Abstract
Background
Autologous breast reconstruction offers excellent long term outcomes after mastectomy. However, maintaining adequate postoperative analgesia remains challenging. Use of paravertebral blocks (PVBs) reduces postoperative narcotic use and length of stay, and enhanced recovery protocols with mixed analgesia methods are gaining popularity, but few studies have explored the intraoperative effects of these interventions.
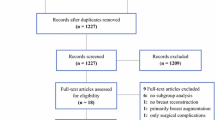
Methods
Patients who underwent abdominally based autologous breast reconstruction between 2010 and 2016 were compiled into a retrospective database. We used electronic medical records to determine demographics, as well as perioperative and intraoperative vital signs and narcotic, anxiolytic, crystalloid, colloid, blood product, and vasopressor requirements, and postoperative complications. Results were compared between patients who had a PVB and those who did not and those who had a PVB alone and those who followed our enhanced recovery protocol using standard statistical methods and adjusting for preoperative values.
Results
A total of 170 patients were included in the study. Sixty-six had a PVB, and 104 did not. Of the 66 who had a PVB, 19 followed our enhanced recovery protocol. Patients who did not have a PVB required 171.6 mg of total narcotic medication in the perioperative period, those with a PVB alone required 146.9 mg, and those who followed the ERAS protocol 95.2 mg (p = 0.01). There was no difference in intraoperative mean arterial pressure, time with mean arterial pressure <80% of baseline, vasopressor use, or fluid requirement. There was no difference in complication rate.
Conclusions
PVBs and an enhanced recovery protocol reduce the use of narcotic medications in autologous breast reconstruction without impacting intraoperative hemodynamics. Breast reconstruction after mastectomy restores body image and improves health-related quality of life, satisfaction with appearance and physical, psychosocial, and sexual well-being (Donovan et al. in J Clin Oncol 7(7):959–968, 1989; Eltahir et al. in Plast Reconstr Surg 132(2):201e–209e, 2013; Jagsi et al. in Ann Surg 261(6):1198–1206, 2015). For patients pursuing breast reconstruction, there are two major options: prosthetic (tissue expander/implant) or autologous reconstruction. However, while providing exceptional long-term outcomes, postoperative pain and length of hospital stay remains a major challenge preventing more widespread adoption of autologous breast reconstruction (Albornoz et al. in Plast Reconstr Surg 131(1):15–23, 2013; Gurunluoglu et al. in Ann Plast Surg 70(1):103–110, 2013; Kulkarni et al. in Plast Reconstr Surg 132(3):534–541, 2013; Sbitany et al. in Plast Reconstr Surg 124(6):1781–1789, 2009). Acute postoperative pain contributes to prolonged hospital stays, increased narcotic use, and associated risks of the aforementioned.
Similar content being viewed by others
References
Donovan K, Sanson-Fisher RW, Redman S. Measuring quality of life in cancer patients. J Clin Oncol. 1989;7(7):959–68.
Eltahir Y, Werners LL, Dreise MM, et al. Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plast Reconstr Surg. 2013;132(2):201e–9e.
Jagsi R, Li Y, Morrow M, et al. Patient-reported quality of life and satisfaction with cosmetic outcomes after breast conservation and mastectomy with and without reconstruction: results of a survey of breast cancer survivors. Ann Surg. 2015;261(6):1198–206.
Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131(1):15–23.
Gurunluoglu R, Gurunluoglu A, Williams SA, Tebockhorst S. Current trends in breast reconstruction: survey of American Society of Plastic Surgeons 2010. Ann Plast Surg. 2013;70(1):103–10.
Kulkarni AR, Sears ED, Atisha DM, Alderman AK. Use of autologous and microsurgical breast reconstruction by U.S. plastic surgeons. Plast Reconstr Surg. 2013;132(3):534–41.
Sbitany H, Amalfi AN, Langstein HN. Preferences in choosing between breast reconstruction options: a survey of female plastic surgeons. Plast Reconstr Surg. 2009;124(6):1781–9.
Rwjf. Deaths from injuries up significantly over past four years in 17 states. 2015-06-17, 2015.
Oderda GM, Said Q, Evans RS, et al. Opioid-related adverse drug events in surgical hospitalizations: impact on costs and length of stay. Ann Pharmacother. 2007;41(3):400–6.
Parikh RP, Sharma K, Guffey R, Myckatyn TM. Preoperative paravertebral block improves postoperative pain control and reduces hospital length of stay in patients undergoing autologous breast reconstruction after mastectomy for breast cancer. Ann Surg Oncol. 2016;23(13):4262–9.
Coopey SB, Specht MC, Warren L, Smith BL, Winograd JM, Fleischmann K. Use of preoperative paravertebral block decreases length of stay in patients undergoing mastectomy plus immediate reconstruction. Ann Surg Oncol. 2013;20(4):1282–6.
Andreae MH, Andreae DA. Regional anaesthesia to prevent chronic pain after surgery: a Cochrane systematic review and meta-analysis. Br J Anaesth. 2013;111(5):711–20.
