-
PDF
- Split View
-
Views
-
Cite
Cite
Luvena Rodrigues, Saudamini V Nesargi, Maneka Fernandes, A Shashidhar, Suman P N Rao, Swarnarekha Bhat, Analgesic Efficacy of Oral Dextrose and Breast Milk during Nasopharyngeal Suctioning of Preterm Infants on CPAP: A Blinded Randomized Controlled Trial, Journal of Tropical Pediatrics, Volume 63, Issue 6, December 2017, Pages 483–488, https://doi.org/10.1093/tropej/fmx017
Close - Share Icon Share
Abstract
Continuous positive airway pressure (CPAP) requires nasopharyngeal suctioning for airway patency, which is painful. Other procedures have used breast milk and 25% dextrose as analgesics. We aimed to compare their analgesic efficacy during nasopharyngeal suctioning in preterm neonates on CPAP. In this blinded randomized controlled trial, babies received 25% dextrose or breast milk orally. Pain before, during and after was assessed using the Premature Infant Pain Profile (PIPP) score. Analysis was done for 40 babies. The mean PIPP score in the 25% dextrose group during the procedure was 11.25 ± 2.73 and 13.2 ± 2.55 (p = 0.02) with the intervention and without. In the breast milk group the PIPP score during the procedure was 11.35 ± 3.05 and 13.45 ± 3.27 (p = 0.04); this difference persisted even after the procedure. There was no significant difference between the interventions. Both interventions significantly reduce pain. The analgesic effect of breast milk was sustained.
INTRODUCTION
Continuous positive airway pressure (CPAP) is commonly used in neonatal intensive care units (NICUs) and often prevents the need for endotracheal intubation [1]. Babies on CPAP need pharyngeal suctioning; however, suctioning practices are highly variable [2]. Suctioning is a painful procedure and produces changes in vital parameters in preterm neonates [3, 4]. Newborns are subjected to numerous painful procedures during their stay in the NICU [5–7]. This has a deleterious long-term effect on the developing brain [8–10]. The guidelines for management of procedural pain do not have any specific recommendations for nasopharyngeal suctioning [11]. Few studies have looked at analgesia during suctioning and have tried 20% dextrose [12], oral glucose with facilitated tuck [3] and opioids [13]. As breast milk and dextrose are effective in ameliorating pain arising from other procedures (heel lance [14], retinopathy of prematurity (ROP) screening [15] and venepuncture [16]), we aimed to compare their efficacy as analgesics during nasopharyngeal suctioning.
METHODS
Study design
This was a prospective blinded randomized controlled trial. It was done at St. Johns Medical College Hospital in Bangalore, a tertiary care hospital. The study was approved by the institutional ethics committee.
Patients
Inclusion criteria were preterm babies (< 37 weeks of gestation) who required CPAP. Gestation was assessed either by a first trimester ultrasound or by the New Ballard Score. Neonates with perinatal asphyxia (Apgar score at 5 min < 5/10), neuromuscular disorders, receiving analgesics, sedatives or anticonvulsants and those who were nil per os were excluded from the study. Written informed consent was taken from either parent.
Randomization and masking: Eligible neonates were randomized to one of two groups (A and B). Babies in group A received 25% dextrose orally during the first suctioning while babies in group B received expressed breast milk (EBM) orally. No intervention was done during the second suctioning. Thus, babies served as their own controls. Randomization was done using block randomization in block sizes of 10, using a computer-generated random number table. Randomization was done by one of the investigators (S.N.). Allocation concealment was done using sequentially numbered opaque sealed envelopes. Patient enrolment and assignment were done by co-investigators (M.F. and S.A.). The primary investigator (L.R.) was blinded to the intervention. Blinding was ensured by preventing L.R. from being in the room when the intervention was done. She was not involved in the randomization, video recording or noting of vital parameters. She was responsible for the scoring of the videos and thus determining the Premature Infant Pain Profile (PIPP) score.
Procedures
After inclusion in the study, just before the suctioning, a video was taken to determine the baseline state of the baby. Heart rate and saturations were noted. The baby then received either 25% dextrose or EBM at 0.3 ml/kg orally by a paladai 3 min before suction was done. This was done by a nurse not involved in the randomization or the analysis. Nasal prongs were removed for suction. If the saturations decreased below 85%, free flow oxygen was administered. Videotaping of the babies’ face was done before, during and after the procedure for 5 min. During this time, minimum saturations and maximum heart rates (Phillips, Masimo) were recorded. All babies were nested during the procedure. For the next suction, the same procedure was followed, except that the babies received standard care (no milk or 25% dextrose).
