Abstract
In addition to its content of traditional nutrients, milk is a rich source of hormones and peptides, which survive digestion in the neonatal gastrointestinal tract secondary to lower proteolytic activity and increased protein permeability. Previous studies have shown accelerated erythropoiesis or elevated serum erythropoietin (Epo) levels in neonatal (suckling) animals after maternal phlebotomy or maternal hypoxia exposure. We sought to determine whether significant quantities of Epo are present in human milk and whether Epo remains intact under physiologic digestion conditions. Immunoreactive Epo concentrations were determined in 409 human milk samples obtained from mothers of term and premature infants. Samples collected between birth and postpartum d 134 were divided into 11 postpartum day groups. Mean milk-borne Epo concentrations were within the normal range for plasma Epo concentrations and rose with postpartum day (F10,398 = 5.82, p < 0.0001). No differences were observed between milk collected from mothers of premature versus term infants. Estimated weekly human milk-borne Epo intakes approximated the lower range of published parenteral therapeutic doses. In simulated digestion at physiologic pH levels of 3.2, 5.8, and 7.4, milk-borne Epo resisted degradation at 1 and 2 h, compared with baseline. Therefore, we conclude that human milk contains considerable amounts of Epo which resist degradation after exposure to gastric juices at physiologic pH levels. These results support continued investigation into the fate and developmental roles of Epo in human milk.
Similar content being viewed by others
Main
Mammalian milk is a rich source of hormones and peptides. Insulin, insulin-like growth factors, epidermal growth factor, transforming growth factor-α, and ILs (IL-6, IL-8, and IL-10) are all present in considerable concentrations in mammalian milk(1–6). Because the neonatal gastrointestinal tract exhibits less proteolytic activity and is more permeable to proteins than that of older individuals, many of these milk-borne peptides and hormones are absorbed intact(6). A number of these absorbed peptides and hormones play important developmental roles in the newborn(6).
Epo, the primary hormone responsible for stimulating erythropoiesis throughout life, is produced in response to hypoxia or anemia. Epo present in mammalian milk appears to have biologic effects in suckling animals(7, 8). Erythropoiesis, as measured by elevated Hb and erythrocyte concentrations, was stimulated in suckling rat pups after their mothers were exposed to hypoxia(7). Carmichael et al.(9–12) observed increased erythropoiesis in suckling rat pups after maternal phlebotomy or in pups fed cow's milk supplemented with Epo. In one study, a concentrated human milk filtrate was administered to polycythemic mice and erythropoiesis, as measured by the incorporation of radiolabeled iron into erythrocytes, was observed(13).
Two recent studies present potential mechanisms of gastro-intestinal absorption of Epo. In the first, when adult rats were administered rhEpo rectally with agents that increase rectal mucosal cell membrane permeability, higher serum Epo levels and stimulated erythropoiesis were observed(14). The second study found specific binding of rhEpo to Epo receptor in rat gastric mucosal cells(15).
A recent study described enteral absorption of rhEpo. Serum Epo levels rose after administration of high dose rhEpo enterally to six premature human infants(16). Because the anemia of prematurity, characterized by relative Epo deficiency, is a major complication of premature birth, the physiologic and pharmacologic actions of enterally administered Epo are potentially important. However, no systematic investigation into the physiologic and pharmacologic roles of human milk-borne Epo has been undertaken.
Our hypothesis is that human milk contains significant quantities of Epo that are absorbed intact and have biologic activity in the neonate. As a first step, the objectives of this study are to quantitate the amount of immunoreactive human milk-borne Epo, determine factors that influence milk-borne Epo levels, and determine whether milk-borne Epo survives exposure to neonatal gastric juices under physiologic conditions.
METHODS
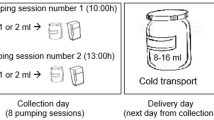
Subjects. Longitudinal and cross-sectional human milk samples were obtained from mothers of infants hospitalized in regional tertiary care newborn intensive care units at The University of Iowa Hospitals and Clinics, Arizona Health Science Center's University Medical Center, and Tucson Medical Center from April 1990 to March 1997. Human milk was collected by mothers via commercial breast pumps, frozen immediately, and stored. Collection date and time were recorded, as were infants' birth date, gestational age, birth weight, and sex. Maternal diagnoses, pregnancy complications, route of delivery (cesarean section versus vaginal), and maternal smoking status were recorded. Aliquots of each collected human milk specimen were thawed and centrifuged 16 000 × g for 5 min. The aqueous fraction of the milk samples was decanted and stored frozen at -20°C for later assay. A subset of these samples was separated as described above, pooled, aliquotted, and used as a “pooled human milk sample.”
