Abstract
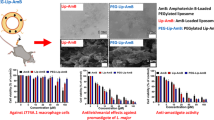
The present study aimed to develop, characterize and evaluate the amphotericin B–loaded nanostructured lipid carriers (AmB-NLCs) for topical treatment of cutaneous leishmaniasis (CL) and vulvovaginal candidiasis (VVC). AmB-NLCs were characterized for particle size, zeta potential, encapsulation efficiency and surface morphology. Prepared NLCs were also characterized for in vitro drug release, ex vivo skin permeation and deposition before evaluating their in vitro and in vivo efficacy. Cytotoxicity of NLCs was assessed on MRC-5 cells, whereas skin irritation potential was evaluated in vivo using rats. Significant accumulation of drug in to the skin supported the topical application potential of drug-loaded NLCs. Encapsulation of AmB in NLCs resulted in enhanced in vitro potency against promastigotes and intracellular amastigotes of L. major JISH 118 (IC50 ± SEM = 0.02 ± 0.1 μM for both) compared with free drug (IC50 ± SEM = 0.15 ± 0.2 & 0.14 ± 0.0, respectively). Similar improved potency of AmB-NLCs was also observed for other Leishmania and fungal strains compared with drug solution. Topical application of AmB-NLCs on L. major–infected BALB/c mice caused a significant reduction in parasite burden per mg of lesion (65 × 108 ± 13) compared with the control group (> 167.8 × 108 ± 11). Topical AmB-NLCs gel demonstrated superior efficacy in the vaginal C. albicans rat model for VVC as compared with plain AmB gel. Moreover, results of in vitro cytotoxicity assay and in vivo skin irritation test confirmed AmB-NLCs to be non-toxic and safe for topical use. In conclusion, NLCs may have promising potential as carrier for topical treatment of various conditions of skin and mucosa.






Similar content being viewed by others

Change history
08 October 2020
In the published manuscript, co-author Sarah Hendrickx name was misspelled and co-author Guy Caljon���s last and first names were inadvertently switched.
References
de Vries HJ, Reedijk SH, Schallig HD. Cutaneous leishmaniasis: recent developments in diagnosis and management. Am J Clin Dermatol. 2015;16(2):99–109.
Hepburn NC. Cutaneous leishmaniasis: current and future management. Expert Rev Anti-Infect Ther. 2003;1(4):563–70.
Arana B. Cutaneous Leishmaniasis: treatment needs and combination therapies. Int J Infect Dis. 2018;73:47.
Van Bocxlaer K, Yardley V, Murdan S, Croft SL. Topical formulations of miltefosine for cutaneous leishmaniasis in a BALB/c mouse model. J Pharm Pharmacol. 2016;68(7):862–72.
Dorgan E, Denning DW, McMullan R. Burden of fungal disease in Ireland. J Med Microbiol. 2015;64(4):423–6.
Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide. Mycoses. 2008;51:2–15.
Song Y, Wang Y, Thakur R, Meidan VM, Michniak B. Mucosal drug delivery: membranes, methodologies, and applications. Critical Reviews™ in Therapeutic Drug Carrier Systems. 2004;21(3).
Lemke A, Kiderlen AF, Kayser O. Amphotericin B. Appl Microbiol Biotechnol. 2005;68(2):151–62.
Brajtburg J, Powderly WG, Kobayashi GS, Medoff G. Amphotericin B: current understanding of mechanisms of action. Antimicrob Agents Chemother. 1990;34(2):183–8.
Croft SL, Seifert K, Yardley V. Current scenario of drug development for leishmaniasis. Indian J Med Res. 2006;123(3):399–410.
Sobel JD. Recurrent vulvovaginal candidiasis. Am J Obstet Gynecol. 2016;214(1):15–21.
King CT, Rogers PD, Cleary JD, Chapman SW. Antifungal therapy during pregnancy. Clin Infect Dis. 1998;27(5):1151–60.
