Abstract
Background
Although subclinical cervical lymph node (LN) metastases in papillary thyroid carcinoma (PTC) are common, the efficacy of prophylactic central LN dissection (CLND) is unclear. Few prospective studies have assessed the relationships between complete pathologic information regarding tumors and metastatic nodes in the central compartment. We therefore investigated the pattern and predictive indicators of central LN metastasis, morbidity, and recurrence in patients who underwent total thyroidectomy and prophylactic CLND for unilateral PTC and clinically node-negative neck (cN0) disease.
Methods
This prospective study involved 184 patients with previously untreated unilateral PTC and cN0 who underwent total thyroidectomy and bilateral CLND. Nodal samples were divided into the prelaryngeal/pretracheal and ipsilateral and contralateral paratracheal regions, with each assessed for clinicopathologic predictors of central metastases. Postoperative morbidity and recurrence were assessed.
Results
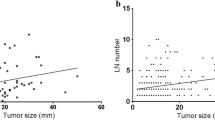
Rates of metastasis to ipsilateral and contralateral central compartments were 42.9 and 9.8%, respectively. Multivariate analysis showed that tumor size >1 cm and extrathyroidal extension were independent predictors of ipsilateral metastasis, and ipsilateral metastases independently predicted contralateral metastases (P < 0.05 each). Permanent hypoparathyroidism and incidental recurrent nerve paralysis were found in 1.6 and 0% of patients, respectively. After a mean follow-up of 46 months, none of these patients had recurrence in the central compartment.
Conclusions
Subclinical metastases are highly prevalent in the ipsilateral central neck of patients with PTC >1 cm. Contralateral central metastases, although uncommon, are associated with ipsilateral central metastases. These findings may guide the necessity and extent of prophylactic bilateral or unilateral CLND.
Similar content being viewed by others
References
Shaha AR. Management of the neck in thyroid cancer. Otolaryngol Clin North Am. 1998;31:823–31.
Shaha AR, Shah JP, Loree TR. Patterns of nodal and distant metastasis based on histologic varieties in differentiated carcinoma of the thyroid. Am J Surg. 1996;172:692–4.
Cooper DS, Doherty GM, Haugen BR, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2006;16:109–42.
Qubain SW, Nakano S, Baba M, et al. Distribution of lymph node micrometastasis in pN0 well-differentiated thyroid carcinoma. Surgery. 2002;131:249–56.
Gimm O, Rath FW, Dralle H. Pattern of lymph node metastases in papillary thyroid carcinoma. Br J Surg. 1998;85:252–4.
Machens A, Holzhausen HJ, Dralle H. Skip metastases in thyroid cancer leaping the central lymph node compartment. Arch Surg. 2004;139:43–5.
Mazzaferri EL, Doherty GM, Steward DL. The pros and cons of prophylactic central compartment lymph node dissection for papillary thyroid carcinoma. Thyroid. 2009;19:683–9.
Pereira JA, Jimeno J, Miquel J, et al. Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery. 2005;138:1095–100.
Cavicchi O, Piccin O, Caliceti U, et al. Transient hypoparathyroidism following thyroidectomy: a prospective study and multivariate analysis of 604 consecutive patients. Otolaryngol Head Neck Surg. 2007;137:654–8.
Kim MK, Mandel SH, Baloch Z, et al. Morbidity following central compartment reoperation for recurrent or persistent thyroid cancer. Arch Otolaryngol Head Neck Surg. 2004;130:1214–6.
Moley JF, Lairmore TC, Doherty GM, et al. Preservation of the recurrent laryngeal nerves in thyroid and parathyroid reoperations. Surgery. 1999;126:673–7.
Lundgren CI, Hall P, Dickman PW, et al. Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer. 2006;106:524–31.
Koo BS, Choi EC, Yoon YH, et al. Predictive factors for ipsilateral or contralateral central lymph node metastasis in unilateral papillary thyroid carcinoma. Ann Surg. 2009;249:840–4.
Carty SE, Cooper DS, Doherty GM, et al. Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid. 2009;19:1153–8.
Ito Y, Jikuzono T, Higashiyama T, et al. Clinical significance of lymph node metastasis of thyroid papillary carcinoma located in one lobe. World J Surg. 2006;30:1821–8.
Wada N, Duh QY, Sugino K, et al. Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg. 2003;237:399–407.
Koo BS, Lim HS, Lim YC, et al. Occult contralateral carcinoma in patients with unilateral papillary thyroid microcarcinoma. Ann Surg Oncol. 2010;17:1101–5.
Lee YS, Lim YS, Lee JC, et al. Clinical implication of the number of central lymph nde metastasis in papillary thyroid carcinoma: preliminary report. World J Surg. 2010;34:2558–63.
Mercante G, Frasoldati A, Pedroni C, et al. Prognostic factors affecting neck lymph node recurrence and distant metastasis in papillary microcarcinoma of the thyroid: results of a study in 445 patients. Thyroid. 2009;19:707–16.
So YK, Son YI, Hong SD, et al. Subclinical lymph node metastasis in papillary thyroid microcarcinoma: a study of 551 resections. Surgery. 2010;148:526–31.
Kouvaraki MA, Shapiro SE, Fornage BD, et al. Role of preoperative ultrasonography in the surgical management of patients with thyroid cancer. Surgery. 2003;134:946–54;
Rosário PW, de Faria S, Bicalho L, et al. Ultrasonographic differentiation between metastatic and benign lymph nodes in patients with papillary thyroid carcinoma. J Ultrasound Med. 2005;24:1385–9.
Roh JL, Koch WM. Role of sentinel lymph node biopsy in thyroid cancer. Expert Rev Anticancer Ther. 2010;10:1429–37.
Giles Senyurek Y, Tunca F, Boztepe H, et al. The long term outcome of papillary thyroid carcinoma patients without primary central lymph node dissection: expected improvement of routine dissection. Surgery. 2009;146:1188–95.
Alvarado R, Sywak MS, Delbridge L, et al. Central lymph node dissection as a secondary procedure for papillary thyroid cancer: is there added morbidity? Surgery. 2009;145:514–8.
Shen WT, Ogawa L, Ruan D, et al. Central neck lymph node dissection for papillary thyroid cancer: comparison of complication and recurrence rates in 295 initial dissections and reoperations. Arch Surg. 2010;145:272–5.
Cooper DS, Doherty GM, Haugen BR, et al. Revised American thyroid association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214.
Son YI, Jeong HS, Baek CH, et al. Extent of prophylactic lymph node dissection in the central neck area of the patients with papillary thyroid carcinoma: comparison of limited versus comprehensive lymph node dissection in a 2-year safety study. Ann Surg Oncol. 2008;15:2020–6.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roh, JL., Kim, JM. & Park, C.I. Central Lymph Node Metastasis of Unilateral Papillary Thyroid Carcinoma: Patterns and Factors Predictive of Nodal Metastasis, Morbidity, and Recurrence. Ann Surg Oncol 18, 2245–2250 (2011). https://doi.org/10.1245/s10434-011-1600-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-011-1600-z