Coveney E, Weltz CR, Greengrass R, et al. Use of paravertebral block anesthesia in the surgical management of breast cancer: experience in 156 cases. Ann Surg. 1998;227(4):496–501.
Fahy AS, Jakub JW, Dy BM, et al. Paravertebral blocks in patients undergoing mastectomy with or without immediate reconstruction provides improved pain control and decreased postoperative nausea and vomiting. Ann Surg Oncol. 2014;21(10):3284–9.
Shah A, Rowlands M, Krishnan N, Patel A, Ott-Young A. Thoracic intercostal nerve blocks reduce opioid consumption and length of stay in patients undergoing implant-based breast reconstruction. Plast Reconstr Surg. 2015;136(5):584e–91e.
Abdelsattar JM, Boughey JC, Fahy AS, et al. Comparative study of liposomal bupivacaine versus paravertebral block for pain control following mastectomy with immediate tissue expander reconstruction. Ann Surg Oncol. 2016;23(2):465–70.
Wolf O, Clemens MW, Purugganan RV, et al. A prospective, randomized, controlled trial of paravertebral block versus general anesthesia alone for prosthetic breast reconstruction. Plast Reconstr Surg. 2016;137(4):660e–6e.
Booi DI. Perioperative fluid overload increases anastomosis thrombosis in the free TRAM flap used for breast reconstruction. Eur J Plast Surg. 2011;34(2):81–6.
Nelson JA, Fischer JP, Grover R, et al. Intraoperative perfusion management impacts postoperative outcomes: an analysis of 682 autologous breast reconstruction patients. J Plast Reconstr Aesthet Surg. 2015;68(2):175–83.
Richardson J, Lonnqvist PA, Naja Z. Bilateral thoracic paravertebral block: potential and practice. Br J Anaesth. 2011;106(2):164–71.
Okitsu K, Iritakenishi T, Iwasaki M, Imada T, Kamibayashi T, Fujino Y. Paravertebral block decreases opioid administration without causing hypotension during transapical transcatheter aortic valve implantation. Heart Vessels. 2016;31(9):1484–90.
Batdorf NJ, Lemaine V, Lovely JK, et al. Enhanced recovery after surgery in microvascular breast reconstruction. J Plast Reconstr Aesthet Surg. 2015;68(3):395–402.
Gnaneswaran N, Perera M, Perera N, Peters M. Enhanced recovery after surgery (ERAS) pathways in autologous breast reconstruction: a systematic review. Eur J Plast Surg. 2016;39(3):165–72.
Salgado CJ, Chim H, Schoenoff S, Mardini S. Postoperative care and monitoring of the reconstructed head and neck patient. Sem Plast Surg. 2010;24(3):281–7.
Weltz CR, Greengrass RA, Lyerly HK. Ambulatory surgical management of breast carcinoma using paravertebral block. Ann Surg. 1995;222(1):19–26.
Pusch F, Freitag H, Weinstabl C, Obwegeser R, Huber E, Wildling E. Single-injection paravertebral block compared to general anaesthesia in breast surgery. Acta Anaesthesiol Scand. 1999;43(7):770–4.
Naja Z, Lönnqvist PA. Somatic paravertebral nerve blockade: incidence of failed block and complications. Anaesthesia. 2001;56(12):1181–201.
Lonnqvist PA, MacKenzie J, Soni AK, Conacher ID. Paravertebral blockade. Failure rate and complications. Anaesthesia. 1995;50(9):813–5.
Karmakar MK. Thoracic paravertebral block. Anesthesiology. 2001;95(3):771–80.
Naja ZM, El-Rajab M, Al-Tannir MA, et al. Thoracic paravertebral block: influence of the number of injections. Reg Anesth Pain Med. 2006;31(3):196–201.
Hagau N, Longrois D. Anesthesia for free vascularized tissue transfer. Microsurgery. 2009;29(2):161–7.
Chen C, Nguyen MD, Bar-Meir E, et al. Effects of vasopressor administration on the outcomes of microsurgical breast reconstruction. Ann Plast Surg. 2010;65(1):28–31.
Brandstrup B, Tonnesen H, Beier-Holgersen R, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003;238(5):641–8.
Kelly DA, Reynolds M, Crantford C, Pestana IA. Impact of intraoperative vasopressor use in free tissue transfer for head, neck, and extremity reconstruction. Ann Plast Surg. 2014;72(6):S135–8.
Cordeiro PG, Santamaria E, Hu QY, Heerdt P. Effects of vasoactive medications on the blood flow of island musculocutaneous flaps in swine. Ann Plast Surg. 1997;39(5):524–31.
Disclosures
This research was supported by T32CA190194 (PI: Colditz, funding for EO) and by the Foundation for Barnes-Jewish Hospital and by Siteman Cancer Center. The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH. Other authors have no financial disclosures or conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Odom, E.B., Mehta, N., Parikh, R.P. et al. Paravertebral Blocks Reduce Narcotic Use Without Affecting Perfusion in Patients Undergoing Autologous Breast Reconstruction. Ann Surg Oncol 24, 3180–3187 (2017). https://doi.org/10.1245/s10434-017-6007-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6007-z