Abstract
Purpose
This study was designed to present the secondary imaging endpoints of the trial for evaluating mammogram (MMG), ultrasound (US) and image guided biopsy (IGBx) assessment of pathologic complete response (pCR) in breast cancer (BC) patients undergoing neoadjuvant chemotherapy (NAC).
Methods
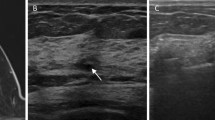
Patients with T1–3, N0–3, M0 triple-negative or HER2-positive BC who received NAC were enrolled in an Institutional Review Board-approved prospective, clinical trial. Patients underwent US and MMG at baseline and after NAC. Images were evaluated for residual abnormality and to determine modality for IGBx [US-guided (USG) or stereotactic guided (SG)]. Fine-needle aspiration and 9-G, vacuum-assisted core biopsy (VACBx) of tumor bed was performed after NAC and was compared with histopathology at surgery.
Results
Forty patients were enrolled. Median age was 50.5 (range 26–76) years; median baseline tumor size was 2.4 cm (range 0.8–6.3) and 1 cm (range 0–5.5) after NAC. Nineteen patients had pCR: 6 (32%) had residual Ca2+ presurgery, 5 (26%) residual mass, 1 (5%) mass with calcifications, and 7 (37%) no residual imaging abnormality. Sensitivity, specificity, and accuracy of US, MMG, and IGBx for pCR were 47/95/73%, 53/90/73%, and 100/95/98%, respectively. Twenty-five (63%) patients had SGBx and 15 (37%) had US-guided biopsy (USGBx). Median number of cores was higher with SGBx (12, range 6–14) than with USGBx (8, range 4–12), p < 0.002. Positive predictive value for pCR was significantly higher for SG VACBx than for USG VACBx (100 vs. 60%, p < 0.05).
Conclusions
SG VACBx is the preferred IGBx modality for identifying patients with pCR for trials testing the safety of eliminating surgery.



Similar content being viewed by others
References
Berruti A, Amoroso V, Gallo F, et al. Pathologic complete response as a potential surrogate for the clinical outcome in patients with breast cancer after neoadjuvant therapy: a meta-regression of 29 randomized prospective studies. J Clin Oncol. 2014;32:3883–91.
Houssami N, Macaskill P, von Minckwitz G, Marinovich ML, Mamounas E. Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur J Cancer. 2012;48:3342–54.
von Minckwitz G, Untch M, Blohmer JU, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796–804.
Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Rauch GM, Adrada BE, Kuerer HM, van la Parra RF, Leung JW, Yang WT. Multimodality imaging for evaluating response to neoadjuvant chemotherapy in breast cancer. Am J Roentgenol. 2017;208:290–9.
Chagpar AB, Middleton LP, Sahin AA, et al. Accuracy of physical examination, ultrasonography, and mammography in predicting residual pathologic tumor size in patients treated with neoadjuvant chemotherapy. Ann Surg. 2006;243:257–64.
Keune JD, Jeffe DB, Schootman M, Hoffman A, Gillanders WE, Aft RL. Accuracy of ultrasonography and mammography in predicting pathologic response after neoadjuvant chemotherapy for breast cancer. Am J Surg. 2010;199:477–84.
Yuan Y, Chen XS, Liu SY, Shen KW. Accuracy of MRI in prediction of pathologic complete remission in breast cancer after preoperative therapy: a meta-analysis. Am J Roentgenol. 2010;195:260–8.
Marinovich ML, Houssami N, Macaskill P, et al. Meta-analysis of magnetic resonance imaging in detecting residual breast cancer after neoadjuvant therapy. J Natl Cancer Inst. 2013;105:321–33.
Hylton NM, Blume JD, Bernreuter WK, et al. Locally advanced breast cancer: MR imaging for prediction of response to neoadjuvant chemotherapy—results from ACRIN 6657/I-SPY trial. Radiology. 2012;263:663–72.
Kuerer HM, Rauch GM, Krishnamurthy S, et al. A clinical feasibility trial for identification of exceptional responders in whom breast cancer surgery can be eliminated following neoadjuvant systemic therapy. Ann Surg. 2017. https://doi.org/10.1097/SLA.0000000000002313.
Heil J, Kummel S, Schaefgen B, et al. Diagnosis of pathological complete response to neoadjuvant chemotherapy in breast cancer by minimal invasive biopsy techniques. Br J Cancer. 2015;113:1565–70.
Kuerer HM, Vrancken Peeters M, Rea DW, Basik M, De Los Santos J, Heil J. Nonoperative management for invasive breast cancer after neoadjuvant systemic therapy: conceptual basis and fundamental international feasibility clinical trials. Ann Surg Oncol. 2017. https://doi.org/10.1245/s10434-017-5926-z.
Peintinger F, Kuerer HM, Anderson K, et al. Accuracy of the combination of mammography and sonography in predicting tumor response in breast cancer patients after neoadjuvant chemotherapy. Ann Surg Oncol. 2006;13:1443–9.
Adrada BE, Huo L, Lane DL, Arribas EM, Resetkova E, Yang W. Histopathologic correlation of residual mammographic microcalcifications after neoadjuvant chemotherapy for locally advanced breast cancer. Ann Surg Oncol. 2015;22:1111–7.
Kim YS, Chang JM, Moon HG, Lee J, Shin SU, Moon WK. Residual mammographic microcalcifications and enhancing lesions on MRI after neoadjuvant systemic chemotherapy for locally advanced breast cancer: correlation with histopathologic residual tumor size. Ann Surg Oncol. 2016;23:1135–42.
Feliciano Y, Mamtani A, Morrow M, Stempel MM, Patil S, Jochelson MS. Do calcifications seen on mammography after neoadjuvant chemotherapy for breast cancer always need to be excised? Ann Surg Oncol. 2017; 24:1492–8.
van la Parra RF, Kuerer HM. Selective elimination of breast cancer surgery in exceptional responders: historical perspective and current trials. Breast Cancer Res. 2016;18:28.
Acknowledgment
The authors thank Stephanie Deming for editing the paper.
Funding
This work was supported by the PH and Fay Etta Robinson Distinguished Professorship in Cancer Research (HMK) and a Cancer Center Support Grant from the National Institutes of Health (NIH) (CA16672).
Disclosure
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rauch, G.M., Kuerer, H.M., Adrada, B. et al. Biopsy Feasibility Trial for Breast Cancer Pathologic Complete Response Detection after Neoadjuvant Chemotherapy: Imaging Assessment and Correlation Endpoints. Ann Surg Oncol 25, 1953–1960 (2018). https://doi.org/10.1245/s10434-018-6481-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6481-y