Samples of human neonatal gastric juices were collected via indwelling nasogastric tubes from eight infants at 35-38 wk of gestation who were less than 7 d postnatal age. The gastric juices were frozen immediately and stored until assay, when they were cleared of particulate material by centrifugation at 16 000 × g for 5 min. Consent from each institution's Human Subjects Committee was obtained for collection of human milk and gastric juice samples that were intended to be discarded.
Procedures. Aqueous fractions of human milk samples were assayed for total protein concentration by the bicinchoninic acid protein assay (BCA; Pierce, Rockford, IL). The aqueous fraction was also quantitated for Epo concentration via double antibody RIA(17) or with an Epo RIA kit (catalog no. DSL 1100, Diagnostic Systems Laboratory, Webster TX), which utilizes the same rabbit polyclonal Epo antibody source. Serial dilutions of human milk were assayed to evaluate curve fitting of the assay. Interassay coefficients of variation ranged from 3.0 to 9.5%.
We evaluated the susceptibility of milk-borne Epo to degradation by neonatal gastric juices by in vitro simulation of neonatal digestion. Simulations were run for 0 (baseline degradation), 1, and 2 h. The intervals were selected because after human milk feedings, maximal gastric acid proteolytic activity occurs at 1 h(18) and stomach emptying occurs between 1 and 2 h(19). To approximate neonatal gastrointestinal luminal conditions without interfering with proteolytic activity, three incubation buffers were used in standard reaction mixtures(20–22). The buffers included:1) 0.1 M glycine, pH 3.2, to simulate preprandial gastric conditions; 2) 0.1 M maleate at pH 5.8, to simulate postprandial gastric conditions; and 3) 0.01 M Tris, 6.7 mM CaCl2, pH 7.4, to simulate proximal small intestinal conditions.
To ensure that endogenous enzymes were active for each simulation, 50 μL of each of these three pH buffers were preincubated 15 min at 37°C with 50-μL aliquots of each thawed, cleared neonatal gastric juice. To start the reaction, a 50-μL aliquot of a substrate was added and incubated at 37°C (150 μL total volume). The substrate used was 1) protein-free buffer labeled with 125I-Epo (Amersham Corp., Arlington Heights, IL, catalog no. IM.178) to evaluate degradation in the absence of milk; 2) pooled milk aqueous fraction labeled with 125I-Epo to evaluate degradation in milk; or 3) a pooled milk aqueous fraction for RIA. An aliquot of each gastric juice was evaluated at all three pH conditions, on all three substrates, for baseline and 1 and 2 h at 37°C.
At the end of incubation, 5 μL of 1 M Tris, pH 8, buffer was added to stop all reaction mixtures. Radiolabeled reaction mixtures were placed on ice, and 450 μL of cold 20% TCA and 100 μL of 15% BSA were added (12% TCA, 2% BSA, final concentrations in the mixture). TCA was used to precipitate all large proteins, leaving digested products in the supernatant, and BSA was used as a carrier protein to ensure a good separation of pellet(20–22). Reaction mixtures were centrifuged at 16 000 × g for 20 min at 4°C, supernatants were decanted from pellets, and both were counted separately to determine percent degradation. Percent degradation was defined as TCA-soluble counts divided by total counts × 100 for each simulation. The unlabeled reaction mixtures frozen immediately at -70°C until assayed for immunoreactive Epo.
Data analysis. Unless otherwise specified, results are expressed as mean Epo concentration in mU/mL or in mU/mg of protein ± SEM. An α level < 0.05 was considered significant. As serum Epo levels in smokers are higher than in nonsmokers(23), we first compared 15 milk samples obtained from smoking mothers with 15 samples from nonsmokers, matched by postconceptional age at delivery and postpartum day, via the Mann-Whitney U test and observed higher immunoreactive milk-borne Epo concentration in smokers (p < 0.002)(Fig. 1). We then excluded all samples obtained from smoking mothers from further analyses.
Human milk samples were also grouped into 11 postpartum day groups, with between 15 and 68 samples per group. One-way ANOVA was used to determine postpartum changes in human milk Epo concentrations and Epo concentrations per mg of protein. If the F ratio, which is a measure of differences between groups, from this comparison demonstrated a significant difference, a post hoc comparison was performed to determine which comparisons were different. The Sheffé's F procedure was selected as it is intended for complicated comparisons and is generally more conservative than other post hoc comparisons.
