Abstract
Background
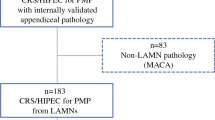
Low-grade appendiceal mucinous neoplasm (LAMN) is the most common primary lesion of pseudomyxoma peritonei, a disease whose standard treatment is cytoreduction and hyperthermic intraperitoneal chemotherapy. The optimal management of LAMN is not well defined. This study prospectively assessed a clinical surveillance strategy for LAMN with or without limited peritoneal spread.
Methods
During 2003–2017, the study prospectively enrolled 41 patients treated by macroscopically complete surgery for LAMN with or without limited peritoneal spread (pelvis and right lower quadrant). Follow-up assessment included thoracic-abdomino-pelvic computed tomography scan and serum tumor markers scheduled after surgery, then every 6 months for 5 years, and yearly thereafter. All specimens were reviewed by a dedicated pathologist.
Results
Appendectomy and five right colectomies were performed for 36 patients. Nine patients also underwent macroscopically complete cytoreduction of mucinous peritoneal disease, and four patients had hysterectomy plus bilateral salphingo-oophorectomy. Appendiceal rupture was evaluable in 38 of the 41 patients, being present in 21 patients (51.2%). Mucin, cells, or both outside the appendix were observed in 24 patients (58.5%). The median follow-up period was 58 months (range 9.3–162 months). The 5-year recurrence-free survival rate was 95.1%. Only two patients experienced peritoneal recurrences (4.9%), respectively 18 and 22 months after appendectomy. Their primary lesions were LAMNs with and without appendix wall rupture or extra-appendiceal mucin, respectively. No death occurred.
Conclusion
These findings strongly suggest that radically resected LAMN, even with limited peritoneal spread, carries a low recurrence risk. Furthermore, appendix wall perforation and the presence of mucin, cells, or both outside the appendix were not associated with a higher risk of metachronous peritoneal dissemination. In this setting, clinical and radiologic surveillance is a viable choice.


Similar content being viewed by others
Change history
19 January 2018
In the original article Massimo Milione’s last name was spelled incorrectly. It is correct as reflected here. The original article has also been updated.
19 January 2018
In the original article Massimo Milione?s last name was spelled incorrectly. It is correct as reflected here. The original article has also been updated.
19 January 2018
In the original article Massimo Milione?s last name was spelled incorrectly. It is correct as reflected here. The original article has also been updated.
References
Malya FU, Hasbahceci A, Sertr G, et al. Appendiceal mucocele: clinical and imaging features of 14 cases. Chirurgia Bucur. 2014;109:788–93.
Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7970 appendectomies. Dis Colon Rectum. 1998;41:75–80.
McCusker ME, Cote TR, Clegg LX, et al. Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology, and end-results program, 1973–1998. Cancer. 2002;94:3307–12.
Misdraji J, Yantiss RK, Graeme-Cook FM, et al. Appendiceal mucinous neoplasms: a clinicopathologic analysis of 107 cases. Am J Surg Pathol. 2003;27:1089–103.
Smeenk RM, van Velthuysen ML, Verwaal VJ, Zoetmulder FA. Appendiceal neoplasms and pseudomyxoma peritonei: a population-based study. Eur J Surg Oncol. 2008;34:196–201.
Fernandez RN, Daly GM. Pseudomyxoma peritonei. Arch Surg. 1980;115:409–14.
Gough DB, Donohue JH, Schutt AJ, et al. Pseudomyxoma peritonei: long-term patient survival with an aggressive regional approach. Ann Surg. 1994;219:112–9.
Miner TJ, Shia J, Jaques DP, et al. Long-term survival following treatment of pseudomyxoma peritonei: an analysis of surgical therapy. Ann Surg. 2005;241:300–8.
Järvinen P, Järvinen HJ, Lepistö A. Survival of patients with pseudomyxoma peritonei treated by serial debulking. Colorectal Dis. 2010;12:868–72.
Chua TC, Moran BJ, Sugarbaker PH, et al. Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Clin Oncol. 2012;30:2449–56.
Moran B, Baratti D, Yan TD, et al. Consensus statement on the locoregional treatment of appendiceal mucinous neoplasms with peritoneal dissemination (pseudomyxoma peritonei). J Surg Oncol. 2008;98:277–82.
Sugarbaker PH. New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome? Lancet Oncol. 2006;7:69–76.
Baratti D, Kusamura S, Nonaka D, Cabras AD, Laterza B, Deraco M. Pseudomyxoma peritonei: biological features are the dominant prognostic determinants after complete cytoreduction and hyperthermic intraperitoneal chemotherapy. Ann Surg. 2009;249:243–9.
Ansari N, Chandrakumaran K, Dayal S, Mohamed F, Cecil TD, Moran BJ. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in 1000 patients with perforated appendiceal epithelial tumours. Eur J Surg Oncol. 2016;42:1035–41.
