Abstract
BACKGROUND: Relatively few studies have directly addressed the interaction dynamics and consequences of a companion’s presence in the medical visit, and their findings have been contradictory.
OBJECTIVES: To examine how patient’s contribution to the medical dialogue, with or without the presence of a visit companion, is related to the perception of the medical visit as patient-centered.
DESIGN: Observational study using pre- and postvisit questionnaires and audiotape recording of medical visits.
PARTICIPANTS: One hundred and fifty-five patients aged 65 or over; 63 in medical visits that included the presence of a companion and 82 in visits that did not include a companion.
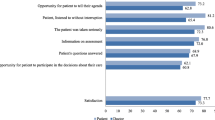
MAIN OUTCOME MEASURE: Patient ratings of visit patient-centeredness.
RESULTS: Long visits (greater than 10 minutes long) and visits in which patients were verbally active were rated as more patient-centered by patients than other visits. Since patients were generally less verbally active in visits that included a companion, accompanied visits, especially if they were less than 10 minutes long, received lower patient-centered ratings than others. The presence of a companion was not related to length of the visit, suggesting that the verbal activity of the companion was off-set by decreased verbal activity of the patient.
CONCLUSIONS: Our results have suggested that patients are more likely to perceive their physician and visit as patient-centered when they have an opportunity to engage directly in the medical dialogue. A minimal amount of “talk-time” for patients themselves should be safe-guarded even in a short visit, when a companion is present.
Similar content being viewed by others
References
Little P, Everitt H, Williamson I, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323:908–11.
Mead N, Bower P. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ Couns. 2002;48:51–61.
Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33.
Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49:796–804.
Stewart M, Brown JB, Weston WW, McWhinney IR, McWilliam CL, Freeman TR. Patient-Centered Medicine: TRANSFORMING the Clinical Method. Thousand Oaks, CA: Sage Publications; 1995.
Adelman RD, Greene MG, Charon R. The physician-elderly patient-companion triad in the medical encounter: the development of a conceptual framework and research agenda. Gerontologist. 1987;27:729–34.
Beisecker AE. The influence of a companion on the doctor-elderly patient interaction. Health Commun. 1989;1:55–70.
Brown JB, Brett P, Stewart M, Marshall JN. Roles and influence of people who accompany patients on visits to the doctor. Can Fam Physician. 1998;44:1644–50.
Prohaska TR, Glasser M. Patients’ views of family involvement in medical care decisions and encounters. Res Aging. 1996;18:52–69.
Clayman ML, Roter D, issow LS, Bandeen-Roche K. Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Soc Sci Med. 2005;60:1583–91.
Ishikawa H, Roter DL, Yamazaki Y, Takayama T. Physician-elderly patient-companion communication in Japanese geriatric encounters. Soc Sci Med. 2005;60:2307–20.
Schilling LM, Scatena L, Steiner JF, Albertson GA, Lin CT, Cyran L, et al. The third person in the room: frequency, role, and influence of companions during primary care medical encounters. J Fam Pract. 2002;51:685–90.
Labrecque MS, Blanchard CG, Ruckdeschel JC, Blanchard EB. The impact of family presence on the physician-cancer patient interaction. Soc Sci Med. 1991;33:1253–61.
Botelho RJ, Lue BH, Fiscella K. Family involvement in routine health care: a survey of patients’ behaviors and preferences. J Fam Pract. 1996;42:572–6.
Baker PS, Yoels WC, Clair JM, Allman RM. Laughter in triadic geriatric medical encounters: a transcript-based analysis. Social Perspectives Emotion. 1997;4:179–207.
Coe RM, Prendergast RM. Research note: the formation of coalitions: interaction strategies in triads. Sociol Health Illness. 1985;7:237–47.
Greene MG, Adelman RD, Friedmann E, Charon R. Older patient satisfaction with communication during an initial medical encounter. Soc Sci Med. 1994;38:1279–88.
Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol. 1998;51:1037–44.
Ishikawa H, Takayama T, Yamazaki Y, Seki Y, Katsumata N. Physician-patient communication and patient satisfaction in Japanese cancer consultations. Soc Sci Med. 2002;55:301–11.
Wissow LS, Roter D, Larson SM, et al. Mechanisms behind the failure of residents’ longitudinal primary care to promote disclosure and discussion of psychosocial issues. Arch Pediatr Adolesc Med. 2002;156:685–92.
Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30.
Greenfield S, Kaplan S, Ware JE, Jr. Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med. 1985;102:520–8.
Mead N, Bower P, Hann M. The impact of general practitioners’ patient-centredness on patients’ post-consultation satisfaction and enablement. Soc Sci Med. 2002;55:283–99.
Wolf KH. The Sociology of Georg Simmel. New York: Free Press; 1950.
Haug MR, Ory MG. Issues in elderly patient-provider interactions. Res Aging. 1987;9:3–44.
Stoeckle JD. Encounters Between Patients and Doctors. Cambridge, MA: The MIT Press; 1987.
Coe RM, Prendergast CG, Psathas G. Strategies for obtaining compliance with medications regimens. J Am Geriatr Soc. 1984;32:589–94.
Ishikawa H, Roter DL, Yamazaki Y, Hashimoto H, Yano E. Patient perceptions of companion helpfulness during geriatric medical visits. Patient Educ Couns (forthcoming).
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no conflicts of interest to declare for this article or this research.
This research was supported by a grant from the Pfizer health research foundation.
Rights and permissions
About this article
Cite this article
Ishikawa, H., Hashimoto, H., Roter, D.L. et al. Patient contribution to the medical dialogue and perceived patient-centeredness. J GEN INTERN MED 20, 906–910 (2005). https://doi.org/10.1111/j.1525-1497.2005.0200.x
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1111/j.1525-1497.2005.0200.x