Sheikh S, Ahmad A, Ali SM, Paithankar M, Barkate H, Raval R. Topical delivery of lipid based amphotericin B gel in the treatment of fungal infection: a clinical efficacy, safety and tolerability study in patients. J Clin Exp Dermatol Res. 2014;5(248):2.
Heidari-Kharaji M, Taheri T, Doroud D, Habibzadeh S, Rafati S. Solid lipid nanoparticle loaded with paromomycin: in vivo efficacy against Leishmania tropica infection in BALB/c mice model. Appl Microbiol Biotechnol. 2016;100(16):7051–60.
Ammar AA, Nasereddin A, Ereqat S, Dan-Goor M, Jaffe CL, Zussman E, et al. Amphotericin B-loaded nanoparticles for local treatment of cutaneous leishmaniasis. Drug Delivery and Translational Research. 2019;9(1):76–84.
Ensign LM, Cone R, Hanes J. Nanoparticle-based drug delivery to the vagina: a review. J Control Release. 2014;190:500–14.
Trombino S, Mellace S, Cassano R. Solid lipid nanoparticles for antifungal drugs delivery for topical applications. Ther Deliv. 2016;7(9):639–47.
Singh S, Singh M, Tripathi CB, Arya M, Saraf SA. Development and evaluation of ultra-small nanostructured lipid carriers: novel topical delivery system for athlete’s foot. Drug delivery and translational research. 2016;6(1):38–47.
Das S, Ng WK, Tan RB. Are nanostructured lipid carriers (NLCs) better than solid lipid nanoparticles (SLNs): development, characterizations and comparative evaluations of clotrimazole-loaded SLNs and NLCs? Eur J Pharm Sci. 2012;47(1):139–51.
Riaz A, Ahmed N, Khan MI, ur Rehman A, Khan GM. Formulation of topical NLCs to target macrophages for cutaneous Leishmaniasis. Journal of Drug Delivery Science and Technology. 2019:101232.
Tran TH, Ramasamy T, Truong DH, Choi H-G, Yong CS, Kim JO. Preparation and characterization of fenofibrate-loaded nanostructured lipid carriers for oral bioavailability enhancement. AAPS PharmSciTech. 2014 December 01;15(6):1509–15.
Javed I, Hussain SZ, Ullah I, Khan I, Ateeq M, Shahnaz G, et al. Synthesis, characterization and evaluation of lecithin-based nanocarriers for the enhanced pharmacological and oral pharmacokinetic profile of amphotericin B. J Mater Chem B. 2015;3(42):8359–65.
Butani D, Yewale C, Misra A. Topical amphotericin B solid lipid nanoparticles: design and development. Colloids Surf B: Biointerfaces. 2016;139:17–24.
Phatak AA, Chaudhari PD. Development and evaluation of nanostructured lipid carrier (NLC) based topical delivery of an anti-inflammatory drug. J Pharm Res. 2013;7(8):677–85.
Hajjar B, Zier K-I, Khalid N, Azarmi S, Löbenberg R. Evaluation of a microemulsion-based gel formulation for topical drug delivery of diclofenac sodium. Journal of Pharmaceutical Investigation. 2018;48(3):351–62.
Zhu Y, Chen X, McClements DJ, Zou L, Liu W. pH-, ion-and temperature-dependent emulsion gels: fabricated by addition of whey protein to gliadin-nanoparticle coated lipid droplets. Food Hydrocoll. 2018;77:870–8.
Maitra M, Goyal AK, Rath G. A novel approach for follicular delivery of minoxidil for treatment of alopecia. Journal of Drug Delivery Science and Technology. 2017;41:113–23.
Santiago RR, e Silva KGH, dos Santos ND, Genre J, de Oliveira Lione VF, Silva AL, et al. Nanostructured lipid carriers containing Amphotericin B: development, in vitro release assay, and storage stability. Journal of Drug Delivery Science and Technology. 2018;48:372–82.
Joshi M, Patravale V. Nanostructured lipid carrier (NLC) based gel of celecoxib. Int J Pharm. 2008;346(1–2):124–32.
