Abstract
Background
Gaps in breast cancer (BC) surgical care have been identified. We have completed a surgeon-directed, iterative project to improve the quality of BC surgery in South-Central Ontario.
Methods
Surgeons performing BC surgery in a single Ontario health region were invited to participate. Interventions included: audit and feedback (A&F) of surgeon-selected quality indicators (QIs), workshops, and tailoring interviews. Workshops and A&F occurred yearly from 2005–2012. QIs included: preoperative imaging; preoperative core biopsy; positive margin rates; specimen orientation labeling; intraoperative specimen radiography of nonpalpable lesions; T1/T2 mastectomy rates; reoperation for positive margins; sentinel lymph node biopsy (SLNB) rates, number of sentinel lymph nodes; and days to receive pathology report. Semistructured tailoring interviews were conducted to identify facilitators and barriers to improved quality. All results were disseminated to all surgeons performing breast surgery in the study region.
Results
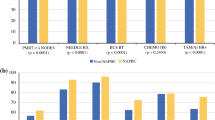
Over 6 time periods, 1,828 BC charts were reviewed from 12 hospitals (8 community and 4 academic). Twenty-two to 40 participants attended each workshop. Sustained improvement in rates of positive margins, preoperative core biopsies, specimen orientation labeling, and SLNB were seen. Mastectomy rates and overall axillary staging rates did not change, whereas time to receive pathology report increased. The tailoring interviews concerning positive margins, SLNB, and reoperation for positive margins identified facilitators and barriers relevant to surgeons.
Conclusions
This surgeon-directed, regional project resulted in meaningful improvement in numerous QIs. There was consistent and sustained participation by surgeons, highlighting the importance of integrating the clinicians in a long-term, iterative quality improvement strategy in BC surgery.



Similar content being viewed by others
References
Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington: National Academy Press; 2001.
McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–45.
Grimshaw JM, Shirran L, Thomas R, et al. Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001;39(8 Suppl 2):II2–45.
Grimshaw JM, Thomas RE, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8(6):iii–iv, 1–72.
Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? J Cont Educ Health Prof. 2006;26:13–24.
Landercasper J, Ellis RL, Mathiason MA, et al. A community breast cancer report card determined by participation in the national quality measures for breast centers program. Breast J. 2010;16:472–80.
Birkmeyer JD, Dimick JB, Birkmeyer NJ. Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg. 2004;198:626–32.
Ko CY, Maggard M, Austin N. Quality in surgery: current issues for the future. World J Surg. 2005;29(10):1204–9.
Maggard MA, McGorgy ML, Ko CY et al. Development of quality indicators: lessons learned in bariatric surgery. Am Surg. 2006;72:870–4.
Kaufman CA, Landercasper J. Can we measure the quality of breast surgical care? Ann Surg Oncol. 2011;18:3053–60.
American Society of Breast Surgeons Mastery Program. www.breast.surgeons.org/mastery/ (2011). Accessed 20 Sept 2013.
National Quality Measure for Breast Centers. www.nqmbc.org/ (2011). Accessed 20 Sept 2013.
National Accreditation Program for Breast Centers. www.accreditedbreastcenters.org/ (2011). Accessed 6 Nov 2012.
Clifford EJ, De vol EB, Pockaj BA, et al. Early results from a novel quality outcomes program: the American society of breast surgeons’ mastery of breast surgery. Ann Surg Oncol. 2010;17:S233–41.
Olaya W, Bae W, Wong J, et al. Are percutaneous biopsy rates a reasonable quality measure in breast cancer management. Ann Surg Oncol. 2010;17:S268–72.
Kao LS, Lally KP, Thoma EJ, et al. Improving quality improvement: a methodologic framework for evaluating effectiveness of surgical quality improvement. J Am Coll Surg. 2009;208:621–6.
Simunovic M, Baxter NN. Knowledge translation research: a review and new concepts from a surgical case study. Surgery. 2009;145:639–44.
Jamtvedt G, Young JM, Kristoffersen DT, et al. Does telling people what they have been doing change what they do? A systematic review of the effects of audit and feedback. Qual Saf Health Care. 2006;15:433–6.
Grimshaw J, Eccles M, Walter A, et al. Changing physician’s behaviour; what works and thoughts on getting more things to work. J Cont Educ Health Prof. 2002;22:237–43.
Doumit G, Gattellari M, Grimshaw J, et al. Local opinion leaders: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007;(1):CD000125.
O’Brien MA, Freemantle N, Oxman AD, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2001;(2):CD003030.
O’Brien MA, Oxman AD, Davis DA, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007;(2):CD000409.
Breslin TM, Caughran J, Pettinga J, et al. Improving breast cancer care through a regional quality collaborative. Surgery. 2011;150:635–42.
Clarke-Pearson EM, Jacobson AF, Boolbol SK, et al. Quality assurance initiative at one institution for minimally invasive breast biopsy as the initial diagnostic technique. J Am Coll Surg. 2009;208:75–8.
Veerbeek L, van der Geest L, Wouters M, et al. Enhancing the quality of care for patients with breast cancer: Seven years of experience with a Dutch auditing system. EJSO. 2011;37:714–8.
Guadagnoli E, Soumerai S, Gurwitz JH, et al. Improving discussion of surgical treatment options for patients with breast cancer: local medical opinion leaders versus audit and performance feedback. Breast Cancer Res Treat. 2000;61:171–5.
Lovrics PJ, Hodgson N, O’Brien MA, et al. The implementation of a surgeon-directed quality improvement strategy in breast cancer surgery. Am J Surg. 2013 Nov 8. [Epub ahead of print].
Lovrics PJ, Cornacchi SD, Farrokhyar F, et al. The relationship between surgical factors and margin status after breast conservation surgery for early stage breast cancer. Am J Surg. 2009;197:740–6.
Hanley C, Kessaram R. Quality of diagnosis and surgical management of breast lesions in a community hospital: room for improvement? Can J Surg. 2006;49:185–92.
Cheater F, Baker R, Gillies C, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2005;(3):CD005470.
Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Chicago: Aldine; 1967.
Charmaz K. Constructing grounded theory. A practical guide through qualitative analysis. Thousand Oaks: Sage Publications; 2006.
Wheeler DJ, Chambers DS. Understanding statistical process control, 2nd edn. Knoxville: SPC Press; 1992.
Williams PM. Techniques for root cause analysis. BUMC Proc. 2001;14:154–7.
Acknowledgment
Funding was provided by grants from the McMaster Surgical Associates and the Canadian Breast Cancer Foundation: Ontario Chapter. Initial planning workshops were supported by funding from the Juravinski Cancer Centre. Mary Ann O’Brien was supported by Postdoctoral Fellowships from the Canadian Breast Cancer Foundation and Psychosocial Oncology Research Training Program. The funding sources played no role in the design, conduct, or reporting of this study. The authors thank Dana Reeson, Michele Marcinow, Amanda Ramsaroop, Lianne Lindsay, Tiffaney Kittmer, and Dyda Dao for assistance with data collection and management. They also thank Ji Cheng for assistance with calculating process control charts.
Disclosure
All authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lovrics, P., Hodgson, N., O’Brien, M.A. et al. Results of a Surgeon-Directed Quality Improvement Project on Breast Cancer Surgery Outcomes in South-Central Ontario. Ann Surg Oncol 21, 2181–2187 (2014). https://doi.org/10.1245/s10434-014-3592-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3592-y