There was a gap of at least 24 h between the first and second suctioning. Suctioning was done every 8 hourly as per unit protocol or when medically indicated (visible secretions or desaturations). Outcomes: The primary outcome measure was pain as assessed by the PIPP score. This score incorporates maximum heart rate, minimum saturations, gestational age and three facial reactions—presence of nasolabial furrow, brow bulge and eye squeeze. It is graded as mild (<6), moderate (6–12) and severe (>12) [17]. The score was assessed at baseline (before starting the procedure), during the procedure and at 1 and 5 min after the procedure. Each video was replayed thrice to assess each of the facial reactions. To avoid inter-observer variation, the analysis of pain was done by the same observer (L.R.). A co-investigator (S.N.) validated 10% of the videos. Both investigators had given the same score for these videos.
Statistical analysis
At the time the study was designed, we could not find a similar study from which sample size could be calculated. Hence, a pilot (n = 10) was done. The mean PIPP score with breast milk or 25% dextrose was 11 ± 2.6 and during standard care was 12.7 ± 1.8. Based on this, a sample size of 19 babies per group was calculated with a power of 90% and a 5% level of significance. The PIPP score between the groups was compared using the ‘t’ test. Comparisons were done between groups A and B.
Comparisons were also done between 25% dextrose and breast milk vs. standard care (paired ‘t’ test).
All analysis was done using SPSS software (version 13). A p-value of <0.05 was taken as significant.
Research in context: With the advent of CPAP, babies often avoid the need for intubation; however, the pain associated with suctioning has not been adequately addressed. While both breast milk and dextrose are effective analgesics for other painful procedures, we do not know their efficacy in nasopharyngeal suctioning.
Evidence before this study:
Newborns perceive pain which has a detrimental effect on long-term neurodevelopment.
Nasopharyngeal suctioning is painful.
Breast milk and sweet solutions decrease pain.
There is some concern about the long-term use of repeated doses of sucrose.
Added value of this study: Both breast milk and dextrose 25% can be used to reduce pain caused by nasopharyngeal suctioning for babies on CPAP. Breast milk had a longer period of analgesia and is known to be safe.
Implications of all the available evidence: CPAP certainly appears to be painful, particularly during suctioning, and breast milk is a safe and effective analgesic.
RESULTS
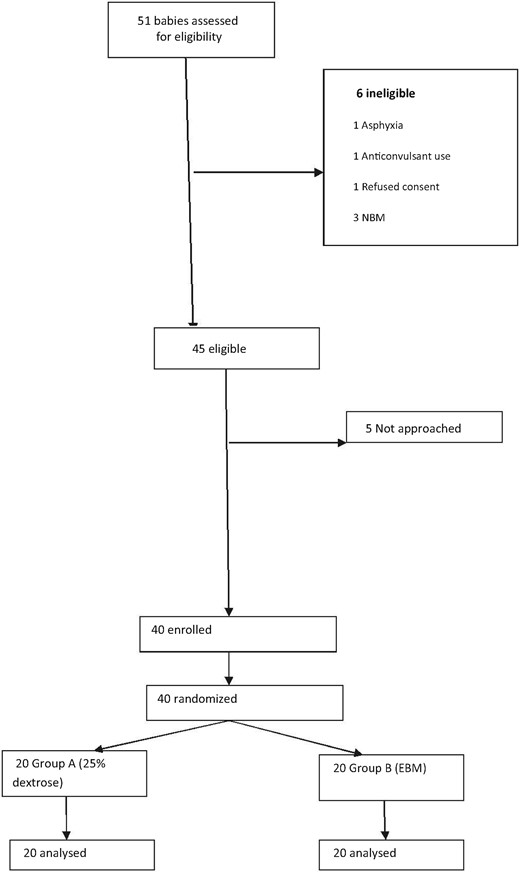
We had a total of 40 babies (20 in each arm) included between July and December 2010 (Figure 1).