Mothana R, Al-Musayeib N, Matheeussen A, Cos P, Maes L. Assessment of the in vitro antiprotozoal and cytotoxic potential of 20 selected medicinal plants from the island of Soqotra. Molecules. 2012;17(12):14349–60.
James O, Sunday AB. Evaluation of acute dermal irritation and wound contraction by Gymnema Sylvestre and Datura Metel extracts in rats. American Journal of Biomedical and Life Sciences. 2014;2(4):83–8.
Vermeersch M, da Luz RI, Toté K, Timmermans J-P, Cos P, Maes L. In vitro susceptibilities of Leishmania donovani promastigote and amastigote stages to antileishmanial reference drugs: practical relevance of stage-specific differences. Antimicrob Agents Chemother. 2009;53(9):3855–9.
da Luz RI, Vermeersch M, Dujardin J-C, Cos P, Maes L. In vitro sensitivity testing of Leishmania clinical field isolates: preconditioning of promastigotes enhances infectivity for macrophage host cells. Antimicrob Agents Chemother. 2009;53(12):5197–203.
Van de Ven H, Paulussen C, Feijens P, Matheeussen A, Rombaut P, Kayaert P, et al. PLGA nanoparticles and nanosuspensions with amphotericin B: Potent in vitro and in vivo alternatives to Fungizone and AmBisome. J Control Release. 2012;161(3):795–803.
Inocêncio da Luz RA, Vermeersch M, Deschacht M, Hendrickx S, Van Assche T, Cos P, et al. In vitro and in vivo prophylactic and curative activity of the triterpene saponin PX-6518 against cutaneous Leishmania species. J Antimicrob Chemother. 2011;66(2):350–3.
de Wit K, Paulussen C, Matheeussen A, van Rossem K, Cos P, Maes L. In vitro profiling of pramiconazole and in vivo evaluation in Microsporum canis dermatitis and Candida albicans vaginitis laboratory models. Antimicrob Agents Chemother. 2010;54(11):4927–9.
Chetoni P, Burgalassi S, Monti D, Tampucci S, Tullio V, Cuffini AM, et al. Solid lipid nanoparticles as promising tool for intraocular tobramycin delivery: pharmacokinetic studies on rabbits. Eur J Pharm Biopharm. 2016;109:214–23.
Shah R, Eldridge D, Palombo E, Harding I. Optimisation and stability assessment of solid lipid nanoparticles using particle size and zeta potential. Journal of Physical Science. 2014;25(1).
Bhosale R, Bhandwalkar O, Duduskar A, Jadhav R, Pawar P. Water soluble chitosan mediated voriconazole microemulsion as sustained carrier for ophthalmic application: in vitro/ex vivo/in vivo evaluations. Open Pharmaceutical Sciences Journal. 2016;3(1).
Teng Z, Yu M, Ding Y, Zhang H, Shen Y, Jiang M, et al. Preparation and characterization of nimodipine-loaded nanostructured lipid systems for enhanced solubility and bioavailability. Int J Nanomedicine. 2019;14:119.
Madane RG, Mahajan HS. Curcumin-loaded nanostructured lipid carriers (NLCs) for nasal administration: design, characterization, and in vivo study. Drug delivery. 2016;23(4):1326–34.
Chawla V, Saraf SA. Rheological studies on solid lipid nanoparticle based carbopol gels of aceclofenac. Colloids Surf B: Biointerfaces. 2012;92:293–8.
Sachan AK, Gupta A, Arora M. Formulation & characterization of nanostructured lipid carrier (NLC) based gel for topical delivery of etoricoxib. Journal of Drug Delivery and Therapeutics. 2016;6(2):4–13.
Hafeez A, Kazmi I. Dacarbazine nanoparticle topical delivery system for the treatment of melanoma. Sci Rep. 2017;7(1):16517.
Fang C-L, Al- Suwayeh S, Fang J-Y. Nanostructured lipid carriers (NLCs) for drug delivery and targeting. Recent Patents on Nanotechnology. 2013;7(1):41–55.
