Abstract
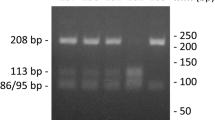
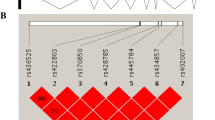
Pelvic organ prolapse (POP) represents a urologic and gynecological disease, the development of which is governed both by environmental and genetic factors. We describe the results of our association study of polymorphic variants of genes involved in the assembly of elastic fibrils, namely, the lysyl oxidase-like protein 1 (LOXL1) and fibulin-3 (FBLN3) genes. We revealed an association of the rs2304719-T allele and rs2165241(C)–rs2304719(T)–rs893821(T) haplotype of the LOXL1 gene with an increased risk of POP development, as well as a weak association with the disease of the rs3791660-C allele and the rs3791679(T)–rs1367228(A)–rs3791660(C)–rs2033316(A) haplotype of the FBLN3 gene.
Similar content being viewed by others
References
Buyanova, S.N., Shchukina, N.A., and Zhuravleva, A.S., Efficiency of using mesh prostheses in complicated forms of genital prolapse, Ross. Vestn. Akush.-Ginekol., 2009, no. 1, pp. 76–81.
Hendrix, S.L., Clark, A., Nygaard, I., et al., Pelvic organ prolapse in the women’s health initiative: gravity and gravidity, Am. J. Obstet. Gynecol., 2002, vol. 186, no. 6 pp. 1160–1166.
Whitcomb, E.L., Rortveit, G., Brown, J.S., et al., Racial differences in pelvic organ prolapse, Obstet. Gynecol., 2009, vol. 114, no. 6, pp. 1271–1277.
Adamyan, L.V., Smol’nova, T.Yu., and Sidorov, V.V., Laser Doppler flowmetry in the study of microvasculature in patients with neoplastic diseases of the genitals, Vopr. Ginekol. Akush. Perinatal., 2006, vol. 5, no. 5, pp. 34–39.
Krasnopol’skii, V.I., Buyanova, S.N., Shchukina, N.A., et al., Surgical treatment of patients with prolapse of internal genital organs, and prevention of vaginal dome prolapse after hysterectomy, Ross. Vestn. Akush.Ginekol., 2006, no. 6(4), pp. 66–71.
Sukhikh, G.T., Danilov, A.Yu., and Botasheva, D.A., The role of immunohistochemical and genetic factors in the etiology refinement and pathogenesis of genital prolapse in women, Ross. Vestn. Akush.-Ginekol., 2012, no. 2, pp. 47–50.
Kamoeva, C.V., Savchenko, T.N., Ivanova, A.V., and Abaeva, Kh.A., Modern genetic aspects of pelvic organ prolapse in women, Akush. Ginekol. Reprod., 2013, vol. 7, no. 1, pp. 17–21.
Drewes, P.G., Yanagisawa, H., Starcher, B., et al., Pelvic organ prolapse in fibulin-5 knockout mice: pregnancy changes in elastic fiber homeostasis in mouse vagina, Am. J. Pathol., 2007, vol. 170, no. 2, pp. 578–589.
Liu, X., Zhao, Y., Pawlyk, B., et al., Failure of elastic fiber homeostasis leads to pelvic floor disorders, Am. J. Pathol., 2006, vol. 168, no. 2, pp. 519–528.
McLaughlin, P.J., Bakall, B., Choi, J., et al., Lack of fibulin-3 causes early aging and herniation, but not macular degeneration in mice, Hum. Mol. Genet., 2007, vol. 16, no. 24, pp. 3059–3070.
Rahn, D.D., Acevedo, J.F., Roshanravan, S., et al., Failure of pelvic organ support in mice deficient in fibulin-3, Am. J. Pathol., 2009, vol. 174, no. 1, pp. 206–215.
Alperin, M., Debes, K., Abramowitch, S., et al., LOXL1 deficiency negatively impacts the biomechanical properties of the mouse vagina and supportive tissues, Int. Urogynecol. J. Pelvic. Floor. Dysfunct., 2008, vol. 19, no. 7, pp. 977–986.
Ferrell, G., Lu, M., Stoddard, P., et al., A single nucleotide polymorphism in the promoter of the LOXL1 gene and its relationship to pelvic organ prolapse and preterm premature rupture of membranes, Reprod. Sci., 2009, vol. 16, no. 5, pp. 438–446.
Hamajima, N., PCR–CTPP: a new genotyping technique in the era of genetic epidemiology, Expert Rev. Mol. Diagn., 2001, vol. 1, no. 1, pp. 119–123.
Trifonova, E.A., Eremina, E.R., Urnov, F.D., and Stepanov, V.A., The genetic diversity and structure of linkage disequilibrium of the MTHFR gene in populations of Northern Eurasia, Acta Nat., 2012, vol. 4, no. 1(12), pp. 55–71.
http://hapmap.ncbi.nlm.nih.gov/
http://bioinfo.iconcologia.net/index.php?module= Snpstats
Rortveit, G., Brown, J.S., Thom, D.H., et al., Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort, Obstet. Gynecol., 2007, vol. 109, no. 6, pp. 1396–1403.
