-
PDF
- Split View
-
Views
-
Cite
Cite
Nikolaos Baritakis, Nikolaos Grapsas, Andreas Kotsalos, Periklis Davlouros, An uncommon variant of double-chambered right ventricle masquerading as double-chambered left ventricle, Interactive CardioVascular and Thoracic Surgery, Volume 26, Issue 2, February 2018, Pages 350–352, https://doi.org/10.1093/icvts/ivx287
Close - Share Icon Share
Abstract
We present a rare case of a double-chambered right ventricle masquerading as a double-chambered left ventricle, which was found incidentally on cardiac imaging in an adult female patient with atypical chest pain. The most common form of double-chambered right ventricle is characterized by compartmentalization of the right ventricle by muscular bands into 2 distinct chambers. The main features of this malformation are a pressure gradient between the 2 compartments, and the frequent (up to 90%) association with a membranous ventricular septal defect. In our case, the muscular band dividing the right ventricle was located in the inferoseptal part of the latter, creating a diminutive cavity that had no communication with the main right ventricle but communicated with the left ventricle creating the false impression of a double-chambered left ventricle. This constitutes a rare variant of double-chambered right ventricle with unknown clinical implications.
This is a case report of a 62-year-old woman who underwent an echocardiogram due to an atypical chest pain with a complete left bundle branch block in the surface electrocardiogram. The pain characteristics pointed out a probable musculoskeletal aetiology, whereas physical examination, medical history and family history were unremarkable.
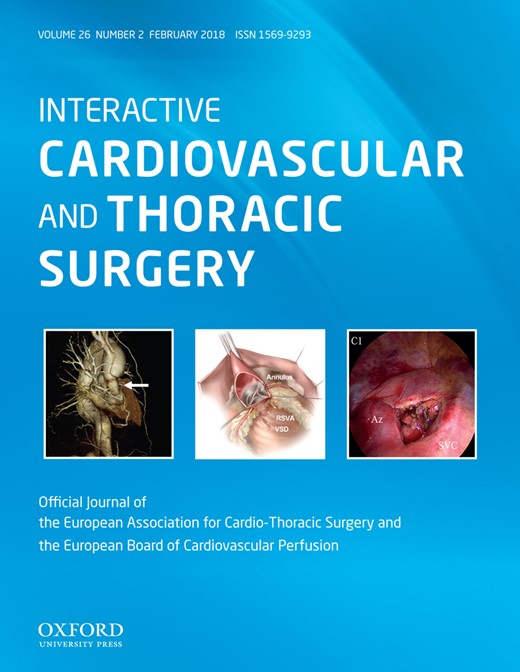
The echocardiogram demonstrated 2 muscular bands, a thicker muscular band on the left, corresponding to the interventricular septum, and a thinner muscular band on the right, which created a small aberrant cavity between the left ventricle (LV) and the right ventricle (RV) (Fig. 1A). Bubbles injected via the left antecubital vein were restricted to the RV, creating the impression that the aberrant cavity was in fact an accessory LV (Fig. 1B). A cardiac magnetic resonance study followed (Fig. 2, Videos 1 and 2) showing that a small smoothly bordered and well-contracting cavity (RV2) was located between the main RV (RV1) and the LV. A ventricular septal defect in the basal interventricular septum allowed communication between the diminutive RV2 and the LV. RV1 was anatomically and functionally normal. The left main coronary artery and the right coronary artery originated from the left sinus of Valsalva and the right sinus of Valsalva, respectively.
Double-chambered right ventricle. (A and B) Subcostal views showing an ‘aberrant’ cavity located between the right ventricle and the left ventricle. Following bubble injection via a left antecubital vein, this cavity (RV2) did not communicate with the main RV (RV1). LV: left ventricle; RV: right ventricle; RA: right atrium; LVOT: left ventricular outflow tract.
Double-chambered right ventricle. (A and B) Short-axis views showing the main LV, with its normal interventricular septum [interventricular septum (IVS), yellow arrows] and a much smaller cavity (RV2), which is separated from the main RV (RV1) by a relatively thin myocardial wall [(4, 5 mm in thickness) (black arrows)] and becomes more apparent at the medial and apical parts of the heart. The smaller cavity (RV2) has an end-diastolic volume of 15 ml and an end-systolic volume of 9 ml [ejection fraction (EF) = 38%], whereas the LV has an end-diastolic volume of 103 ml and an end-systolic volume of 35 ml (EF = 65%). (C and D) Late gadolinium enhancement imaging showing that there is no evidence of scar or fibrosis, even in the thinner parts of the RV2 ‘free wall’ (black arrows on C and D). The RV2 communicates with the LV through a non-restrictive defect in the basal membranous part (yellow arrow on D) of the IVS. LV: left ventricle; RV: right ventricle; LGE: late gadolinium enhancement.
