Abstract
Background
This study retrospectively analyzed the feasibility and surgical outcome of an algorithmic approach using negative pressure wound therapy for patients with synchronous hypopharyngeal and esophageal cancer undergoing pharyngolaryngoesophagectomy with gastric tube reconstruction.
Methods
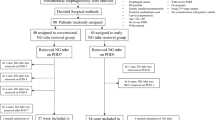
Patients undergoing pharyngolaryngoesophagectomy and gastric tube reconstruction for hypopharyngeal cancer between 2011 and 2019 were candidates for this study. Data were collected on patient demographics, comorbidities, performance status, cancer stage, treatment, complication, and survival. Survival analysis was performed using the Kaplan-Meier method. The Cox proportional hazards model was used for prognostic factors.
Results
The study enrolled 43 patients. Anastomotic leakage was found in 21 of the patients with a conventional surgical drain (61.9%) and in 10 of the 22 patients with negative pressure wound therapy (45.5%) (p = 0.280). Nine patients in the conventional drain group (42.9%) and two patients in the negative pressure wound therapy group (9.1%) had leakage-associated complications (p = 0.011). The incidence of pulmonary complications was higher in the conventional surgical drain group (9 vs 2; p = 0.011). The number of complications requiring surgery was higher in the conventional drain group (7 vs 0; p = 0.004). The overall survival in the negative pressure wound therapy group was better (hazard ratio [HR], 0.33; 95% confidence interval [CI], 0.15–0.76; p = 0.009). Negative pressure wound therapy was independently associated with overall survival (HR, 0.31; 95% CI, 0.13–0.77; p = 0.011).
Conclusions
Negative pressure wound therapy with an algorithmic approach improved the overall survival for the patients undergoing gastric tube reconstruction after pharyngolaryngoesophagectomy for hypopharyngeal and esophageal cancer by preventing deadly complications secondary to anastomotic leakage




Similar content being viewed by others
References
Peracchia A, Bonavina L, Botturi M, Pagani M, Via A, Saino G. Current status of surgery for carcinoma of the hypopharynx and cervical esophagus. Dis Esophagus. 2001;14:95–7.
Hall SF, Groome PA, Irish J, O’Sullivan B. The natural history of patients with squamous cell carcinoma of the hypopharynx. Laryngoscope. 2008;118:1362–71.
Chen YH, Lu HI, Chien CY, et al. Treatment outcomes of patients with locally advanced synchronous esophageal and head/neck squamous cell carcinoma receiving curative concurrent chemoradiotherapy. Sci Rep. 2017;7:41785.
Iyer NG, Tan DS, Tan VK, et al. Randomized trial comparing surgery and adjuvant radiotherapy versus concurrent chemoradiotherapy in patients with advanced, nonmetastatic squamous cell carcinoma of the head and neck: 10-year update and subset analysis. Cancer. 2015;121:1599–607.
Bradley PJ. Epidemiology of hypopharyngeal cancer. Adv Otorhinolaryngol. 2019;83:1–14.
Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer. 2015;112:580–93.
Viner B, Barberio AM, Haig TR, Friedenreich CM, Brenner DR. The individual and combined effects of alcohol consumption and cigarette smoking on site-specific cancer risk in a prospective cohort of 26,607 adults: results from Alberta’s Tomorrow Project. Cancer Causes Control. 2019;30:1313–26.
Hung SH, Tsai MC, Liu TC, Lin HC, Chung SD. Routine endoscopy for esophageal cancer is suggestive for patients with oral, oropharyngeal and hypopharyngeal cancer. PLoS One. 2013;8:e72097.
Wang WL, Wang CP, Wang HP, et al. The benefit of pretreatment esophageal screening with image-enhanced endoscopy on the survival of patients with hypopharyngeal cancer. Oral Oncol. 2013;49:808–13.
Yamamoto Y, Sasaki S, Furukawa H, Okushiba S, Ohno K, Sugihara T. Microsurgical reconstruction of the digestive tract following pharyngolaryngectomy and total esophagectomy. Ann Plast Surg. 1998;41:22–6; discussion 26–7.
Nakatsuka T, Harii K, Ebihara S, et al. Free colon transfer: a versatile method for reconstruction of pharyngoesophageal defects with a large pharyngostoma. Ann Plast Surg. 1996;37:596–603.
Matsubara T, Ueda M, Nakajima T, Kamata S, Kawabata K. Elongated stomach roll with vascular microanastomosis for reconstruction of the esophagus after pharyngolaryngoesophagectomy. J Am Coll Surg. 1995;180:613–5.
Omura K, Misaki T, Watanabe Y, Urayama H, Hashimoto T, Matsu T. Reconstruction with free jejunal autograft after pharyngolaryngoesophagectomy. Ann Thorac Surg. 1994;57:112–7; discussion 117–8.
Asamura H, Kato H, Watanabe H, Tachimori Y, Ebihara S, Harii K. Combined gastric pull-up and microvascular jejunal transfer procedure after pharyngolaryngoesophagectomy. Ann Thorac Surg. 1989;48:423–5.
Tabah RJ, Flynn MB, Acland RD, Banis JC Jr. Microvascular free tissue transfer in head and neck and esophageal surgery. Am J Surg. 1984;148:498–504.
Dai Z, He Q, Pan B, Liu L, Zhou D. Postoperative complication assessments of different reconstruction procedures after total pharyngolaryngoesophagectomy: tubular gastric pull-up versus whole gastric pull-up. Am Surg. 2018;84:1927–31.
