Abstract
Background
Pathologic response to preoperative chemotherapy for colorectal liver metastases (CLM) is associated with survival after hepatectomy. Histologically, dominant response patterns include fibrosis, necrosis and/or acellular mucin, but some of these changes can appear without previous chemotherapy and their individual correlation with outcome is unknown.
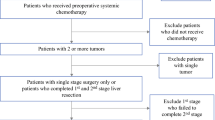
Methods
Pathology slides from patients who underwent CLM resection (irrespective of preoperative chemotherapy status) were rereviewed by a blinded pathologist. Pathologic response was recorded as the summation of percentage necrosis, fibrosis and acellular mucin. Associations between pathologic response, its components, preoperative chemotherapy, and survival were analyzed.
Results
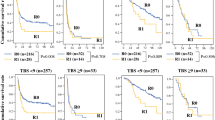
Pathology slides were rereviewed in 366 patients undergoing CLM resection from 2003 to 2007. Preoperative chemotherapy was administered in 249 (68 %) patients, who, when compared to no preoperative chemotherapy patients, had higher rates of overall pathologic response (57 vs. 46 %, P < .01), fibrosis (21 vs. 12 %, P < .01) and acellular mucin (6 vs. 3 %, P = .05) but similar rates of necrosis (30 vs. 31 %, P = .30). In patients receiving preoperative chemotherapy, overall pathologic response ≥75 % (5 year, 83 vs. 47 %, P < .01) and fibrosis ≥40 % (5 year, 87 vs. 51 %, P < .01) independently correlated with disease-specific survival after hepatectomy. Preoperative hepatic artery infusion chemotherapy (P = .04) and bevacizumab (P = .05) were marginally associated with overall pathologic response and fibrosis, respectively.
Conclusions
Fibrosis is the predominant chemotherapy-related pathologic alteration driving the association of treatment response with survival after CLM resection. Necrosis in CLM is not related to chemotherapy or outcome.



Similar content being viewed by others
References
Nordlinger B, Sorbye H, Glimelius B, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008;371:1007–16.
Adam R, Delvart V, Pascal G, et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg. 2004;240:644–57.
Alberts SR, Horvath WL, Sternfeld WC, et al. Oxaliplatin, fluorouracil, and leucovorin for patients with unresectable liver-only metastases from colorectal cancer: a North Central Cancer Treatment Group phase II study. J Clin Oncol. 2005;23:9243–9.
Kemeny NE, Melendez FD, Capanu M, et al. Conversion to resectability using hepatic artery infusion plus systemic chemotherapy for the treatment of unresectable liver metastases from colorectal carcinoma. J Clin Oncol. 2009;27:3465–71.
Adam R, Wicherts DA, de Haas RJ, et al. Complete pathologic response after preoperative chemotherapy for colorectal liver metastases: myth or reality? J Clin Oncol. 2008;26:1635–41.
Blazer DG III, Kishi Y, Maru DM, et al. Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol. 2008;26:5344–51.
Rubbia-Brandt L, Giostra E, Brezault C, et al. Importance of histological tumor response assessment in predicting the outcome in patients with colorectal liver metastases treated with neo-adjuvant chemotherapy followed by liver surgery. Ann Oncol. 2007;18:299–304.
Compton CC. Key issues in reporting common cancer specimens: problems in pathologic staging of colon cancer. Arch Pathol Lab Med. 2006;130:318–24.
Shia J, Guillem JG, Moore HG, et al. Patterns of morphologic alteration in residual rectal carcinoma following preoperative chemoradiation and their association with long-term outcome. Am J Surg Pathol. 2004;28:215–23.
Shia J, McManus M, Guillem JG, et al. Significance of acellular mucin pools in rectal carcinoma after neoadjuvant chemoradiotherapy. Am J Surg Pathol. 2011;35:127–34.
Washington MK, Berlin J, Branton P, et al. Protocol for the examination of specimens from patients with primary carcinoma of the colon and rectum. Arch Pathol Lab Med. 2009;133:1539–51.
Rullier A, Laurent C, Vendrely V, et al. Impact of colloid response on survival after preoperative radiotherapy in locally advanced rectal carcinoma. Am J Surg Pathol. 2005;29:602–6.
Ng JK, Urbanski SJ, Mangat N, et al. Colorectal liver metastases contract centripetally with a response to chemotherapy: a histomorphologic study. Cancer. 2008;112:362–71.
Znajda TL, Hayashi S, Horton PJ, et al. Postchemotherapy characteristics of hepatic colorectal metastases: remnants of uncertain malignant potential. J Gastrointest Surg. 2006;10:483–9.
Mandard AM, Dalibard F, Mandard JC, et al. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer. 1994;73:2680–6.
Benoist S, Brouquet A, Penna C, et al. Complete response of colorectal liver metastases after chemotherapy: does it mean cure? J Clin Oncol. 2006;24:3939–45.
Auer RC, White RR, Kemeny NE, et al. Predictors of a true complete response among disappearing liver metastases from colorectal cancer after chemotherapy. Cancer. 2010;116:1502–9.
Klinger M, Tamandl D, Eipeldauer S, et al. Bevacizumab improves pathological response of colorectal cancer liver metastases treated with XELOX/FOLFOX. Ann Surg Oncol. 2010;17:2059–65.
Ribero D, Wang H, Donadon M, et al. Bevacizumab improves pathologic response and protects against hepatic injury in patients treated with oxaliplatin-based chemotherapy for colorectal liver metastases. Cancer. 2007;110:2761–7.
White RR, Schwartz LH, Munoz JA, et al. Assessing the optimal duration of chemotherapy in patients with colorectal liver metastases. J Surg Oncol. 2008;97:601–4.
Kishi Y, Zorzi D, Contreras CM, et al. Extended preoperative chemotherapy does not improve pathologic response and increases postoperative liver insufficiency after hepatic resection for colorectal liver metastases. Ann Surg Oncol. 2010;17:2870–6.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
The first two authors contributed equally to this work.
Rights and permissions
About this article
Cite this article
Poultsides, G.A., Bao, F., Servais, E.L. et al. Pathologic Response to Preoperative Chemotherapy in Colorectal Liver Metastases: Fibrosis, not Necrosis, Predicts Outcome. Ann Surg Oncol 19, 2797–2804 (2012). https://doi.org/10.1245/s10434-012-2335-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-012-2335-1