Jain V, Gupta A, Pawar VK, Asthana S, Jaiswal AK, Dube A, et al. Chitosan-assisted immunotherapy for intervention of experimental Leishmaniasis via amphotericin B-loaded solid lipid nanoparticles. Appl Biochem Biotechnol. 2014 October 01;174(4):1309–30.
Jansook P, Pichayakorn W, Ritthidej GC. Amphotericin B-loaded solid lipid nanoparticles (SLNs) and nanostructured lipid carrier (NLCs): effect of drug loading and biopharmaceutical characterizations. Drug Dev Ind Pharm. 2018;44(10):1693–700.
Dash S, Murthy PN, Nath L, Chowdhury P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol Pharm. 2010;67(3):217–23.
Fang J-Y, Fang C-L, Liu C-H, Su Y-H. Lipid nanoparticles as vehicles for topical psoralen delivery: solid lipid nanoparticles (SLN) versus nanostructured lipid carriers (NLC). Eur J Pharm Biopharm. 2008;70(2):633–40.
Schäfer-Korting M, Mehnert W, Korting H-C. Lipid nanoparticles for improved topical application of drugs for skin diseases. Adv Drug Deliv Rev. 2007;59(6):427–43.
Gupta M, Vyas SP. Development, characterization and in vivo assessment of effective lipidic nanoparticles for dermal delivery of fluconazole against cutaneous candidiasis. Chem Phys Lipids. 2012;165(4):454–61.
Severino P, Andreani T, Macedo AS, Fangueiro JF, Santana MHA, Silva AM, et al. Current state-of-art and new trends on lipid nanoparticles (SLN and NLC) for oral drug delivery. 2012;2012.
Dolatabadi JEN, Azami A, Mohammadi A, Hamishehkar H, Panahi-Azar V, Saadat YR, et al. Formulation, characterization and cytotoxicity evaluation of ketotifen-loaded nanostructured lipid carriers 2018;46:268–273.
Silva A, González-Mira E, García M, Egea M, Fonseca J, Silva R, et al. Preparation, characterization and biocompatibility studies on risperidone-loaded solid lipid nanoparticles (SLN): high pressure homogenization versus ultrasound. 2011;86(1):158–65.
Müller RH, Rühl D, Runge S, Schulze-Forster K, Mehnert WJPr. Cytotoxicity of solid lipid nanoparticles as a function of the lipid matrix and the surfactant 1997;14(4):458–62.
Gokce EH, Korkmaz E, Dellera E, Sandri G, Bonferoni MC, Ozer OjIjon. Resveratrol-loaded solid lipid nanoparticles versus nanostructured lipid carriers: evaluation of antioxidant potential for dermal applications 2012;7:1841.
Üner MJDp-aijops. Preparation, characterization and physico-chemical properties of solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC): their benefits as colloidal drug carrier systems. 2006;61(5):375–86.
Müller RH, MaÈder K, Gohla S. Solid lipid nanoparticles (SLN) for controlled drug delivery–a review of the state of the art. Eur J Pharm Biopharm. 2000;50(1):161–77.
Song X, Lin Q, Guo L, Fu Y, Han J, Ke H, et al. Rifampicin loaded mannosylated cationic nanostructured lipid carriers for alveolar macrophage-specific delivery. Pharm Res. 2015;32(5):1741–51.
Zhu L, Cao X, Xu Q, Su J, Li X, Zhou WJIjon evaluation of the antibacterial activity of tilmicosin-slN against Streptococcus agalactiae: in vitro and in vivo studies 2018;13:4747.
Nasseri M, Golmohammadzadeh S, Arouiee H, Jaafari MR, Neamati H. Antifungal activity of Zataria multiflora essential oil-loaded solid lipid nanoparticles in-vitro condition 2016;19(11):1231.
Gandomi N, Atyabi F, Fazeli M, Farbood E, Dinarvand R. Solid lipid nanoparticles of ciprofloxacin hydrochloride with enhanced antibacterial activity 2012;7(5):271.
Fazly Bazzaz B, Khameneh B, Namazi N, Iranshahi M, Davoodi D, Golmohammadzadeh SJ. Solid lipid nanoparticles carrying Eugenia caryophyllata essential oil: the novel nanoparticulate systems with broad-spectrum antimicrobial activity 2018;66(6):506–513.