The nonparametric Mann-Whitney U test was also used to compare human milk Epo concentrations by mode of delivery and to compare milk-borne Epo to serum Epo concentrations. Because the biologic activity of Epo correlates with the logarithm of its concentration, Figure 2 shows natural logarithmic conversion of Epo levels. Percent degradation and Epo concentrations from 1- and 2-h reaction mixtures were compared with baseline with multiple paired t tests.
Human milk-borne Epo concentrations (mU/mL) by natural log (ln) conversion are displayed on the vertical axis and postpartum day intervals are shown on the horizontal axis. Mean values are indicated by the small black squares and median values by the horizontal line inside the rectangles. The upper and lower horizontal boundaries of the rectangles define the upper and lower quartiles, and the top and bottom of the vertical lines indicate the 90th and 10th percentiles, respectively. The number of samples in each group is listed to the left of the rectangle. Milk-borne Epo varied with postpartum day (F10,398 = 5.82, p < 0.0001). The highest mean Epo concentration (33.8 ± 6.14 mU/mL) was observed during postpartum d 51-134. Sheffé post hoc testing showed that d 51-134 were higher than all other periods, except d 0-1 and d 16-20.
RESULTS
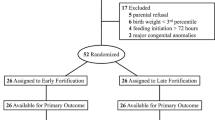
Human milk. We analyzed 409 human milk samples, collected from 58 mothers of premature and term infants (2-40 samples per mother). Measurable immunoreactive Epo levels were observed in early milk (colostrum) and throughout the collection period.
To assess the relative concentrations of milk-borne Epo with serum Epo, several comparison were performed. The mean human milk-borne Epo concentration(11.7 ± 0.75 mU/mL) was within the 2 SD range for serum Epo observed in normal adults (i.e. 3.4-24.8 mU/mL)(24, 25). The mean milk-borne Epo concentration (11.7 ± 0.75 mU/mL) was also lower than the mean serum Epo observed in 66 women(26) in the 1st wk postpartum (35.0 ± 3.23 mU/mL), p < 0.0001. The mean milk-borne Epo concentration was lower than the mean Epo concentration of 109 serum samples from 25 healthy term infants(27) studied longitudinally over the same postpartum period (11.7 ± 0.75 versus 14.2 ± 0.81 mU/mL, respectively), p < 0.0001.
Both milk-borne Epo concentration (F10,398 = 5.84,p < 0.0001) and Epo concentration standardized per mg of protein(F10,376 = 3.13, p < 0.001) changed over time, when grouped by postpartum day. The patterns of postpartum change in Epo concentration and Epo concentration per mg of protein were similar. The highest mean Epo concentration (33.8 ± 6.1 mU/mL) was observed in the last postpartum day group (d 51-134). There was considerable variability between milk from different mothers in Epo concentration(F57,351 = 6.65, p < 0.0001) and Epo concentration standardized per mg protein (F55,331 = 5.23,p < 0.0001). Serum Epo levels rise in mothers after delivery and fall to prepregnancy levels at 2 wk postpartum(26, 28, 29). Of 207 samples obtained in the first 2 wk postpartum, we observed that milk-borne Epo levels from mothers who delivered vaginally were lower than in those who experienced cesarean section or hemorrhage at delivery (9.4 ± 0.77 versus 12.0± 2.19 mU/mL, respectively), p < 0.03.
However, there was no appreciable diurnal pattern of Epo concentration(F11,395 = 1.04, p = 0.41) or Epo concentration per mg of protein (F11,373 = 1.04, p = 0.41). Additionally, the milk-borne Epo concentration and Epo concentration standardized per mg of protein in milk from mothers who delivered prematurely versus at term was similar (p = 0.25 and p = 0.21).
Based on published milk intakes of premature and term infants(30–32), the estimated weekly enteral intake of Epo in premature or term human milk-fed infants was calculated by multiplying mean milk-borne Epo concentration for each postpartum interval by estimated volume of the aqueous fraction of human milk for that interval. Based on the formula, (Epo/mL × mL milk/d) ÷ body weight in kg and using the mean milk-borne Epo levels, the estimated mean weekly intake ranged from 4 U/kg in the first postpartum week to 41 U/kg in the last postpartum interval (d 51-134). Based on individual maternal milk-borne Epo levels, the postpartum days collected, and infant's weight, the maximal weekly intake for an individual infant was estimated to be 136 U/kg.