Table 1 shows baseline characteristics; there was no significant difference between the two groups. Table 2 shows PIPP score outcome. There was no significant difference between 25% dextrose and breast milk in reducing pain. Table 3 depicts PIPP score in 25% dextrose vs. standard care; when compared with no intervention (standard care), 25% dextrose significantly decreased pain during the suction. In standard care, babies experienced severe pain during suctioning. Table 4 shows PIPP score in breast milk vs. standard care; breast milk significantly decreased pain during and 1 min and 5 min after the procedure.
Baseline characteristics
| Characteristics . | Group A—25% dextrose . | Group B—breast milk . |
|---|---|---|
| N =20 (mean ± SD) . | N =20 (mean ± SD) . | |
| Birth weight (g) | 1415 ± 367.2 | 1481 ± 404.36 |
| Gestation (week) | 31.5 ± 1.82 | 31.65 ± 1.95 |
| Male % | 30% | 45% |
| Duration of ventilation before procedure (hours) | 8.9 ± 17.05 | 32.2 ± 64.2 |
| Amount of feeds baby on (ml/kg) | 19.5 ± 10.5 | 19 ± 12.94 |
| Caesarean section % | 85% | 90% |
| Characteristics . | Group A—25% dextrose . | Group B—breast milk . |
|---|---|---|
| N =20 (mean ± SD) . | N =20 (mean ± SD) . | |
| Birth weight (g) | 1415 ± 367.2 | 1481 ± 404.36 |
| Gestation (week) | 31.5 ± 1.82 | 31.65 ± 1.95 |
| Male % | 30% | 45% |
| Duration of ventilation before procedure (hours) | 8.9 ± 17.05 | 32.2 ± 64.2 |
| Amount of feeds baby on (ml/kg) | 19.5 ± 10.5 | 19 ± 12.94 |
| Caesarean section % | 85% | 90% |
There was no significant difference between the two groups (p > 0.05).
Baseline characteristics
| Characteristics . | Group A—25% dextrose . | Group B—breast milk . |
|---|---|---|
| N =20 (mean ± SD) . | N =20 (mean ± SD) . | |
| Birth weight (g) | 1415 ± 367.2 | 1481 ± 404.36 |
| Gestation (week) | 31.5 ± 1.82 | 31.65 ± 1.95 |
| Male % | 30% | 45% |
| Duration of ventilation before procedure (hours) | 8.9 ± 17.05 | 32.2 ± 64.2 |
| Amount of feeds baby on (ml/kg) | 19.5 ± 10.5 | 19 ± 12.94 |
| Caesarean section % | 85% | 90% |
| Characteristics . | Group A—25% dextrose . | Group B—breast milk . |
|---|---|---|
| N =20 (mean ± SD) . | N =20 (mean ± SD) . | |
| Birth weight (g) | 1415 ± 367.2 | 1481 ± 404.36 |
| Gestation (week) | 31.5 ± 1.82 | 31.65 ± 1.95 |
| Male % | 30% | 45% |
| Duration of ventilation before procedure (hours) | 8.9 ± 17.05 | 32.2 ± 64.2 |
| Amount of feeds baby on (ml/kg) | 19.5 ± 10.5 | 19 ± 12.94 |
| Caesarean section % | 85% | 90% |
There was no significant difference between the two groups (p > 0.05).
PIPP scores outcome
| PIPP score . | Group A—25% dextrose (Mean ± SD) . | Group B— breast milk (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.75 ± 1.16 | 2.8 ± 1.24 | 0.89 |
| During | 11.25 ± 2.73 | 11.35 ± 3.05 | 0.91 |
| 1 min | 7.15 ± 3.45 | 6.6 ± 3.27 | 0.60 |
| 5 min | 4.6 ± 1.85 | 4.15 ± 1.87 | 0.44 |
| PIPP score . | Group A—25% dextrose (Mean ± SD) . | Group B— breast milk (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.75 ± 1.16 | 2.8 ± 1.24 | 0.89 |
| During | 11.25 ± 2.73 | 11.35 ± 3.05 | 0.91 |
| 1 min | 7.15 ± 3.45 | 6.6 ± 3.27 | 0.60 |
| 5 min | 4.6 ± 1.85 | 4.15 ± 1.87 | 0.44 |
There was no significant difference between 25% dextrose and breast milk in reducing pain.
