-
PDF
- Split View
-
Views
-
Cite
Cite
M Y Rao, Y L Wang, G R Zhang, Y Zhang, T Liu, A J Guo, L Li, K Zhou, M Wang, Thrombolytic therapy to the patients with de Winter electrocardiographic pattern, is it right?, QJM: An International Journal of Medicine, Volume 111, Issue 2, February 2018, Pages 125–127, https://doi.org/10.1093/qjmed/hcx253
Close - Share Icon Share
Learning points for clinicians
The de Winter ECG pattern is one of the STEMI equivalents which deserves emergent reperfusion therapy. Two patients with de Winter pattern benefited from the thrombolytic therapy and recovered well. So, we think that thrombolytic therapy may be a choice for de Winter pattern patients when cardiac catheterization laboratory can’t be activated emergently.
Case report
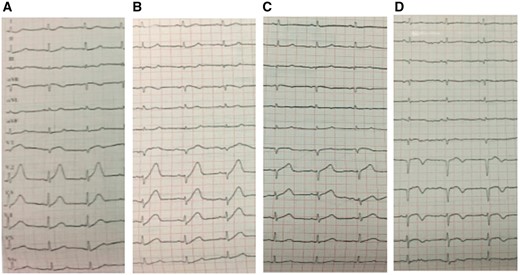
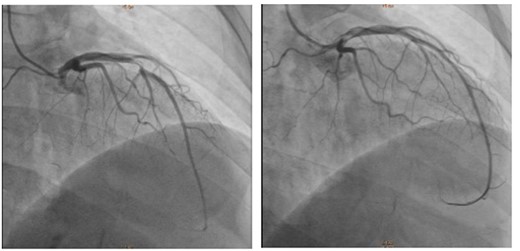
A 60-year-old male was presenting with chest tightness and substernal chest pain for 70 min, with previous typical anginal symptoms in the past 5 years without consulting a physician. The first ECG (Figure 1A) was performed at the emergency room, which showed slight ST depression at the J point in precordial leads V3–V6, with upsloping ST segments continuing into tall, symmetrical T waves and ST elevation 0.1 mV in leads aVR. Then the patient was diagnosed with non-STEMI, then oral aspirin and clopidogrel and subcutaneous low molecular weight heparin injection were administered. Another ECG (Figure 1B) was performed at third hour and his symptoms without alleviation. Based on the prediagnosis of recognizing the de Winter ECG pattern and we gave him thrombolytic therapy with prourokinase. His symptoms relieved 1 h later and dynamic changes showed in ECG (Figure 1C), which revealed ST segment back to baseline in V2 through V6. Echocardiography showed anterior wall hypokinesis with normal left venticular ejection fraction. The next day, the coronary angiography revealed a 90% stenosis of the middle of the left anterior descending (Figure 2) and then the patient underwent post thrombolysis percutaneous coronary intervention. The ECG (Figure 1D) recorded after the procedure.
(A) Electrocardiogram performed approximately 70 min after onset of pain. (B) Electrocardiogram at the 3rd h with persisting ischemic pain. (C) Electrocardiogram 1 h after the thrombolytic therapy. (D) Electrocardiogram after the PCI.
Cardiac catheterization showing a 90% stenosis of the middle of the left anterior descending (left) and after a drug-eluting stent placement (right).
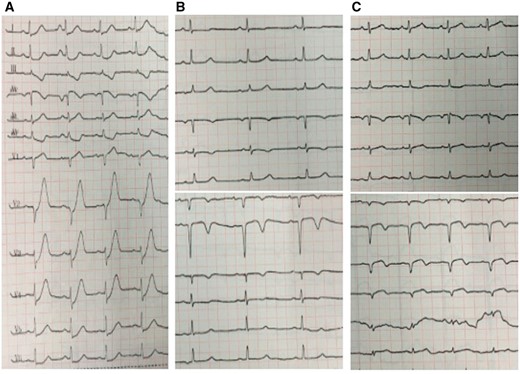
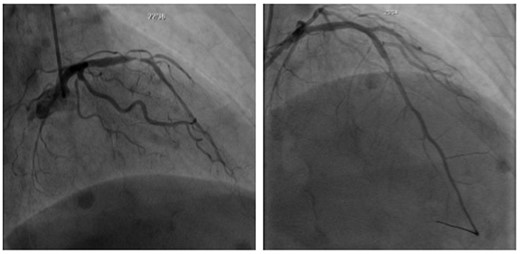
The second case was a 52-year-old woman with no relevant history, who was admitted with 3 h history of chest pain, radiating to the left upper extremity and left shoulder and back, accompanied with nausea and vomit. The first ECG (Figure 3A) performed showed ST-segment depression of up to 3 mm after the J point, with minimal Q wave, loss of R wave progression, and prominent T waves in the precordial leads, ST elevation in lead aVR and ST-segment depression in the inferior leads. Recognizing the de Winter ECG pattern and suggested the patient for immediate reperfusion therapy, we gave him thrombolytic therapy with prourokinase. Her symptoms subsided 2 h later and ECG showed significant changes in Figure 3B. All lab workup values were within normal limits except for elevated myocardial enzyme and troponin. Echocardiography showed anterior wall hypokinesis with normal left ventricular ejection fraction. The next day, Coronary angiography showed a 90% stenosis of the proximal left anterior descending artery and a 90% stenosis of the proximal first diagonal branch (Figure 4). The lesion was treated by implantation of two drug-eluting stents. The ECG recorded after the procedure showed in Figure 3C.
(A) Electrocardiogram at the 3 h after onset of pain. (B) Electrocardiogram 2 h after the thrombolytic therapy. (C) Electrocardiogram after the PCI.
Cardiac catheterization showing a 90% stenosis of the proximal left anterior descending artery and a 90% stenosis of the proximal first diagonal branch (left) and after two drug-eluting stents placement (right).
Discussion
STE in lead aVR with multilead STD has been described for patients with occlusion of left main, proximal LAD, and MI in the presence of multivessel coronary artery disease. Because these patients have a higher mortality in the setting of MI, this ECG finding should be considered a STEMI equivalent and that patients with this finding deserves emergent reperfusion therapy preferably at a center with both primary percutaneous coronary intervention and coronary artery bypass grafting capability. Zhao et al. suggested that patients showing the de Winter ECG pattern should receive follow-up treatment in accordance with the STEMI guidelines.1 When timely PCI is not available, thrombolytic therapy in patients with ongoing symptoms suggestive of acute MI can be considered.2 In our two patients, their symptoms resolved in 1–2 h after receiving thrombolytic therapy and normalization of the ST segment in 12 leads. They benefited from the thrombolytic therapy and recovered well with normal left ventricular function, without manifestations of heart failure during follow-up. Therefore, we think it is right to administer thrombolytic therapy to the patients with de Winter electrocardiographic pattern.
Conflict of interest: None declared.