Gastric juice digestion. We evaluated the capacity of human milk to protect against proteolytic degradation after exposure to term neonatal gastric juices (n = 8). We evaluated Epo degradation in protein-free buffer compared with Epo degradation in the aqueous fraction of milk. Results are shown in Figure 3. Compared with baseline, significant degradation of 125I-Epo in protein-free buffer was observed at pH 3.2 and 7.4 at 1 h (p < 0.0001 and p< 0.05, respectively), and at pH 3.2, 5.8, and 7.4 at 2 h (p < 0.0001, p < 0.02, and p < 0.02, respectively)(Fig. 3A). At maximal degradation in buffer, 55% of labeled Epo remains intact by TCA precipitation. Degradation of125 I-Epo in pooled human milk aqueous fractions at three different pH levels (pH 3.2, 5.8, and 7.4) is also shown (Fig. 3B). No significant differences in degradation were observed at 1 h compared with baseline at the three pH levels, but small increases in degradation were observed at pH 5.8 and 7.4 at 2 h (p < 0.05). At maximal degradation, 80% remains intact. Immunoreactive milk-borne Epo concentrations in pooled human milk are unchanged at 1 and 2 h compared with baseline at the three pH levels (Fig. 3C).
(A) Percent degradation of 125I-Epo in protein-free buffer in the absence of human milk by TCA precipitation is shown. Significant degradation of 125I-Epo occurred at 1 and 2 h after exposure to neonatal gastric juices, compared with baseline at pH 3.2(white bars) and pH 7.4 (black bars), and at 2 h at pH 5.8(hatched bars) (*p < 0.0001, †p < 0.02, and ¶p < 0.0001, respectively), paired t tests. (B) Percent degradation of 125I-Epo in pooled human milk was unchanged after exposure to neonatal gastric juices by TCA precipitation, compared with baseline, except at 2 h at pH 5.8 (hatched bars) and 7.4 (black bars) (*p < 0.05) paired t tests. (C) Immunoreactive milk-borne Epo concentrations in pooled human milk were unchanged compared with baseline (0 h), at 1 and 2 h after exposure to neonatal gastric juices at pH 3.2 (white bars), 5.8 (hatched bars), and 7.4 (black bars), paired t tests.
DISCUSSION
Considerable amounts of Epo are present in human milk. Mean milk-borne Epo concentration is slightly lower than serum Epo concentration from postpartum women or from infants the same postnatal age. Although there is variability in milk-borne Epo concentrations with postpartum days and between different mothers, milk-borne Epo concentrations from mothers of premature infants is not different from from mothers of term infants. Additionally, milk-borne Epo concentration does not vary in a diurnal fashion, despite small diurnal changes previously reported in serum Epo levels(33).
Little is known about the factors that influence milk-borne protein synthesis. Most proteins in human milk originate from two sources: passive transfer from the serum or synthesis from mammary glands(34). The serum protein, albumin is present in human milk at a concentration lower than its serum concentration, whereas lactoferrin and epidermal growth factor are present at higher levels than serum concentration(34, 35). Although milk-borne Epo levels vary with postpartum day and may be influenced by maternal conditions, it is not known where milk-borne Epo originates. Apparent variability in milk-borne Epo concentrations could be due to the nature of the data, which is cross-sectional and longitudinal. However, in animals, milk-borne Epo reflects maternal serum Epo(7, 10, 13). If human milk-borne Epo levels reflect maternal serum levels, we would anticipate finding higher human milk Epo levels in smokers, which we found. Although our study did not determine the level of maternal anemia or maternal serum Epo levels, it is known that Hb levels fall immediately postpartum, followed by a 1-2-wk rise in serum Epo levels and reticulocytes, which return to normal thereafter(26, 28, 29). When we evaluated samples obtained during these first 2 wk postpartum, we observed higher milk-borne Epo levels in mothers with cesarean delivery or hemorrhage who experience greater blood loss, compared with mothers delivering vaginally.
