ganz PA. Validity of cancer registry data for measuring the quality of breast cancer care. J Natl Cancer Inst. 2002;94(11):835–44.
Acknowledgment
The work was supported by the Centers for Disease Control and Prevention (CDC). CDC coauthors participated as a part of their official duties.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
No conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Erdrich, J., Cordova-Marks, F., Monetathchi, A.R. et al. Disparities in Breast-Conserving Therapy for Non-Hispanic American Indian/Alaska Native Women Compared with Non-Hispanic White Women. Ann Surg Oncol 29, 1019–1030 (2022). https://doi.org/10.1245/s10434-021-10730-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10730-7