Abstract
Purpose
The prognostic impact of radiographic splenic vessel involvement in pancreatic cancer remains unclear. We evaluate its oncological significance in resectable pancreatic body/tail cancer.
Patients and Methods
We retrospectively review 102 cases of resectable pancreatic cancer and 51 of borderline resectable pancreatic cancer (BRPC) who underwent pancreatectomy for pancreatic body/tail cancer. Resectable pancreatic body/tail cancer was classified into one of three categories based on radiographic splenic vessel involvement.
Results
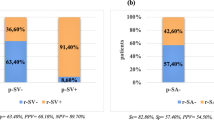
Among 102 cases of resectable pancreatic cancer, 37 (36.3%), 35 (34.3%), and 30 cases (29.4%) were classified as no splenic vessel involvement (Rnone), splenic vein involvement (RV), and splenic artery involvement (RA), respectively. Disease-free survival (DFS) among patients with Rnone, RV, RA, and BRPC was 58.5, 18.4, 10.8, and 9.2 months, respectively. Patients with RV and RA had significantly poorer DFS than patients with Rnone (P = 0.010, P < 0.001, respectively). Median survival among Rnone, RV, RA, and BRPC was 80.6, 23.4, 15.1, and 21.3 months, respectively. Patients with RV and RA had significantly poorer survival than patients with Rnone (P = 0.001, P < 0.001, respectively) and had short survival similar to that of those with BRPC. Multivariate Cox proportional hazard analysis detected preoperative CA19-9 ≥ 37 IU/L, radiologic splenic vein involvement, radiologic splenic artery involvement, intraoperative bleeding ≥ 500 ml, transfusion, positive washing cytology, and noncompletion of adjuvant therapy as independent prognostic factors.
Conclusions
Radiographic splenic artery involvement is a poor prognostic factor in resectable pancreatic body/tail cancer and may have a role in stratification of treatment strategy.



Similar content being viewed by others
References
National Comprehensive Cancer Network. NCCN practice guidelines for pancreatic cancer, Version 1; 2020. https://www.nccn.org/professionals/physician_gls/PDF/pancreatic.pdf.
Shimada K, Sakamoto Y, Sano T, Kosuge T. Prognostic factors after distal pancreatectomy with extended lymphadenectomy for invasive pancreatic adenocarcinoma of the body and tail. Surgery 2006;139:288–95.
Kanda M, Fujii T, Sahin TT, et al. Invasion of the splenic artery is a crucial prognostic factor in carcinoma of the body and tail of the pancreas. Ann Surg. 2010;251:483–7.
Partelli S, Crippa S, Barugola G, et al. Splenic artery invasion in pancreatic adenocarcinoma of the body and tail: a novel prognostic parameter for patient selection. Ann Surg Oncol. 2011;18:3608–14.
Fukami Y, Kaneoka Y, Maeda A, Takayama Y, Onoe S. Prognostic impact of splenic artery invasion for pancreatic cancer of the body and tail. Int J Surg. 2016;35:64–8.
Mizumoto, T, Toyama H, Asari S, et al. Pathological and radiological splenic vein involvement are predictors of poor prognosis and early liver metastasis after surgery in patients with pancreatic adenocarcinoma of the body and tail. Ann Surg Oncol. 2018;25:638–46.
Hyun JJ, Rose JB, Alseidi AA, et al. Significance of radiographic splenic vessel involvement in the pancreatic ductal adenocarcinoma of the body and tail of the gland. J Surg Oncol. 2019;120:262–9.
Strasberg SM, Drebin JA, Linehan D. Radical antegrade modular pancreatosplenectomy. Surgery. 2003;133:521–7.
Hirano S, Kondo S, Hara T, et al. Distal pancreatectomy with en bloc celiac axis resection for locally advanced pancreatic body cancer: long-term results. Ann Surg. 2007;246:46–51.