Although we found no studies that describe Epo mRNA production in breast tissue, we speculate that Epo may also be produced in the breast. Generally, milk proteins that are produced and secreted in the mammary gland are expected to constitute the largest proportion of protein in human milk, and to have more postpartum variation than serum proteins that are passively transferred into milk(34). Accumulating evidence supports that cytokine growth factors (IL-6, IL-8, and IL-10) are produced in the mammary gland cells as well(1, 2, 4). Of note, mean milk-borne Epo concentrations were highest in the last postpartum day group(51-134 d), which coincides with the postnatal fall in Hb concentrations in the infant and after maternal peripartum anemia would have resolved. Further studies are necessary to investigate the source of milk-borne Epo.
By TCA precipitation method, Epo in the absence of human milk undergoes significant degradation by neonatal gastric juices, but milk-borne Epo is protected from degradation within the range of gastric and small intestinal pH values. We observed no fall in immunoreactive milk-borne Epo concentration after exposure to gastric juices. Previous work suggests that milk raises the stomach pH postprandially, thus proteins resist gastric digestion by proteolytic enzymes, which require low pH levels for activation(6). This explanation would be consistent with our finding that relatively higher Epo degradation is observed in reaction mixtures containing buffer at pH 3.2, but no human milk proteins. Second, Epo may also be protected from degradation by the presence of antiproteolytic agents known to be present in milk(6). Small intestinal juices were absent from our digestion mixture secondary to difficulty in obtaining human small intestinal juice samples. It is possible that a greater percentage of Epo would be degraded in the presence of small intestinal juices and further studies are necessary.
Although it is known that the primary role of Epo is to stimulate erythropoiesis, potential roles for milk-borne Epo include growth and development effects on the gastrointestinal tract(36). Epo specifically binds to Epo receptor and has physiologic effects on nonerythroid cells, such as other liver hematopoietic cells, spleen cells, megakaryocytes, vascular smooth muscle cells, endothelial cells, and early fetal tissue(14, 37–39). As other growth factors increase small intestine and liver DNA, and accelerate organ maturation in suckling rats(6), similar effects may also be seen with Epo. In support of this speculation, Okada et al.(15) reported that rhEpo may play a physiologic role in gastrointestinal cells by stimulating dose-dependent DNA synthesis and cell proliferation in a rat gastric mucosal cell line, RGM-1.
The finding that Epo administered in the presence of human milk underwent less degradation by neonatal gastric juices suggests that pharmacologic oral Epo dosing in milk may be possible. One previous study administered a high pharmacologic dose of rhEpo (1000 U/kg/d for 10 d) enterally to six premature infants(16). Compared with prestudy values, the authors found higher serum Epo levels 2 h after the first dose (p < 0.02) and before the 10th daily dose (p < 0.01). Although levels rose, suggesting enteral absorption of rhEpo, increases in serum Epo levels were relatively small for the dose administered. Because the rhEpo in this study was administered in buffered albumin solution, independent of milk feedings greater degradation of rhEpo may have occurred. However, an alternative explanation could be that the Epo binds specifically to sites in the gastrointestinal tract and other tissues. Thus, further investigation into enteral versus parenteral Epo administration is warranted.
CONCLUSION
Considerable amounts of Epo are present in human milk. Milk-borne Epo concentrations change with postpartum time, are variable between mothers, but were similar between milk collected from mothers who delivered prematurely and at term, suggesting that Epo levels are regulated by postpartum age and maternal conditions, but not developmental age of the infant. Milk-borne Epo resists degradation and is immunoreactive after exposure to neonatal gastric juices at physiologic pH levels and digestion times. If Epo contained in human milk is not degraded, in vivo weekly estimated enteral milk-borne Epo intake approximates the lower pharmacologic doses currently administered to infants. The scope of these preliminary studies was limited to the questions of the presence and potential proteolytic degradation of Epo. Although these studies do not address the physiologic mechanisms by which Epo is protected from degradation and how Epo exerts its effects, these and other published data support that milk-borne Epo is involved in erythropoiesis. These results support continued investigation into the fate and developmental roles of both physiologic and pharmacologic intakes of Epo in human milk.
Abbreviations
- Epo:
-
erythropoietin
- rhEpo:
-
recombinant human Epo
- TCA:
-
trichloroacetic acid
References
Basolo F, Conaldi PG, Fiore L, Calvo S, Toniolo A 1993 Normal breast epithelial cells produce interleukins 6 and 8 together with tumor-necrosis factor: defective IL6 expression in mammary carcinoma. Int J Cancer 55: 926–930.
Palkowetz KH, Royer CL, Garofalo R, Rudloff HE, Schmalstieg FC, Goldman AS 1994 Production of interleukin-6 and interleukin-8 by human mammary gland epithelial cells. J Reprod Immunol 26: 57–64.