Kharaji MH, Doroud D, Taheri T, Rafati S. Drug targeting to macrophages with solid lipid nanoparticles harboring paromomycin: an in vitro evaluation against L. major and L. tropica. AAPS PharmSciTech. 2016 Oct;17(5):1110–9.
Jain K, Jain NKJD. Novel therapeutic strategies for treatment of visceral leishmaniasis 2013;18(23–24):1272–81.
Kunjachan S, Gupta S, Dwivedi AK, Dube A, Chourasia MKJJ. Chitosan-based macrophage-mediated drug targeting for the treatment of experimental visceral leishmaniasis 2011;28(4):301–10.
Xie S, Tao Y, Pan Y, Qu W, Cheng G, Huang L, et al. Biodegradable nanoparticles for intracellular delivery of antimicrobial agents 2014;187:101–17.
Xie S, Yang F, Tao Y, Chen D, Qu W, Huang L, et al. Enhanced intracellular delivery and antibacterial efficacy of enrofloxacin-loaded docosanoic acid solid lipid nanoparticles against intracellular Salmonella 2017;7:41104.
Nasseri M, Golmohammadzadeh S, Arouiee H, Jaafari MR, Neamati H. Antifungal activity of Zataria multiflora essential oil-loaded solid lipid nanoparticles in-vitro condition. Iranian Journal of Basic Medical Sciences. 2016;19(11):1231–7.
Mayelifar K, Taheri AR, Rajabi O, Sazgarnia A. Ultraviolet B efficacy in improving antileishmanial effects of silver nanoparticles. Iranian journal of basic medical sciences. 2015;18(7):677–83.
Bavarsad N, Bazzaz BSF, Khamesipour A, Jaafari MR. Colloidal, in vitro and in vivo anti-leishmanial properties of transfersomes containing paromomycin sulfate in susceptible BALB/c mice. Acta Trop. 2012;124(1):33–41.
Pople PV, Singh KK. Targeting tacrolimus to deeper layers of skin with improved safety for treatment of atopic dermatitis. Int J Pharm. 2010;398(1–2):165–78.
Monteiro LM, Löbenberg R, Cotrim PC, de Barros Araujo GL, Bou-Chacra N. Buparvaquone nanostructured lipid carrier: development of an affordable delivery system for the treatment of leishmaniases. BioMed research international. 2017;2017.
Ghadiri M, Vatanara A, Doroud D, Najafabadi AR. Paromomycin loaded solid lipid nanoparticles: characterization of production parameters. Biotechnol Bioprocess Eng. 2011;16(3):617–23.
Fernandes Costa A, Evangelista Araujo D, Santos Cabral M, Teles Brito I, Borges de Menezes Leite L, Pereira M, et al. Development, characterization, and in vitro–in vivo evaluation of polymeric nanoparticles containing miconazole and farnesol for treatment of vulvovaginal candidiasis. Med Mycol 2018;57(1):52–62.
Cassone A, Sobel JD. Experimental models of vaginal candidiasis and their relevance to human candidiasis. Infect Immun. 2016;84(5):1255–61.
Bonifácio BV, dos Santos Ramos MA, da Silva PB, Negri KMS, de Oliveira LÉ, de Souza LP, et al. Nanostructured lipid system as a strategy to improve the anti-Candida albicans activity of Astronium sp. Int J Nanomedicine. 2015;10:5081.
Funding
Higher Education Commission of Pakistan (HEC) provided funding for this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 1.07 mb)
Rights and permissions
About this article
Cite this article
Riaz, A., Hendricks, S., Elbrink, K. et al. Preparation and Characterization of Nanostructured Lipid Carriers for Improved Topical Drug Delivery: Evaluation in Cutaneous Leishmaniasis and Vaginal Candidiasis Animal Models. AAPS PharmSciTech 21, 185 (2020). https://doi.org/10.1208/s12249-020-01717-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-020-01717-w