PIPP scores outcome
| PIPP score . | Group A—25% dextrose (Mean ± SD) . | Group B— breast milk (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.75 ± 1.16 | 2.8 ± 1.24 | 0.89 |
| During | 11.25 ± 2.73 | 11.35 ± 3.05 | 0.91 |
| 1 min | 7.15 ± 3.45 | 6.6 ± 3.27 | 0.60 |
| 5 min | 4.6 ± 1.85 | 4.15 ± 1.87 | 0.44 |
| PIPP score . | Group A—25% dextrose (Mean ± SD) . | Group B— breast milk (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.75 ± 1.16 | 2.8 ± 1.24 | 0.89 |
| During | 11.25 ± 2.73 | 11.35 ± 3.05 | 0.91 |
| 1 min | 7.15 ± 3.45 | 6.6 ± 3.27 | 0.60 |
| 5 min | 4.6 ± 1.85 | 4.15 ± 1.87 | 0.44 |
There was no significant difference between 25% dextrose and breast milk in reducing pain.
PIPP score in 25% dextrose vs. standard care
| PIPP score . | 25% dextrose (Mean ± SD) . | Standard care (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.75 ± 1.16 | 3.05 ± 1.09 | 0.41 |
| During | 11.25 ± 2.73 | 13.2 ± 2.55 | 0.02 |
| 1 min | 7.15 ± 3.45 | 8.65 ± 3.69 | 0.19 |
| 5 min | 4.6 ± 1.85 | 5.75 ± 2.69 | 0.12 |
| PIPP score . | 25% dextrose (Mean ± SD) . | Standard care (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.75 ± 1.16 | 3.05 ± 1.09 | 0.41 |
| During | 11.25 ± 2.73 | 13.2 ± 2.55 | 0.02 |
| 1 min | 7.15 ± 3.45 | 8.65 ± 3.69 | 0.19 |
| 5 min | 4.6 ± 1.85 | 5.75 ± 2.69 | 0.12 |
When compared with no intervention (standard care), 25% dextrose significantly decreased pain during the suction. In standard care, babies experienced severe pain during suctioning.
PIPP score in 25% dextrose vs. standard care
| PIPP score . | 25% dextrose (Mean ± SD) . | Standard care (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.75 ± 1.16 | 3.05 ± 1.09 | 0.41 |
| During | 11.25 ± 2.73 | 13.2 ± 2.55 | 0.02 |
| 1 min | 7.15 ± 3.45 | 8.65 ± 3.69 | 0.19 |
| 5 min | 4.6 ± 1.85 | 5.75 ± 2.69 | 0.12 |
| PIPP score . | 25% dextrose (Mean ± SD) . | Standard care (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.75 ± 1.16 | 3.05 ± 1.09 | 0.41 |
| During | 11.25 ± 2.73 | 13.2 ± 2.55 | 0.02 |
| 1 min | 7.15 ± 3.45 | 8.65 ± 3.69 | 0.19 |
| 5 min | 4.6 ± 1.85 | 5.75 ± 2.69 | 0.12 |
When compared with no intervention (standard care), 25% dextrose significantly decreased pain during the suction. In standard care, babies experienced severe pain during suctioning.
PIPP score in breast milk vs. standard care
| PIPP score . | Breast milk (Mean ± SD) . | Standard care (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.8 ± 1.24 | 3.3 ± 1.17 | 0.19 |
| During | 11.35 ± 3.05 | 13.45 ± 3.27 | 0.04 |
| 1 min | 6.6 ± 3.27 | 9.1 ± 3.23 | 0.02 |
| 5 min | 4.15 ± 1.87 | 6.3 ± 3.06 | 0.01 |
| PIPP score . | Breast milk (Mean ± SD) . | Standard care (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.8 ± 1.24 | 3.3 ± 1.17 | 0.19 |
| During | 11.35 ± 3.05 | 13.45 ± 3.27 | 0.04 |
| 1 min | 6.6 ± 3.27 | 9.1 ± 3.23 | 0.02 |
| 5 min | 4.15 ± 1.87 | 6.3 ± 3.06 | 0.01 |
Breast milk significantly decreased pain during and 1 min and 5 min after the procedure.