Goldman AS, Chheda S, Keeney SE, Schmalstieg FC, Schanler R 1994 Immunologic protection of the premature newborn by human milk. Semin Perinatol 18: 495–501.
Garofalo R, Chheda S, Mei F, Palkowetz KH, Rudloff HE, Schmalstieg FC, Rassin DK, Goldman AS 1995 Interleukin-10 in human milk. Pediatr Res 37: 444–449.
Koldovský O 1995 Hormones in milk. In: Litwack G(ed) Vitamins and Hormones. Academic Press, New York, pp 77–149.
Koldovský O 1996 The potential physiological significance of milk-borne hormonally active substances for the neonate. J Mamm Gland Biol Neoplasia 1: 317–322.
Grant W 1952 Influence of anoxia of a lactating rat on the blood of normal baby rats. Am J Physiol 171: 728–729.
Hyzy J 1969 Search for erythropoietin in the milk of sheep. Acta Physiol Pol 20: 11–22.
Carmichael RD, Gordon AS, LoBue J 1978 The effects of maternal phlebotomy and orally-administered erythropoietin (Ep) on erythropoiesis in the suckling rat. Biol Neonate 33: 119–131.
Carmichael RD, Gordon AS, LoBue J 1978 Erythropoietic response of hypertransfused neonatal rats suckled by anemic mothers. Anat Rec 191: 227–238.
Carmichael RD, Gordon AS, Lobue J 1986 Effects of the hormone erythropoietin in milk on erythropoiesis in neonatal rats. Endocrinol Exp 20: 167–188.
Carmichael RD, LoBue J, Gordon AS 1992 Neonatal erythropoiesis. I. Peripheral blood erythropoietic parameters: data suggest erythropoietin transfer via maternal milk. Endocr Regul 26: 83–88.
Bielecki M, Przala F, Lazewska M 1972 Level of erythropoietin in the woman milk. Acta Physiol Pol 23: 435–439.
Mizuno A, Ueda M, Kawanishi G 1991 Effects of salicylate and other enhancers on rectal absorption of erythropoietin in rats. J Pharm Pharmacol 44: 570–573.
Okada A, Kinoshita Y, Maekawa T, Hannan MS, Kawanami C, Asahara M, Matsushima Y, Kishi K, Nakata H, Naribayashi Y, Chiba T 1996 Erythropoietin stimulates proliferation of rat-cultured gastric mucosal cells. Digestion 57: 328–332.
Britton JR, Christensen RD 1995 Enteral administration of recombinant erythropoietin to preterm infants. J Perinatol 15: 281–283.
Georgieff MK, Landon MB, Mills MM, Hedlund BE, Faassen AE, Schmidt RL, Ophoven JJ, Widness JA 1990 Abnormal iron distribution in infants of diabetic mothers: Spectrum and maternal antecedents. J Pediatr 117: 455–461.
Yahav J, Carrion V, Lee PC, Lebenthal E 1987 Meal-stimulated pepsinogen secretion in premature infants. J Pediatr 110: 949–951.
Lebenthal E, Siegel M 1985 Understanding gastric emptying: implications for feeding the healthy and compromised infant. J Pediatr Gastroenterol Nutr 4: 1–3.
Britton JR, George-Nascimento C, Koldovský O 1988 Luminal hydrolysis of recombinant human epidermal growth factor in the rat gastrointestinal tract: segmental and developmental differences. Life Sci 43: 1339–1347.
Britton JR, George-Nascimento C, Udall JN, Koldovský O 1989 Minimal hydrolysis of epidermal growth factor by gastric fluid of preterm infants. Gut 30: 327–332.
Britton JR, Koldovský O 1989 Transferrin degradation by gastrointestinal fluids of suckling and weanling rats. J Dev Physiol 11: 57–61.
Widness J, Clemons GK, Garcia JF, Oh W, Schwartz R 1984 Increased immunoreactive erythropoietin in cord serum after labor. Am J Obstet Gynecol 148: 194–196.
Widness JA, Veng-Pedersen P, Peters C, Pereira LM, Schmidt RL, Lowe LS 1996 Erythropoietin pharmacokinetics in premature infants: developmental, non-linearity, and treatment effects. J Appl Physiol 80: 140–148.