Barrett, J., Fry, B., Maller, J., and Daly, M.J., Haploview: analysis and visualization of LD and haplotype maps, Bioinformatics, 2005, vol. 21, no. 2, pp. 263–265.
Memon, H.U. and Handa, Vl.., Vaginal childbirth and pelvic floor disorders, Women’s Health (London), 2013, vol. 9, no. 3, pp. 65–77.
Nygaard, I., Barber, M.D., Burgio, K.L., et al., Prevalence of symptomatic pelvic floor disorders in US women, JAMA, 2008, vol. 300, no. 11, pp. 1311–13163.
Mant, J., Painter, R., and Vessey, M., Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study, Br. J. Obstet. Gynaecol., 1997, vol. 10, no. 5, pp. 579–585.
Handa, Vl.., Blomquist, J.L., McDermott, K.C., et al., Pelvic floor disorders after vaginal birth: effect of episiotomy, perineal laceration, and operative birth, Obstet. Gynecol., 2012, vol. 119, no. 2, Pt. 1, pp. 233–239.
Lince, S.L., van Kempen, L.C., Vierhout, M.E., and Kluivers, K.B., A systematic review of clinical studies on hereditary factors in pelvic organ prolapse, Int. Urogynecol. J., 2012, vol. 23, no. 10, pp. 1327–1336.
Zhao, B.H. and Zhou, J.H., Decreased expression of elastin, fibulin-5 and lysyl oxidase-like 1 in the uterosacral ligaments of postmenopausal women with pelvic organ prolapse, J. Obstet. Gynaecol. Res., 2012, vol. 38, no. 6, pp. 925–931.
Wang, X., Li, Y., and Chen, J., Differential expression profiling of matrix metalloproteinases and tissue inhibitors of metalloproteinases in females with or without pelvic organ prolapse, Mol. Med. Rep., 2014, vol. 10, no. 4, pp. 2004–2008.
Cartwright, R., Kirby, A.C., Tikkinen, K.A., et al., Systematic review and metaanalysis of genetic association studies of urinary symptoms and prolapse in women, Am. J. Obstet. Gynecol., 2015, vol. 212, no. 2, p. 199. e1-24.
Zhang, Y. and Marmorstein, L.Y., Focus on molecules: fibulin-3 (EFEMP1), Exp. Eye Res., 2010, vol. 90, no. 3, pp. 374–375.
Pass, H.I., Levin, S.M., Harbut, M.R., et al., Fibulin-3 as a blood and effusion biomarker for pleural mesothelioma, N. Engl. J. Med., 2012, vol. 367, no. 15, pp. 1417–1427.
Xu, S., Yang, Y., Sun, Y.B., et al., Role of fibulin-3 in lung cancer: in vivo and in vitro analyses, Oncol. Rep., 2014, vol. 31, no. 1, pp. 79–86.
Zhang, T., Xie, X., Cao, G., et al., Malattia leventinese/Doyne honeycomb retinal dystrophy in a Chinese family with mutation of the EFEMP1 gene, Retina, 2014, vol. 34, no. 12, pp. 2462–2471.
Northington, G.M., Fibulin-5: two for the price of one maintaining pelvic support, J. Clin. Invest., 2011, vol. 121, no. 5, pp. 2048–2059.
Ji, Q.S., Qi, B., Wen, Y.C., et al., The association of LOXL1 polymorphisms with exfoliation syndrome/glaucoma: meta-analysis, Int. J. Ophthalmol., 2015, vol. 8, no. 1, pp. 148–156.
Ramamurthi, A., Venkataraman, L., Lenis, A.T., et al. Induced regenerative elastic matrix repair in LOXL1 knockout mouse cell cultures: towards potential therapy for pelvic organ prolapse, J. Tissue Sci. Eng., 2012, vol. 3, no. 3, p. 120.
Takacs, P., Nassiri, M., Candiotti, K., et al., Differential expression of fibulins in the uterosacral ligaments of women with uterine prolapse, Arch. Gynecol. Obstet., 2010, vol. 282, no. 4, pp. 389–394.
Khadzhieva, M.B., Kamoeva, S.V., Chumachenko, A.G., et al., Fibulin-5 (FBLN5) gene polymorphism is associated with pelvic organ prolapse, Maturitas, 2014, vol. 78, pp. 287–292.
Makarov, O.V., Kamoeva, S.V., Khadzhieva, M.B., et al., Relation of FBLN5 gene polymorphism with the risk of pelvic organ prolapse in women with injuries of soft birth canal, Akush. Ginekol., 2015, no. 1, pp. 42–50.
Author information
Authors and Affiliations
Corresponding author
Additional information
Original Russian Text © M.B. Khadzhieva, S.V. Kamoeva, A.V. Ivanova, S.K. Abilev, L.E. Salnikova, 2015, published in Genetika, 2015, Vol. 51, No. 10, pp. 1191–1198.
Rights and permissions
About this article
Cite this article
Khadzhiev, M.B., Kamoeva, S.V., Ivanova, A.V. et al. Elastogenesis-related gene polymorphisms and the risk of pelvic organ prolapse development. Russ J Genet 51, 1026–1032 (2015). https://doi.org/10.1134/S1022795415100087
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1022795415100087