PIPP score in breast milk vs. standard care
| PIPP score . | Breast milk (Mean ± SD) . | Standard care (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.8 ± 1.24 | 3.3 ± 1.17 | 0.19 |
| During | 11.35 ± 3.05 | 13.45 ± 3.27 | 0.04 |
| 1 min | 6.6 ± 3.27 | 9.1 ± 3.23 | 0.02 |
| 5 min | 4.15 ± 1.87 | 6.3 ± 3.06 | 0.01 |
| PIPP score . | Breast milk (Mean ± SD) . | Standard care (Mean ± SD) . | p-value . |
|---|---|---|---|
| Baseline | 2.8 ± 1.24 | 3.3 ± 1.17 | 0.19 |
| During | 11.35 ± 3.05 | 13.45 ± 3.27 | 0.04 |
| 1 min | 6.6 ± 3.27 | 9.1 ± 3.23 | 0.02 |
| 5 min | 4.15 ± 1.87 | 6.3 ± 3.06 | 0.01 |
Breast milk significantly decreased pain during and 1 min and 5 min after the procedure.
DISCUSSION
Our study showed that EBM and 25% dextrose significantly reduced the PIPP scores during nasopharyngeal suctioning. There did not appear to be any superiority of one over the other—both 25% dextrose and breast milk reduced pain similarly. This is in accordance with a study by Axelin et al. [3] who used 24% dextrose and found a significant decrease in PIPP scores during oropharyngeal suctioning. Their study population was similar to ours in terms of birth weight (mean 1123 g) and gestation (mean 28 weeks). Vezyroglou et al. [12] reported no decrease in PIPP scores when 20% glucose was applied orally during oropharyngeal suctioning. This difference in results may be owing to a lower concentration of dextrose and higher birth weight and gestation.
The recent Cochrane meta-analysis shows that sucrose is a good analgesic for procedural pain but naso- or oropharyngeal suctioning in particular has not been studied [18]. Another study using dextrose also showed beneficial effects on pain during heel lance [19]. There have been some concerns raised about the safety of repeated doses of sucrose given to preterms [20]. A few studies have shown poorer neurodevelopmental outcomes when >10 doses were used [21]. Despite increasing awareness about the need for neonatal analgesia, newborns still appear to undergo >11 painful procedures a day [7].
Breast milk, in numerous trials, has been shown to decrease pain during various procedures [22]. To our knowledge, this is the first trial to assess the efficacy of breast milk during suctioning. When compared with the standard of care, PIPP scores were significantly lower during the procedure and up to 5 min after the procedure. In this regard, breast milk appeared to be superior to 25% dextrose in the sustainability of its actions. The analgesic effect of EBM, which contains a disaccharide—lactose—is probably based on the link between the oro-gustatory effects of sweet solution given orally and the endogenous opioid pathway. In all probability, this is due to the sweet taste perception, a sense well developed even in premature infants at birth [23]. Breast milk also contains tryptophan, which could lead to higher levels of beta endorphins, thereby decreasing pain [24, 25].
There are several scores to assess neonatal pain. Among them, we have experienced using the PIPP score [14, 15, 26], and hence, this was chosen. Vezyroglou et al. [12] had also used the same score while Axelin et al. [3] used the Neonatal Infant Pain Scale. A possible limitation of the use of PIPP could be that minimum saturations are one of the parameters used to calculate the total score. During this study, once the CPAP was removed, if the baby desaturated to < 85%, free flow oxygen was used. This may alter the score. However, the same procedure was done for all babies, in both groups and during standard care.
We found that nasopharyngeal suctioning causes moderate to severe pain (PIPP > 12). These results were similar to other studies [3, 4, 12]. One study showed PIPP scores of 8, suggesting moderate pain [12], while another study using salivary cortisol, showed a lack of a stress response to suctioning [27]. A Swiss study showed that both nasopharyngeal suctioning and installation of CPAP prongs cause moderate pain [28, 29].
Despite significantly decreasing pain during suctioning, both breast milk and 25% dextrose were not able to ameliorate pain—it only decreased from severe to moderate. Probably, this degree of pain requires a multimodal approach, that is, breast milk and facilitated tuck (holding the infant by placing a hand on his or her hands and feet and by positioning the infant in a flexed midline position while in a side-lying, supine, or prone position). Future studies incorporating this may provide evidence for its use.
In conclusion, both 25% dextrose and breastmilk significantly decreased pain associated with oropharyngeal suctioning. Breast milk, however, showed a more sustained benefit for up to 5 min.
With the increasing use of non-invasive ventilation for preterm neonates, we recommend the use of oral EBM before nasopharyngeal suctioning. This will significantly decrease pain and may enable better intact neurological outcomes.


Comments