Abstract
Purpose
The aim of this study was to investigate the relationship between same-day discharge (SDD) and postoperative complications within 30 days of laparoscopic hysterectomy for endometrial cancer and endometrial intraepithelial neoplasia (EIN).
Methods
This single-institution retrospective cohort included all patients who underwent conventional and robotic-assisted laparoscopic hysterectomy for endometrial cancer or EIN in a large teaching hospital between 2011 and 2013. Temporal trends in frequency of SDD and rates of postoperative complications were investigated to assess whether adoption of routine SDD was associated with increased postoperative complications. Associations between SDD and postoperative complications were also investigated in univariate and multivariate models.
Results
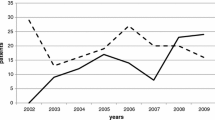
Overall, 696 patients underwent laparoscopic hysterectomy. Of these, 37.1 % had pelvic lymphadenectomy, 3.0 % had para-aortic lymphadenectomy, and 9.3 % underwent omentectomy. The rate of SDD increased from 3.9 to 69.6 % during the study period (p < 0.001), and the frequency of postoperative readmission, unscheduled surgery, infection, and composite complications within 30 days of hysterectomy did not differ during the study period. The composite complication rate did not differ significantly between patients who underwent surgery before and after the adoption of routine SDD (rate ratio 0.7, 95 % CI 0.4–1.2, p = 0.24). After controlling for demographic, intraoperative, and comorbid factors, patients who underwent SDD were not at increased risk for postoperative complications.
Conclusions
Adoption of routine SDD after laparoscopic surgery for endometrial cancer and EIN did not result in increased complication rates within our institution. A larger prospective study is required to definitively establish the safety of this approach.

Similar content being viewed by others
References
Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, et al. (editors). SEER cancer statistics review, 1975–2011. National Cancer Institute: Bethesda (MD). Available at: http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.
Ries LAG, Young JL, Keel GE, Eisner MP, Lin YD, Horner M-J (editors). SEER survival monograph: cancer survival among adults: US SEER Program, 1988–2001, patient and tumor characteristics. NIH Pub. No. 07-6215. Bethesda (MD): National Cancer Institute, SEER Program. 2007.
Wright JD, Barrena Medel NI, Sehouli J, Fujiwara K, Herzog TJ. Contemporary management of endometrial cancer. Lancet. 2012;379:1352–60.
Mariani A, Webb MJ, Keeney GL, Haddock MG, Calori G, Podratz KC. Low-risk corpus cancer: is lymphadenectomy or radiotherapy necessary? Am J Obstet Gynecol. 2000;182:1506–19.
Greer BE, Koh WJ, Abu-Rustum N, Bookman MA, Bristow RE, Campos SM, et al. Uterine neoplasms. Clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2009;7:498–531.
Vargas R, Rauh-Hain JA, Clemmer J, Clark RM, Goodman A, Growdon WB, et al. Tumor size, depth of invasion, and histologic grade as prognostic factors of lymph node involvement in endometrial cancer: a SEER analysis. Gynecol Oncol. 2014;133:216–20.
Management of endometrial cancer. ACOG Practice Bulletin No. 65. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2005;106:413–25.
Mutter GL, Kauderer J, Baak JP, Alberts D. Biopsy histomorphometry predicts uterine myoinvasion by endometrial carcinoma: a Gynecologic Oncology Group study. Hum Pathol. 2008;39:866–74.
Galaal K, Bryant A, Fisher AD, Al-Khaduri M, Kew F, Lopes AD. Laparoscopy versus laparotomy for the management of early stage endometrial cancer. Cochrane Database Syst Rev. 2012;(9):CD006655.
Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009;(3):CD003677.
Zullo F, Falbo A, Palomba S. Safety of laparoscopy vs laparotomy in the surgical staging of endometrial cancer: a systematic review and metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2012;207:94–100.
Walker JL, Piedmonte MR, Spirtos NM, Eisenkop SM, Schlaerth JB, Mannel RS, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer. Gynecologic Oncology Group Study LAP2. J Clin Oncol. 2009;27:5331–36.
Walker JL, Piedmonte MR, Spirtos NM, Eisenkop SM, Schlaerth JB, Mannel RS, et al. Recurrence and survival after random assignment to laparoscopy versus laparotomy for comprehensive surgical staging of uterine cancer. Gynecologic Oncology Group LAP2 Study. J Clin Oncol. 2012;30:695–700.
