Abstract
Background
We investigated sequential effects of HIFU ablation combined with contrast agent SonoVue by using histopathology examination, immunohistochemistry, and enzyme histochemistry.
Materials and Methods
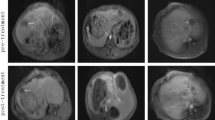
Forty rabbits with VX2 liver tumors were subjected to HIFU ablation. Before ablation, a bolus injection of 0.2 mL SonoVue was administrated in group II (n = 20), and normal saline solution was injected in group I (n = 20). On day 0, 3, 7, and 14 after ablation, 5 animals in each group were sacrificed. The tissue in ablated zone, transient zone (within 3 mm around ablated area), and surrounding zone (beyond 3 mm around ablated area) were collected. Coagulated volume measurement, hematoxylin-eosin staining, immunohistochemistry of Ki 67, Bcl-2, CD54, and MMP-2 to determine cell proliferation and tissue repair, and nicotinamide adenine dinucleotide phosphate-diaphorase (NADPH-d) and succinic dehydrogenase (SDH) staining to evaluate tissue viability were performed.
Results
The coagulated volume in group II at each time point was larger than that in group I (P < .05). After day 3, hematoxylin-eosin staining demonstrated necrosis in ablated zones and increasing surrounding fibra bands in group I and group II, while increasing expression of Ki 67, Bcl-2, CD54, and MMP-2 in transient zones was detected using immunohistochemistry in both groups (P > .05). NADPH-d and SDH staining showed dramatic decrease of enzyme activities in ablated zones immediately after ablation, while residual viable tissues in ablated zones of group II were less than those of group I (P < .05).
Conclusion
Contrast agent SonoVue enables improvement of HIFU ablation on rabbit VX2 liver tumors.






Similar content being viewed by others
References
Leslie TA, Kennedy JE. High intensity focused ultrasound in the treatment of abdominal and gynaecological diseases. Int J Hyperthermia. 2007;23:173–82.
Illing RO, Kennedy JE, Wu F, ter Haar GR, Protheroe AS, Friend PJ, et al. The safety and feasibility of extracorporeal high-intensity focused ultrasound (HIFU) for the treatment of liver and kidney tumours in a Western population. Br J Cancer. 2005;93:890–5.
Li CX, Xu GL, Jiang ZY, Li JJ, Luo GY, Shan HB, et al. Analysis of clinical effect of high-intensity focused ultrasound on liver cancer. World J Gastroenterol. 2004;10:2201–4.
Kennedy JE, Ter Haar GR, Cranston D. High intensity focused ultrasound: surgery of the future? Br J Radiol. 2003;76:590–9.
Haar GT, Coussios C. High intensity focused ultrasound: physical principles and devices. Int J Hyperthermia. 2007;23:89–104.
Rabkin BA, Zderic V, Vaezy S. Hyperecho in ultrasound images of HIFU therapy: involvement of cavitation. Ultrasound Med Biol. 2005;31:947–56.
Feng F, Mal A, Kabo M, Wang JC, Bar-Cohen Y. The mechanical and thermal effects of focused ultrasound in a model biological material. J Acoust Soc Am. 2005;117:2347–55.
Murat FJ, Poissonnier L, Pasticier G, Gelet A. High-intensity focused ultrasound (HIFU) for prostate cancer. Cancer Control. 2007;14:244–9.
Li YY, Sha WH, Zhou YJ, Nie YQ. Short and long term efficacy of high intensity focused ultrasound therapy for advanced hepatocellular carcinoma. J Gastroenterol Hepatol. 2007;22:2148–54.
Wu F, Wang ZB, Chen WZ, Zhu H, Bai J, Zou JZ, et al. Extracorporeal high intensity focused ultrasound ablation in the treatment of patients with large hepatocellular carcinoma. Ann Surg Oncol. 2004;11:1061–9.
Li JJ, Xu GL, Gu MF, Luo GY, Rong Z, Wu PH, et al. Complications of high intensity focused ultrasound in patients with recurrent and metastatic abdominal tumors. World J Gastroenterol. 2007;21:2747–51.
Ahmed M, Goldberg SN. Thermal ablation therapy for hepatocellular carcinoma. J Vasc Interv Radiol. 2002;13:S231–44.
Melodelima D, N’djin W, Parmentier H, Rivoire M, Chapelon J.-Y. Using a toroid transducer for thermal ablation by high-intensity-focused ultrasound increases the coagulated volume. J Acoust Soc Am. 2008;123:2995.
Luo W, Zhou X, Tian X, Ren X, Zheng M, Gu K, et al. Enhancement of ultrasound contrast agent in high-intensity focused ultrasound ablation. Adv Ther. 2006;23:861–8.
Cheng SQ, Zhou XD, Tang ZY, Yu Y, Bao SS, Qian DC. Iodized oil enhances the thermal effect of high-intensity focused ultrasound on ablating experimental liver cancer. J Cancer Res. Clin Oncol. 1997;123:639–44.
Kessel D, Jeffers R, Fowlkes JB, et al. Porphyrin-induced enhancement of ultrasound cytotoxicity. Int J Radiat Biol. 1994;66: 221-8.
Luo W, Zhou X, Ren X, Zheng M, Zhang J, He G. Enhancing effects of SonoVue, a microbubble sonographic contrast agent, on high-intensity focused ultrasound ablation in rabbit livers in vivo. J Ultrasound Med. 2007;26:469–76.
