Abstract
Background
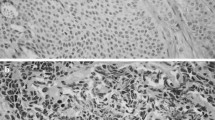
Tumor grade is an important predictor of survival in gastroenteropancreatic (GEP) neuroendocrine tumors (NETs), as determined by Ki-67 expression and mitotic rate. NETs generally grow indolently, but some cells may acquire traits facilitating metastasis. It is unclear how frequently metastases differ in grade from their primary tumors, and whether increasing grade in metastases affects prognosis.
Methods
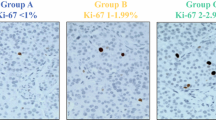
Ki-67 immunohistochemistry was performed on resected GEPNET specimens and cases with results for both primary tumors and concurrent metastases were identified. Grade was determined using a modified World Health Organization classification (Ki-67: G1 = 0–2%; G2 > 2–20%; G3 > 20%).
Results
Ki-67 was performed on both the primary tumor and metastases in 103 patients. Tumor grade was higher in metastases from 25 (24%) patients, 24 increased from G1 to G2, and 1 increased from G2 to G3; 68 (66%) patients had no change in grade (42 G1 and 26 G2), and 10 (10%) decreased from G2 to G1. No clinicopathologic factors were predictive of higher grade in metastases. The 5-year progression-free survival (PFS) was 55% for patients with stable grade versus 8% of patients with increased grade, while 5-year overall survival (OS) was 92 and 54%, respectively. The 5-year OS of patients who had stable grade with G1 and G2 primaries was 92 and 64%, respectively.
Conclusions
Nearly one-third of patients had metastases with a different grade than their primary, and, when grade increased, both PFS and OS significantly decreased. Determining the grade in both the primary tumor and a metastasis is important for estimating prognosis and to help inform decisions regarding additional therapies.


Similar content being viewed by others
References
Hallet J, Law CH, Cukier M, Saskin R, Liu N, Singh S. Exploring the rising incidence of neuroendocrine tumors: a population-based analysis of epidemiology, metastatic presentation, and outcomes. Cancer. 2015;121(4):589–97.
Boyar Cetinkaya R, Aagnes B, Thiis-Evensen E, Tretli S, Bergestuen DS, Hansen S. Trends in incidence of neuroendocrine neoplasms in Norway: a report of 16,075 cases from 1993 through 2010. Neuroendocrinology. 2015;104(1):1–10.
Grillo F, Albertelli M, Annunziata F, Boschetti M, Caff A, Pigozzi S, et al. Twenty years of gastroenteropancreatic neuroendocrine tumors: is reclassification worthwhile and feasible? Endocrine. 2015;53(1):58–62.
Yang M, Ke NW, Zeng L, Zhang Y, Tan CL, Zhang H, et al. Survival analyses for patients with surgically resected pancreatic neuroendocrine tumors by World Health Organization 2010 grading classifications and American Joint Committee on Cancer 2010 staging systems. Medicine. 2015;94(48):e2156.
Khan MS, Luong TV, Watkins J, Toumpanakis C, Caplin ME, Meyer T. A comparison of Ki-67 and mitotic count as prognostic markers for metastatic pancreatic and midgut neuroendocrine neoplasms. Br J Cancer. 2013;108(9):1838–45.
McCall CM, Shi C, Cornish TC, Klimstra DS, Tang LH, Basturk O, et al. Grading of well-differentiated pancreatic neuroendocrine tumors is improved by the inclusion of both Ki67 proliferative index and mitotic rate. Am J Surg Pathol. 2013;37(11):1671–7.
Rindi G, Kloppel G, Couvelard A, Komminoth P, Korner M, Lopes JM, et al. TNM staging of midgut and hindgut (neuro) endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 2007;451(4):757–62.
Rindi G, Arnold R, Bosman FT, Capella C, Klimstra DS, Kloppel G, et al. Nomenclature and classification of neuroendocrine neoplasms of the digestive system. In: Bosman FT, Carneiro F, Hruban RH, Theise ND (eds). WHO classification of tumours of the digestive system. 4th ed. Lyon: International Agency for Research on Cancer; 2010. pp. 13–4.
Grillo F, Albertelli M, Brisigotti MP, Borra T, Boschetti M, Fiocca R, et al. Grade increases in gastro-entero-pancreatic neuroendocrine tumor metastases compared to the primary tumor. Neuroendocrinology. 2015;103(5):452–9.