Zullo F, Palomba S, Falbo A, Russo T, Mocciaro R, Tartaglia E, et al. Laparoscopic surgery vs laparotomy for early stage endometrial cancer: long-term data of a randomized controlled trial. Am J Obstet Gynecol. 2009;200:296.e1–e9.
Malzoni M, Tinelli R, Cosentino F, Perone C, Rasile M, Iuzzolino D, et al. Total laparoscopic hysterectomy versus abdominal hysterectomy with lymphadenectomy for early-stage endometrial cancer: a prospective randomized study. Gynecol Oncol. 2009;112:126–33.
Schiavone MB, Herzog TJ, Ananth CV, Wilde ET, Lewin SN, Burke WM, et al. Feasibility and economic impact of same day discharge for women who undergo laparoscopic hysterectomy. Am J Obstet Gynecol. 2012;207:382.e1–e9.
Khavanin N, Mlodinow A, Milad MP, Bilimoria KY, Kim JY. Comparison of perioperative outcomes in outpatient and inpatient laparoscopic hysterectomy. J Minim Invasive Gynecol. 2013;20:604–10.
Perron-Burdick M, Yamamoto M, Zaritsky E. Same day discharge after laparoscopic hysterectomy. Obstet Gynecol. 2011;117:1136–41.
Rettenmaier MA, Mendivil AA, Brown JV 3rd, Abaid LN, Micha JP, Goldstein BH. Same day discharge in clinical stage I endometrial cancer patients treated with total laparoscopic hysterectomy, bilateral salpingo-oophorectomy and bilateral pelvic lymphadenectomy. Oncology. 2012;82:321–26.
Gien LT, Kupets R, Covens A. Feasibility of same day discharge after laparoscopic surgery in gynecologic oncology. Gynecol Oncol. 2011;121:339–43.
Penner KR, Fleming ND, Barlavi L, Axtell AE, Lentz SE. Same-day discharge is feasible and safe in patients undergoing minimally invasive staging for gynecologic malignancies. Am J Obstet Gynecol. 2015;212:186.e1–8.
Lee SJ, Calderon B, Gardner GJ, Mays A, Nolans S, Sonoda Y, et al. The feasibility and safety of same day discharge after robotic assisted hysterectomy alone or with other procedures for benign and malignant indications. Gynecol Oncol. 2014;133:552–55.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Mathis MR, Naughton NN, Shanks AM, et al. Patient selection for day case-eligible surgery: identifying those at high risk for major complications. Anesthesiology. 2013;119:1310–21.
Whippey A, Kostandoff G, Paul J, Ma J, Thabane L, Ma HK. Predictors of unanticipated admission following ambulatory surgery: a retrospective case-control study. Can J Anaesth. 2013;60:675–83.
Joshi GP, Ahmad S, Riad W, Eckert S, Chung F. Selection of patients with obesity undergoing ambulatory surgery: a systematic review of the literature. Anesth Analg. 2013;117:1082–91.
Joshi GP, Ankichetty S, Chung F, Gan TJ. Society for Ambulatory Anesthesia consensus statement on preoperative selection of patients with obstructive sleep apnea scheduled for ambulatory surgery. Anesth Analg. 2012;115:1060–68.
Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970;49:924–34.
Ead H. From Aldrete to PADSS: reviewing discharge criteria after ambulatory surgery. J Perianesth Nurs. 2006;21:259–67.
Sarin P, Philip BK, Mitani A, Eappen S, Urman RD. Specialized ambulatory anesthesia teams contribute to decreased ambulatory surgery recovery room length of stay. Ochsner J. 2012;12:94–100.
Gan TJ, Diemunsch P, Habib AS, Kovac A, Kranke P, Meyer TA, et al.; Society for Ambulatory Anesthesia. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118:85–113.
Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6.
Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200.
Walker AM. Confounding by indication. Epidemiology. 1996;7:335–6.
Milam MR, Java J, Walker JL, Metzinger DS, Parker LP, Coleman RL; Gynecologic Oncology Group. Nodal metastasis risk in endometrioid endometrial cancer. Obstet Gynecol. 2012;119:286–92.
Mariani A, Dowdy SC, Cliby WA, Gostout BS, Jones MB, Wilson TO, et al. Prospective assessment of lymphatic dissemination in endometrial cancer: a paradigm shift in surgical staging. Gynecol Oncol. 2008;109:11–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Melamed, A., Katz Eriksen, J.L., Hinchcliff, E.M. et al. Same-Day Discharge After Laparoscopic Hysterectomy for Endometrial Cancer. Ann Surg Oncol 23, 178–185 (2016). https://doi.org/10.1245/s10434-015-4582-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4582-4