Diagnostic Systems Laboratory 1993 Erythropoietin: Radioimmunoassay kit for the quantitative measurement of erythropoietin in serum or plasma (DSL-1100). Diagnostic Systems Laboratory, Webster, TX, p 12
Beguin Y, Lipscei G, Oris R, Thoumsin G, Fillet G 1990 Serum immunoreactive erythropoietin during pregnancy and in the early postpartum. Br J Haematol 76: 545–549.
Kling PJ, Schmidt RL, Roberts RA, Widness JA 1996 Serum erythropoietin levels during infancy: associations with erythropoiesis. J Pediatr 128: 791–796.
Huch R, Huch A 1993 Maternal and fetal erythropoietin: physiologic aspects and clinical significance. Ann Med 25: 289–293.
Widness J, Clemons G, Garcia J, Schwartz R 1984 Plasma immunoreactive erythropoietin in normal women studied sequentially during and after pregnancy. Am J Obstet Gynecol 149: 646–650.
DeCarvalho M, Robertson S, Merkayz R, Klaus M 1982 Milk intake and frequency of feeding in breast fed infants. Early Hum Dev 7: 155–163.
Dewey KG, Lovelady CA, Nommsen-Rivers LA, McCrory MA, Lonnerdal B 1994 A randomized study of the effects of aerobic exercise by lactating women on breast-milk volume and composition. N Engl J Med 330: 449–453.
Schanler RJ 1995 Suitability of human milk for the low-birthweight infant. Clin Perinatol 22: 207–222.
Cahan C, Decker MJ, Arnold JL, Washington LH, Veldhuis JD, Goldwasser E, Strohl KP 1992 Diurnal variations in serum erythropoietin levels in healthy subjects and sleep apnea patients. J Appl Physiol 72: 2112–2117.
Lonnerdal B, Atkinson S 1995 Human Milk Proteins. In: Jensen R (ed) Handbook of Milk Composition. Academic Press, San Diego, pp 351–368.
Moran JR, Courtney ME, Orth DN, Vaughan R, Coy S, Mount CD, Sherrell BJ, Greene HL 1983 Epidermal growth factor in human milk: daily production and diurnal variation during early lactation in mothers delivering at term and at premature gestation. J Pediatr 103: 402–405.
Pereira GR 1995 Nutritional care of the extremely premature infant. Clin Perinatol 22: 61–75.
D'Andrea AD, Zon LI 1990 Erythropoietin receptor, Subunit structure and activation. J Clin Invest 86: 681–687.
Winkelmann JC 1992 The human erythropoietin receptor. Int J Cell Cloning 10: 254–261.
Li Y, Juul SE, Morris-Wiman JA, Calhoun D, A, Christensen RD 1996 Erythropoietin receptors are expressed in the central nervous system of mid-trimester human fetuses. Pediatr Res 40: 376–380.
Acknowledgements
The authors thank John A. Widness, M.D., and Karen J. Johnson, R.N., at the University of Iowa, and the NICU nursing staffs at University Medical Center and Tucson Medical Center, Tucson, for technical support and assistance in collection of human milk samples.
Author information
Authors and Affiliations
Additional information
Supported in part by Arizona Disease Control Research Commission 9421(P.J.K.), 1995 Undergraduate Honors Research Grant, University of Arizona(T.M.S.), Sigma Xi Undergraduate Research Grant (T.M.S.), and Program Project National Institutes of Health HD 26013 (A.F.P., O.K.).
Rights and permissions
About this article
Cite this article
Kling, P., Sullivan, T., Roberts, R. et al. Human Milk as a Potential Enteral Source of Erythropoietin. Pediatr Res 43, 216–221 (1998). https://doi.org/10.1203/00006450-199802000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199802000-00010
This article is cited by
-
Robust increases in erythropoietin production by the hypoxic fetus is a response to protect the brain and other vital organs
Pediatric Research (2018)
-
Breast feeding in infancy and arterial endothelial function later in life. The Cardiovascular Risk in Young Finns Study
European Journal of Clinical Nutrition (2009)
-
Host Factors in Amniotic Fluid and Breast Milk that Contribute to Gut Maturation
Clinical Reviews in Allergy & Immunology (2008)
-
Protective effects of recombinant human granulocyte colony stimulating factor in a rat model of necrotizing enterocolitis
Pediatric Surgery International (2006)
-
Hematologic Abnormalities in Severe Neonatal Necrotizing Enterocolitis: 25 Years Later
Journal of Perinatology (2003)