Sugiyama N, Takao S, Suzuki E, Kimata Y. Risk factors for wound complications in head and neck reconstruction: 773 free jejunal reconstruction procedures after total pharyngolaryngoesophagectomy. Head Neck. 2017;39:2057–69.
Miyata H, Sugimura K, Motoori M, et al. Clinical assessment of reconstruction involving gastric pull-up combined with free jejunal graft after total pharyngolaryngoesophagectomy. World J Surg. 2017;41:2329–36.
Liu J, Zhang Y, Li Z, Liu S, Li H, Xu Z. Benefit of salvage total pharyngolaryngoesophagectomy for recurrent locally advanced head and neck cancer after radiotherapy. Radiat Oncol. 2017;12:164.
Meulemans J, Couvreur F, Beckers E, et al. Oncologic and functional outcomes after primary and salvage laryngopharyngoesophagectomy with gastric pull-up reconstruction for locally advanced hypopharyngeal squamous cell carcinoma. Front Oncol. 2019;9:735.
McLean JN, Nicholas C, Duggal P, et al. Surgical management of pharyngocutaneous fistula after total laryngectomy. Ann Plast Surg. 2012;68:442–5.
Umezawa H, Matsutani T, Yokoshima K, Nakamizo M, Ogawa R. A novel tube-drainage technique of negative pressure wound therapy for fistulae after reconstructive surgery. Plast Reconstr Surg Glob Open. 2018;6:e1885.
Andrews BT, Smith RB, Goldstein DP, Funk GF. Management of complicated head and neck wounds with vacuum-assisted closure system. Head Neck. 2006;28:974–81.
Teixeira S, Costa J, Bartosch I, Correia B, Silva A. Management of pharyngocutaneous fistula with negative pressure wound therapy. J Craniofac Surg. 2017;28:e364–7.
Ho CM, Lam KH, Wei WI, Yuen PW, Lam LK. Squamous cell carcinoma of the hypopharynx: analysis of treatment results. Head Neck. 1993;15:405–12.
Morita M, Saeki H, Ito S, et al. Technical improvement of total pharyngo-laryngo-esophagectomy for esophageal cancer and head and neck cancer. Ann Surg Oncol. 2014;21:1671–7.
Puttawibul P, Pornpatanarak C, Sangthong B, et al. Results of gastric pull-up reconstruction for pharyngolaryngo-oesophagectomy in advanced head and neck cancer and cervical oesophageal squamous cell carcinoma. Asian J Surg. 2004;27:180–5.
Booka E, Takeuchi H, Nishi T, et al. The impact of postoperative complications on survivals after esophagectomy for esophageal cancer. Med Baltim. 2015;94:e1369.
Markar S, Gronnier C, Duhamel A, et al. The impact of severe anastomotic leak on long-term survival and cancer recurrence after surgical resection for esophageal malignancy. Ann Surg. 2015;262:972–80.
Ogura M, Takeuchi H, Kawakubo H, et al. Clinical significance of CXCL-8/CXCR-2 network in esophageal squamous cell carcinoma. Surgery. 2013;154:512–20.
Kataoka K, Takeuchi H, Mizusawa J, et al. Prognostic impact of postoperative morbidity after esophagectomy for esophageal cancer: exploratory analysis of JCOG9907. Ann Surg. 2017;265:1152–7.
Okita Y, Kobayashi M, Araki T, et al. Impact of Surgical Infection Society/Infectious Disease Society of America-recommended antibiotics on postoperative intra-abdominal abscess with image-guided percutaneous abscess drainage following gastrointestinal surgery. Surg Today. 2015;45:993–1000.
Okita Y, Mohri Y, Kobayashi M, et al. Factors influencing the outcome of image-guided percutaneous drainage of intra-abdominal abscess after gastrointestinal surgery. Surg Today. 2013;43:1095–102.
McNeeley MF, Vo NJ, Prabhu SJ, Vergnani J, Shaw DW. Percutaneous drainage of intra-abdominal abscess in children with perforated appendicitis. Pediatr Radiol. 2012;42:805–12.
Ballard DH, Erickson AEM, Ahuja C, Vea R, Sangster GP, D’Agostino HB. Percutaneous management of enterocutaneous fistulae and abscess-fistula complexes. Dig Dis Interv. 2018;2:131–40.
Gedda S, van der Linden W. What makes the peritoneal drain work? Pressure in the subhepatic space after biliary surgery. Acta Chir Scand. 1983;149:703–6.
Jiang T, Li J, Ren J. Continuous negative pressure drain is associated with better outcome: a randomized prospective trial in plastic surgery patients. Aesth Plast Surg. 2019;43:91–7.
Schintler M, Maier A, Matzi V, Smolle-Juttner FM. Vacuum-assisted closure system in the management of cervical anastomotic leakage after gastric pull-up. Interact Cardiovasc Thorac Surg. 2004;3:92–4.
Kim SI, Lim MC, Song YJ, Seo SS, Kang S, Park SY. Application of a subcutaneous negative pressure drain without subcutaneous suture: impact on wound healing in gynecologic surgery. Eur J Obstet Gynecol Reprod Biol. 2014;173:94–100.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chang, CC., Tang, WR., Huang, WL. et al. Algorithmic Approach Using Negative Pressure Wound Therapy Improved Survival for Patients with Synchronous Hypopharyngeal and Esophageal Cancer Undergoing Pharyngolaryngoesophagectomy with Gastric Tube Reconstruction. Ann Surg Oncol 28, 8996–9007 (2021). https://doi.org/10.1245/s10434-021-10365-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10365-8