Abstract
Background
The aim of this study was to analyze clinical and anatomical factors affecting the pathologic quality of the resected specimen after total mesorectal excision (TME) for rectal cancer.
Methods
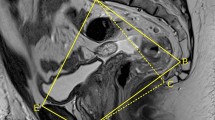
A total of 100 patients who underwent TME for mid or low rectal cancer were evaluated prospectively. MRI pelvimetry data (transverse diameter, obstetric conjugate, interspinous distance, sacrum length, and sacrum depth) were analyzed as anatomically affecting factors to postoperative specimen quality. Sex, body mass index (BMI), type of surgery, tumor size, and tumor distance from the anal verge were analyzed as clinically affecting factors. The gross judgment of resected specimen, circumferential resection margin and the number of harvested lymph nodes were used to access postoperative specimen quality.
Results
The univariate and multivariate analysis showed that narrow obstetric conjugate and shorter interspinous distance were related to the inadequate quality of the mesorectum in the specimen (P = 0.022, P = 0.030). Interspinous distance was a predicting factor of a positive circumferential resection margin (P = 0.007). There were no clinical factors affecting the inadequate quality of the mesorectum or positive circumferential resection margin. Moreover, there were no clinico-anatomical factors affecting the number of harvested lymph nodes after TME.
Conclusion
Narrow obstetric conjugate and shorter interspinous distance were factors leading to poor postoperative specimen quality. Rectal cancer patients with narrow obstetric conjugate or shorter interspinous distance should be considered as high-risk patients with regard to specimen quality, which is in turn related to oncological outcome.


Similar content being viewed by others
References
Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery - clue to pelvic recurrence? Br J Surg 1982;69:613–6
Havenga K, DeRuiter MC. Enker WE, Welvaart K. Anatomic basis of autonomic nerve preserving total mesorectal excision for rectal cancer. Br J Surg 1996;83:384–8
Church JM, Raudkivi PJ, Hill GL. The surgical anatomy of the rectum-a review with particular relevance to the hazard of rectal mobilization. Int J Colorectal Dis 1987;2:158–66
Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK. Rectal cancer: the Basingstoke experience of total mesorectal excision, 1987–1997. Arch Surg 1998;133:894–9
Enker WE, Thaler HT, Cranor ML, Polyak T. Total mesorectal excision in the operative treatment of carcinoma of the rectum. J Am Coll Surg 1995;181;335–46
Nagtegaal ID van de Velde CJ, van der Worp E, et al. Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality conrol. J Clin Oncol 2002;20:1729–34
Maslekar S, Sharma A, MacDonald A, et al. Mesorectal grades predict recurrences after curative resection for rectal cancer. Dis Colon Rectum 2006;50:168–75
Lee HY, Choi HJ, Park KJ, et al. Prognostic significance of metastatic lymph node ratio in node-positive colon carcinoma. Ann Surg Oncol 2007;14:1712–7
Le Voyer TE, Sigurdson ER, Hanlon AL, et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 2003;21:2912–9
Swanson RS, Compton CC, Stewart AK, Bland KI. The prognosis of T3N0 colon cancer is dependent on the number of lymph nodes examined. Ann Surg Oncol 2003;10:65–71
NIH consensus conference adjuvant therapy for patients with colon and rectal cancer. JAMA 1990;264:1444–50
Handa VL, Pannu HK, Siddique S, Gutman R, VonRooyen J, Cundiff Geoff. Architectural difference in the bony pelvis of women with and without pelvic floor disorders. Obstet Gynecol 2003;102:1283–90
Stark DD, McCarthy SM, Filly RA, Parer JT, Hricak H, Callen PW. Pelvimetry by magnetic resonance imaging. AJR Am J Roentgenol 1985;144:947–50
Wright AR, English PT, Cameron HM, Wilsdon JB. MR pelvimetry: a practical alteration. Acta Radiol 1992;33:582–7
van Loon AJ, Mantingh A, Serlier EK, Kroon G, Mooyaart EL, Huisjes HJ. Randomized controlled trial of magnetic-resonance pelvimetry in breech presentation at term. Lancet 1997;350:1799–4
Sporri S, Hanggi W, Braghetti A, Vock P, Schneider H. Pelvimetry by magnetic resonance imaging as a diagnostic tool to evaluate dystocia. Obstet Gynecol 1997;89:902–8
Levine D, Barnes PD, Edelman RR. Obstetric MR imaging. Radiology 1999;211:609–17
Junginger T, Hermanek P, Klimpfinger M. Klassifikation maligner Tumoren des Gastrointestinaltrakts I. Berlin Heidelberg New York: Springer, 2002
Baik SH, Kim NK, Lee YC, et al. Prognostic significance of circumferential resection margin following total mesorectal excision and adjuvant chemoradiotherapy in patients with rectal cancer. Ann Surg Oncol 2007;14:462–9
Quirke P, Durdey P, Dixon MF, Williams NS. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection: histopathological study of lateral tumor spread and surgical excision. Lancet 1986;2:996–9
Adam IJ, Mohamdee MO, Martin IG, et al. Role of circumferential resection margin involvement in the local recurrence of rectal cancer. Lancet 1994;344:701–11
Boyle KM, Petty D, Chalmers AG, et al. MRI assessment of the bony pelvis may help predict resectability of rectal cancer. Colorectal Dis 2005;7:232–240
Acknowledgement
This study was supported by a faculty research grant of the Yonsei University College of Medicine in 2006 (no. 6-2006-0093).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hyuk Baik, S., Kyu Kim, N., Young Lee, K. et al. Factors Influencing Pathologic Results after Total Mesorectal Excision for Rectal Cancer: Analysis of Consecutive 100 Cases. Ann Surg Oncol 15, 721–728 (2008). https://doi.org/10.1245/s10434-007-9706-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-007-9706-z