Okada K, Kawai M, Tani M, et al. Surgical strategy for patients with pancreatic body/tail carcinoma: who should undergo distal pancreatectomy with en-bloc celiac axis resection? Surgery 2013;153:365–372.
James D. Brierley, Mary K. Gospodarowicz, Christian Wittekind. TNM classification of malignant tumours. 8th ed. Hoboken: Wiley-Blackwell; 2017.
Strobel O, Hank T, Hinz U, et al. Pancreatic cancer surgery: the new R-status counts. Ann Surg. 2017;265:565–573.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213.
Bassi C, Marchegiani G, Dervenis C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 2017;161:584–91.
Wente MN, Bassi C, Dervenis C, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2007;142:761–768.
Hirono S, Kawai M, Okada KI, et al. treatment strategy for borderline resectable pancreatic cancer with radiographic artery involvement. Pancreas 2016;45:1438–1446.
Yamaue H, Satoi S, Kanbe T, et al. Phase II clinical study of alternate-day oral therapywithS-1 as first-line chemotherapy for locally-advanced and metastatic pancreatic cancer. Cancer Chemother Pharmacol. 2014;73:97–102.
Okada KI, Kawai M, Hirono S, et al. Impact of treatment duration of neoadjuvant FIRINOX in patients with borderline resectable pancreatic cancer: a pilot trial. Cancer Chemother Pharmacol. 2016;78:719–26.
Okada KI, Hirono S, Kawai M, et al. Phase I study of nab-paclitaxel plus gemcitabine as neoadjuvant therapy for borderline resectable pancreatic cancer. Anticancer Res. 2017;37:853–858.
Oettle H, Neuhaus P, Hochhaus A, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310:1473–81.
Uesaka K, Boku N, Fukutomi A, et al; JASPAC 01 Study Group. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet. 2016;388:248–57.
Tani M, Kawai M, Terasawa H, et al. Does postoperative chemotherapy have a survival benefit for patients with pancreatic cancer? J Surg Oncol. 2006;93:485–90.
Takahashi H, Akita H, Gotoh K, et al. Preoperative gemcitabine-based chemoradiation therapy for pancreatic ductal adenocarcinoma of the body and tail: impact of splenic vessels involvement on operative outcome and pattern of recurrence. Surgery. 2015;157:484–95.
Yang R, Lu M, Qian X, et al. Diagnostic accuracy of EUS and CT of vascular invasion in pancreatic cancer: a systematic review. J Cancer Res Clin Oncol. 2014;140: 2077–86.
Mitsunaga S, Hasebe T, Kinoshita T, et al. Detail histologic analysis of nerve plexus invasion in invasive ductal carcinoma of the pancreas and its prognostic impact. Am J Surg Pathol. 2007;31:1636–44.
Makino I, Kitagawa H, Ohta T, et al. Nerve plexus invasion in pancreatic cancer: spread patterns on histopathologic and embryological analyses. Pancreas 2008;37:358–65.
Shimada K, Nara S, Esaki M, Sakamoto Y, Kosuge T, Hiraoka N. Intrapancreatic nerve invasion as a predictor for recurrence after pancreaticoduodenectomy in patients with invasive ductal carcinoma of the pancreas. Pancreas 2011;40:464–8.
Stopczynski RE, Normolle DP, Hartman DJ, et al. Neuroplastic changes occur early in the development of pancreatic ductal adenocarcinoma. Cancer Res. 2014;74:1718–27.
Amit M, Na’ara S, Gil Z. Mechanisms of cancer dissemination along nerves. Nat Rev Cancer. 2016;16:399–408.
Nagakawa T, Kayahara M, Ohta T, et al. Patterns of neural and plexus invasion of human pancreatic cancer and experimental cancer. Int J Pancreatol. 1991;10:113–119.
Fabre JM, Houry S, Manderscheid JC, et al. Surgery for left-sided pancreatic cancer. Br J Surg. 1996;83:1065–1070.