Yu T, Xiong S, Mason TJ, Wang Z. The use of a micro-bubble agent to enhance rabbit liver destruction using high intensity focused ultrasound. Ultrason Sonochem. 2006;13:143–9.
Kaneko Y, Maruyama T, Takegami K, Watanabe T, Mitsui H, Hanajiri K, et al. Use of a microbubble agent to increase the effects of high intensity focused ultrasound on liver tissue. Eur Radiol. 2005;15:1415–20.
Luo W, Zhou X, He G, Li Q, Zheng X, Fan Z, et al. Ablation of high intensity focused ultrasound combined with SonoVue on rabbit VX2 liver tumors: Assessment with conventional gray-scale US, conventional color/power Doppler US, contrast-enhanced color Doppler US, and contrast-enhanced pulse-inversion harmonic US. Ann Surg Oncol. 2008;15:2943–53.
Wang Z, Bai J, Li F, Du Y, Wen S, Hu K, et al. Study of a “biological focal region” of high-intensity focused ultrasound. Ultrasound Med Biol. 2003;29:749–54.
Wu F, Wang ZB, Cao YD, Xu ZL, Zhou Q, Zhu H, et al. Heat fixation of cancer cells ablated with high-intensity-focused ultrasound in patients with breast cancer. Am J Surg. 2006;192:179–84.
Nikfarjam M, Muralidharan V, Malcontenti-Wilson C, McLaren W, Christophi C. Impact of blood flow occlusion on liver necrosis following thermal ablation. ANZ J Surg. 2006;76:84–91.
Ozaki T, Tabuse K, Tsuji T, Nakamura Y, Kakudo K, Mori I. Microwave cell death: Enzyme histochemical evaluation for metastatic carcinoma of the liver. Pathol Int. 2003;53:837–45.
Yamashiki N, Kato T, Bejarano PA, Berho M, Montalvo B, Shebert RT, et al. Histopathological changes after microwave coagulation therapy for patients with hepatocellular carcinoma: review of 15 explanted livers. Am J Gastroenterol. 2003;98:2052–9.
Frich L, Bjørnland K, Pettersen S, Clausen OP, Gladhaug IP. Increased activity of matrix metalloproteinase 2 and 9 after hepatic radiofrequency ablation. J Surg Res. 2006;135:297–304.
Luo W, Zhou X, Zhang J, Qian Y, Zheng M, Yu M, et al. Analysis of apoptosis and cell proliferation after high intensity-focused ultrasound ablation combined with microbubbles in rabbit livers. Eur J Gastroenterol Hepatol. 2007;19:962–8.
Rai R, Richardson C, Flecknell P, Robertson H, Burt A, Manas DM. Study of apoptosis and heat shock protein (HSP) expression in hepatocytes following radiofrequency ablation (RFA). J Surg Res. 2005;129:147–51.
Nikfarjam M, Muralidharan V, Christophi C. Altered growth patterns of colorectal liver metastases after thermal ablation. Surgery. 2006;139:73–81.
Karavias DD, Tsamandas AC, Tepetes K, Kritikos N, Kourelis T, Ravazoula P, et al. BCL-2 and BAX expression and cell proliferation, after partial hepatectomy with and without ischemia, on cholestatic liver in rats: an experimental study. J Surg Res. 2003;110:399–408.
Scholzen T, Gerdes J. The Ki-67 protein: from the known and the unknown. J Cell Physiol. 2000;182:311–22.
Nelson AR, Fingleton B, Rothenberg ML, Matrisian LM. Matrix metalloproteinases: Biologic activity and clinical implications. J Clin Oncol. 2000;18:1135–49.
Qin LX, Tang ZY. Recent progress in predictive biomarkers for metastatic recurrence of human hepatocellular carcinoma: a review of the literature. J Cancer Res Clin Oncol. 2004;130:497–513.
Zhou XD. Recurrence and metastasis of hepatocellular carcinoma: progress and prospects. Hepatobiliary Pancreat Dis Int. 2002;1:35–41.
Tran BC, Seo J, Hall TL, Fowlkes JB, Cain CA. Effects of contrast agent infusion rates on thresholds for tissue damage produced by single exposures of high-intensity ultrasound. IEEE Trans Ultrason Ferroelectr Freq Control. 2005;52:1121–30.
Takegami K, Kaneko Y, Watanabe T, Maruyama T, Matsumoto Y, Nagawa H. Erythrocytes, as well as microbubble contrast agents, are important factors in improving thermal and therapeutic effects of high-intensity focused ultrasound. Ultrasound Med Biol. 2005;31:385–90.
Miller DL, Li P, Dou C, Gordon D, Edwards CA, Armstrong WF. Influence of contrast agent dose and ultrasound exposure on cardiomyocyte injury induced by myocardial contrast echocardiography in rats. Radiology. 2005;237:137–43.
Acknowledgment
The authors sincerely thank Jianguo He, Haiying Qin, Li Wang (Department of Ultrasound in Xijing Hospital, China), and Dr. Zhiyong Fan (Department of Hepatobiliary Surgery in Xijing Hospital, China) for the excellent assistance in HIFU performance, surgical operation, and animal care.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Luo, W., Zhou, X., Yu, M. et al. Ablation of High-Intensity Focused Ultrasound Assisted with SonoVue on Rabbit VX2 Liver Tumors: Sequential Findings with Histopathology, Immunohistochemistry, and Enzyme Histochemistry. Ann Surg Oncol 16, 2359–2368 (2009). https://doi.org/10.1245/s10434-009-0419-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-009-0419-3