Abstract
Background
Neoadjuvant chemotherapy (NAC) downstages breast cancer and provides prognostic information. Males with breast cancer are known to receive less treatment overall and have poorer outcomes relative to females. We hypothesized that males would be less likely to receive NAC.
Patients and methods
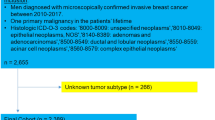
Patients with a primary diagnosis of cN1–3 breast cancer were identified in the National Cancer Database (2004–2016). Multivariable logistic regression determined the association between NAC utilization and sex, and the relationship between sex and NAC response, controlling for demographic and tumor factors. Overall survival was analyzed using a multivariable Cox model.
Results
In total, 196,027 patients (194,010 females, 2017 males) met inclusion criteria. A significantly greater proportion of males underwent mastectomy (80% vs. 60%, P < 0.001), and axillary lymph node dissection (76% vs. 74%, P = 0.022). Overall fewer men received chemotherapy than women (73% vs. 84%, P < 0.001); men also received NAC at a significantly lower rate (26% men vs. 45% women, P < 0.001). After accounting for demographic and oncologic factors including hormone receptor (HR) subtype, females remained more likely to undergo NAC (OR 1.84, P < 0.001). On multivariable analysis, sex was not associated with pathologic response or overall survival after NAC.
Conclusions
Although oncologic outcomes after NAC were similar, males with node-positive breast cancer received less NAC and more aggressive surgery than females. These data suggest men achieve outcomes comparable to women with cN1–3 disease, and NAC should be used in appropriate male patients to downstage the breast and axilla.

Similar content being viewed by others
References
Petruolo O, Sevilimedu V, Montagna G, Le T, Morrow M, Barrio AV. How often does modern neoadjuvant chemotherapy downstage patients to breast-conserving surgery? Ann Surg Oncol. 2021;28(1):287–94.
Untch M, Konecny GE, Paepke S, von Minckwitz G. Current and future role of neoadjuvant therapy for breast cancer. Breast. 2014;23(5):526–37.
Cortazar, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384(9938):164–72.
Von Minckwitz G, Untch M, Blohmer JU, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30(15):1796–804.
Santonja A, Sanchez-Munoz A, Lluch A, et al. Triple negative breast cancer subtypes and pathologic complete response rate to neoadjuvant chemotherapy. Oncotarget. 2018;9(41):26406–16.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30.
White J, Kearins O, Dodwell D, Horgan K, Hanby AM, Speirs V. Male breast carcinoma: increased awareness needed. Breast Cancer Res. 2011;13(5):219.
William JGBOA, Jame A, Rebecca A, Doreen A, Kimberly HA, Sarah LB. NCCN guidelines: breast cancer, version 6. J Natl Compr Cancer Netw. 2020;2:20.
Anderson WF, Jatoi I, Tse J, Rosenberg PS. Male breast cancer: a population-based comparison with female breast cancer. J Clin Oncol. 2010;28(2):232–9.
Liu N, Johnson KJ, Ma CX. Male breast cancer: an updated surveillance, epidemiology, and end results data analysis. Clin Breast Cancer. 2018;18(5):e997–1002.
National Cancer Data Base Participant User File (PUF) Data Dictionary Version: PUF 2016 – Containing cases diagnosed in 2004–2016. 2016.
Organization WH. International classification of diseases for oncology (ICD-O)–3rd edition. 2013; 1st revision(3rd ed).
Schott AF, Hayes DF. Defining the benefits of neoadjuvant chemotherapy for breast cancer. J Clin Oncol. 2012;30(15):1747–9.
Scholl SM, Fourquet A, Asselain B, et al. Neoadjuvant versus adjuvant chemotherapy in premenopausal patients with tumours considered too large for breast conserving surgery: preliminary results of a randomised trial: S6. Eur J Cancer. 1994;30A(5):645–52.
Van J, Hage C, Velde JJ, Tubiana-Hulin M, Vandervelden C. Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902, in Impact of age, tumor characteristics, and treatment on local control and disease outcome in early stage breast cancer. 2001:33.
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr. 2001;30:96–102.
Nguyen TT, Hoskin TL, Day CN, et al. Decreasing use of axillary dissection in node-positive breast cancer patients treated with neoadjuvant chemotherapy. Ann Surg Oncol. 2018;25(9):2596–602.
Caudle AS, Yu TK, Tucker SL, et al. Local-regional control according to surrogate markers of breast cancer subtypes and response to neoadjuvant chemotherapy in breast cancer patients undergoing breast conserving therapy. Breast Cancer Res. 2012;14(3):83.
Tadros AB, Yang WT, Krishnamurthy S, et al. Identification of patients with documented pathologic complete response in the breast after neoadjuvant chemotherapy for omission of axillary surgery. JAMA Surg. 2017;152(7):665–70.
Park JW, Minetta CL, Douglas Y, Angela DM, Laura VV, Nola H, Fraser S, et al. Abstract CT227: neratinib plus standard neoadjuvant therapy for high-risk breast cancer: efficacy results from the I-SPY 2 TRIAL. AACR. 2014;3:227.
Wuerstlein R, Harbeck N. Neoadjuvant therapy for HER2 − positive breast cancer. Rev Recent Clin Trials. 2017;12(2):81–92.
Buzdar A, Valero V, Theriault R, Frye D, Green M, Booser D, Guerra L, Sahin A, Ames F, Smith T, Singletary E. Pathological complete response to chemotherapy is related to hormone receptor status. Br Cancer Res Treat. 2003;7:82.
Coates AS, Colleoni M, Goldhirsch A. Is adjuvant chemotherapy useful for women with luminal a breast cancer? J Clin Oncol. 2012;30(12):1260–3.
Acknowledgment
This research did not receive any specific funding from agencies in the public, commercial, or nonprofit sectors except the institutional funds made available to the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was presented in e-Poster format at the Society of Surgical Oncology International Conference on Surgical Cancer Care, March 18-19, 2021
Rights and permissions
About this article
Cite this article
Cao, L., Hue, J.J., Freyvogel, M. et al. Despite Equivalent Outcomes, Men Receive Neoadjuvant Chemotherapy Less Often Than Women for Lymph Node-Positive Breast Cancer. Ann Surg Oncol 28, 6001–6011 (2021). https://doi.org/10.1245/s10434-021-09857-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09857-4