Murphy EMA, Farquharson SM, Moran BJ. Management of an unexpected appendiceal neoplasm. Br J Surg. 2006;93:783–92.
Barrios P, Losa F, Gonzalez-Moreno S. Rojo A, Go´mez-Portilla A, Bretcha-Boix P, et al. Recommendations in the management of epithelial appendiceal neoplasms and peritoneal dissemination from mucinous tumours (pseudomyxoma peritonei). Clin Transl Oncol. 2016;18:437–48.
Gonzalez-Moreno S, Sugarbaker PH. Right hemicolectomy does not confer a survival advantage in patients with mucinous carcinoma of the appendix and peritoneal seeding. Br J Surg. 2004;91:304–11.
McDonald JR, O’Dwyer ST, Rout S, et al. Classification of and cytoreductive surgery for low-grade appendiceal mucinous neoplasms. Br J Surg. 2012;99:987–9.
Foster JM, Sleightholm RL, Wahlmeier S, Loggie B, Sharma P, Patel A. Early identification of DPAM in at-risk low-grade appendiceal mucinous neoplasm patients: a new approach to surveillance for peritoneal metastasis. World J Surg Oncol. 2016;14:243.
Fournier K, Rafeeq S, Taggart M, et al. Low-grade appendiceal mucin mucinous neoplasm of uncertain malignant potential (LAMN-UMP): prognostic factors and implications for treatment and follow-up. Ann Surg Oncol. 2017;24:187–93.
Pai RK, Beck AH, Norton JA, Longacre TA. Appendiceal mucinous neoplasms: clinicopathologic study of 116 cases with analysis of factors predicting recurrence. Am J Surg Pathol. 2009;33:1425–39.
Young RH. Pseudomyxoma peritonei and selected other aspects of the spread of appendiceal neoplasms. Semin Diagn Pathol. 2004;21:134–50.
Panarelli NC, Yantiss RK. Mucinous neoplasms of the appendix and peritoneum. Arch Pathol Lab Med. 2011;135:1261–8.
Baratti D, Kusamura S, Milione M, et al. Pseudomyxoma peritonei of extra-appendiceal origin: a comparative study. Ann Surg Oncol. 2016;23:4222–30.
Carr NJ, Sobin LH. Adenocarcinoma of the appendix. In: Bosman F, Carneiro F, Hruban R, Theise N (ed). WHO classification of tumours of the digestive system. International Agency for Research on Cancer, Lyon, 2010, pp 122–25.
Carr NJ, Cecil TD, Mohamed F, et al. A consensus for classification and pathologic reporting of pseudomyxoma peritonei and associated appendiceal neoplasia: the results of the Peritoneal Surface Oncology Group International (PSOGI) modified Delphi process. Am J Surg Pathol. 2016;40:14–26.
Carr NJ, Bibeau F, Bradley RF, et al. The histopathological classification, diagnosis, and differential diagnosis of mucinous appendiceal neoplasms, appendiceal adenocarcinomas, and pseudomyxoma peritonei. Histopathology. 2017;71:847–58.
Smeenk RM, van Velthuysen ML, Verwaal VJ, Zoetmulder FA. Appendiceal neoplasms and pseudomyxoma peritonei: a population-based study. Eur J Surg Oncol. 2008;34:196–201.
Baratti D, Kusamura S, Iusco D, et al. Hyperthermic intraperitoneal chemotherapy (HIPEC) at the time of primary curative surgery in patients with colorectal cancer at high risk for metachronous peritoneal metastases. Ann Surg Oncol. 2017;24:167–75.
Arnason T, Kamionek M, Yang M, et al. Significance of proximal margin involvement in low-grade appendiceal mucinous neoplasms. Arch Pathol Lab Med. 2015;139:518–21.
Yantiss RK, Shia J, Klimstra DS, Hahn HP, Odze RD, Misdraji J. Prognostic significance of localized extra-appendiceal mucin deposition in appendiceal mucinous neoplasms. Am J Surg Pathol. 2009;33:248–55.
Acknowledgement
The study was partially supported by a grant of the Italian Association for Cancer Research (AIRC). Snita Sinukumar is a fellow of the European School of Peritoneal Surface Oncology (ESPSO).
Disclosure
The authors have no conflicts of interest or financial disclosures to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original version of this article was revised: Massimo Milione’s last name was spelled incorrectly.
Rights and permissions
About this article
Cite this article
Guaglio, M., Sinukumar, S., Kusamura, S. et al. Clinical Surveillance After Macroscopically Complete Surgery for Low-Grade Appendiceal Mucinous Neoplasms (LAMN) with or Without Limited Peritoneal Spread: Long-Term Results in a Prospective Series. Ann Surg Oncol 25, 878–884 (2018). https://doi.org/10.1245/s10434-017-6305-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6305-5