Shi C, Gonzalez RS, Zhao Z, Koyama T, Cornish TC, Hande KR, et al. Liver metastases of small intestine neuroendocrine tumors: Ki-67 heterogeneity and World Health Organization grade discordance with primary tumors. Am J Clin Pathol. 2015;143(3):398–404.
Mitry E, Baudin E, Ducreux M, Sabourin JC, Rufie P, Aparicio T, et al. Treatment of poorly differentiated neuroendocrine tumours with etoposide and cisplatin. Br J Cancer. 1999;81(8):1351–-5.
Moertel CG, Kvols LK, O’Connell MJ, Rubin J. Treatment of neuroendocrine carcinomas with combined etoposide and cisplatin. Evidence of major therapeutic activity in the anaplastic variants of these neoplasms. Cancer. 1991;68(2):227–32.
Fjallskog ML, Granberg DP, Welin SL, Eriksson C, Oberg KE, Janson ET, et al. Treatment with cisplatin and etoposide in patients with neuroendocrine tumors. Cancer. 2001;92(5):1101–7.
Caplin ME, Pavel M, Cwikla JB, Phan AT, Raderer M, Sedlackova E, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224–33.
Frilling A, Clift AK. Therapeutic strategies for neuroendocrine liver metastases. Cancer. 2015;121(8):1172–86.
Rinke A, Muller HH, Schade-Brittinger C, Klose KJ, Barth P, Wied M, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27(28):4656–63.
Givi B, Pommier SJ, Thompson AK, Diggs BS, Pommier RF. Operative resection of primary carcinoid neoplasms in patients with liver metastases yields significantly better survival. Surgery. 2006;140(6):891–7
Maxwell JE, Sherman SK, O’Dorisio TM, Bellizzi AM, Howe JR. Liver-directed surgery of neuroendocrine metastases: what is the optimal strategy? Surgery. 2016;159(1):320–35.
Yao JC, Fazio N, Singh S, Buzzoni R, Carnaghi C, Wolin E, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968–77.
Yao JC, Shah MH, Ito T, Bohas CL, Wolin EM, Van Cutsem E, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):514–23.
Liu E, Marincola P, Oberg K. Everolimus in the treatment of patients with advanced pancreatic neuroendocrine tumors: latest findings and interpretations. Therap Adv Gastroenterol. 2013;6(5):412–9.
Raymond E, Dahan L, Raoul JL, Bang YJ, Borbath I, Lombard-Bohas C, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):501–13.
Abdel-Rahman O, Fouad M. Temozolomide-based combination for advanced neuroendocrine neoplasms: a systematic review of the literature. Future Oncol. 2015;11(8):1275–90.
Claringbold PG, Price RA, Turner JH. Phase I-II study of radiopeptide 177Lu-octreotate in combination with capecitabine and temozolomide in advanced low-grade neuroendocrine tumors. Cancer Biother Radiopharm. 2012;27(9):561–9.
Welin S, Sorbye H, Sebjornsen S, Knappskog S, Busch C, Oberg K. Clinical effect of temozolomide-based chemotherapy in poorly differentiated endocrine carcinoma after progression on first-line chemotherapy. Cancer. 2011;117(20):4617–22.
Cherenfant J, Talamonti MS, Hall CR, Thurow TA, Gage MK, Stocker SJ, et al. Comparison of tumor markers for predicting outcomes after resection of nonfunctioning pancreatic neuroendocrine tumors. Surgery. 2014;156(6):1504–10
Richards-Taylor S, Ewings SM, Jaynes E, Tilley C, Ellis SG, Armstrong T, et al. The assessment of Ki-67 as a prognostic marker in neuroendocrine tumours: a systematic review and meta-analysis. J Clin Pathol. 2016;69(7):612–8.
Hamilton NA, Liu TC, Cavatiao A, Mawad K, Chen L, Strasberg SS, et al. Ki-67 predicts disease recurrence and poor prognosis in pancreatic neuroendocrine neoplasms. Surgery. 2012;152(1):107–13.
Acknowledgment
T32: T32CA148062 (KK, JM), and SPORE: P50CA174521 (JH, JD, PB, GL, TO, AB).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keck, K.J., Choi, A., Maxwell, J.E. et al. Increased Grade in Neuroendocrine Tumor Metastases Negatively Impacts Survival. Ann Surg Oncol 24, 2206–2212 (2017). https://doi.org/10.1245/s10434-017-5899-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5899-y