Jang JY, Han Y, Lee H, et al. Oncological benefits of neoadjuvant chemoradiation with gemcitabine versus upfront surgery in patients with borderline resectable pancreatic cancer: a prospective, randomized, open-label, multicenter phase 2/3 trial. Ann Surg. 2018;268:215–22.
Blazer M, Wu C, Goldberg RM, et al. Neoadjuvant modified (m) FOLFIRINOX for locally advanced unresectable (LAPC) and borderline resectable (BRPC) adenocarcinoma of the pancreas. Ann Surg Oncol. 2015;22:1153–9.
Murakami Y, Uemura K, Sudo T, et al. Survival impact of neoadjuvant gemcitabine plus S-1 chemotherapy for patients with borderline resectable pancreatic carcinoma with arterial contact. Cancer Chemother Pharmacol. 2017;79:37–47.
Eguchi H, Takeda Y, Takahashi H, et al. A prospective, open-label, multicenter phase 2 trial of neoadjuvant therapy using full-dose gemcitabine and s-1 concurrent with radiation for resectable pancreatic ductal adenocarcinoma. Ann Surg Oncol. 2019;26:4498–4505.
Reni M, Balzano G, Zanon S, et al. Safty and efficacy of preoperative or postoperative chemotherapy for resectable pancreatic adenocarcinoma (PACT-15): a randomised, open-label, phase 2–3 trial. Lancet Gastroenterol Hepatol. 2018;3:413–423.
de Geus SW, Eskander MF, Bliss LA, et al. Neoadjuvant therapy versus upfront surgery for resected pancreatic adenocarcinoma: A nationwide propensity score matched analysis. Surgery 2017;161:592–601.
Mokdad AA, Minter RM, Zhu H, et al. Neoadjuvant therapy followed by resection versus upfront resection for resectable pancreatic cancer: a propensity score matched analysis. J Clin Oncol 2017;35:515–22.
Nelson DW, Chang SC, Grunkemeier G, et al. Resectable distal pancreas cancer: time to reconsider the role of upfront surgery. Ann Surg Oncol 2018;25:4012–4019.
Crippa S, Cirocchi R, Maisonneuve P, et al. Systematic review and meta-analysis of prognostic role of splenic vessels infiltration in resectable pancreatic cancer. Eur J Surg Oncol 2018;44:24–30.
Malleo G, Maggino L, Ferrone CR, et al. Number of examined lymph nodes and nodal status assessment in distal pancreatectomy for body/tail ductal adenocarcinoma. Ann Surg. 2019;270:1138–1146.
Asano D, Nara S, Kishi Y, et al. A single-institution validation study of lymph node staging by the AJCC 8th edition for patients with pancreatic head cancer: a proposal to subdivide the N2 category. Ann Surg Oncol. 2019;26:2112–20.
Malleo G, Maggino L, Nobile S, et al. Reappraisal of nodal staging and study of lymph node station involvement in distal pancreatectomy for body-tail pancreatic ductal adenocarcinoma. Eur J Surg Oncol. 2020. https://doi.org/10.1016/j.ejso.2020.04.006.
Acknowledgment
We acknowledge editing and proofreading by Benjamin Phillis from the Clinical Study Support Center at Wakayama Medical University.
Funding
This study is our own work. It has not received outside funding.
Author information
Authors and Affiliations
Contributions
Study concept and design: Kawai and Yamaue. Data collection, analysis, and interpretation: Kawai, Hirono, Okada, Miyazawa, Kitahata, Kobayashi, Ueno, and Hayami. Writing: Kawai. Critical revision: Yamaue and Kawai. All the authors approved the final version to be published and each is accountable for all aspects of the work.
Corresponding author
Ethics declarations
Disclosure
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kawai, M., Hirono, S., Okada, Ki. et al. Radiographic Splenic Artery Involvement Is a Poor Prognostic Factor in Upfront Surgery for Patients with Resectable Pancreatic Body and Tail Cancer. Ann Surg Oncol 28, 1521–1532 (2021). https://doi.org/10.1245/s10434-020-08922-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08922-8