Double-chambered right ventricle. Short-axis view of magnetic resonance imaging.
Double-chambered right ventricle. Long-axis view of magnetic resonance imaging.
Our initial impression based on the bubble study, and the absence of communication between the small cavity and the main RV, was that this case represented a double-chambered left ventricle, a rare congenital malformation with only a few cases reported in the literature [1] However, the fact that the muscular band dividing the RV is located to the right of the interventricular septum, and the reduced ejection fraction of the small cavity on the cardiac magnetic resonance study compared with the left ventricular ejection fraction, led us to the conclusion that our case could represent an even more rare cardiac malformation, namely a double-chambered right ventricle (DCRV) masquerading as a double-chambered left ventricle [2–4]. The ‘classic’ DCRV is characterized by an intraventricular pressure gradient created by anomalous hypertrophic muscular bands [2, 3]. It is a rare congenital heart defect (0.5–2.0%) most frequently diagnosed in infants and children [3]. It has been speculated that abnormal flow in the RV outflow tract may be causally associated with DCRV, leading to abnormal muscle hypertrophy (mainly involving the crista supraventricularis), thus it may be discovered even some years following ventricular septal defect repair [3]. Surgical excision of the muscular bands, which has excellent long-term results [5], is indicated in symptomatic patients and/or in patients with a significant intraventricular pressure gradient, as the latter may lead to RV pressure loading and ultimately to RV failure [3]. However, a rare variant of DCRV (anomalous apical shelf) has been described, in which a prominent septoparietal band with high take-off, along with hypertrophic apical trabeculations, formed an apical muscle shelf dividing the apical RV into 2 pouches, with only 1 communicating with the RV outlet, thus giving the impression of a double-chambered left ventricle [2, 4]. The clinical implications of this rare DCRV variant, which we believe our case also represents are largely unknown, as there is no communication between the 2 parts of the RV, therefore no pressure gradient exists. For the same reason, there should not be any impact of a coexistent ventricular septal defect on the pulmonary circulation even if the former is non-restrictive. Indeed, our patient went through the adult life being completely asymptomatic. The chest pain syndrome of the patient was rather musculoskeletal, and the patient was discharged without further diagnostic investigations or medical therapy.
Conflict of interest: none declared.



![Double-chambered right ventricle. (A and B) Short-axis views showing the main LV, with its normal interventricular septum [interventricular septum (IVS), yellow arrows] and a much smaller cavity (RV2), which is separated from the main RV (RV1) by a relatively thin myocardial wall [(4, 5 mm in thickness) (black arrows)] and becomes more apparent at the medial and apical parts of the heart. The smaller cavity (RV2) has an end-diastolic volume of 15 ml and an end-systolic volume of 9 ml [ejection fraction (EF) = 38%], whereas the LV has an end-diastolic volume of 103 ml and an end-systolic volume of 35 ml (EF = 65%). (C and D) Late gadolinium enhancement imaging showing that there is no evidence of scar or fibrosis, even in the thinner parts of the RV2 ‘free wall’ (black arrows on C and D). The RV2 communicates with the LV through a non-restrictive defect in the basal membranous part (yellow arrow on D) of the IVS. LV: left ventricle; RV: right ventricle; LGE: late gadolinium enhancement.](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/icvts/26/2/10.1093_icvts_ivx287/1/m_ivx287f2.jpeg?Expires=1716440508&Signature=mclRW-a9Rwd0KvL6REeRVlVAAeu7AMkzmmgg1Zq5rvZva8XuC5YnsOxLT6k9zkEgodbTENm3YFwZzEQ9BHLxxSltzkD43rYd7S5KFoKNukXoMFEWJ64tCBzjnMqCEJPdEcz5L9I~Sc7vP0na2eFhVnseL8gSCzG8-g1mLjct9HSE7d~V6qflJcqIecMEpukx4aWZcr2oGpwdrlPV4s1JhYrTmOF0UlghjimwHpeUP9nXSH1hVKjB-ebM89tcE8wafndC6W9Noa1OZxb1bPBCKRPNPi2GgFHrboelOslaCrPaX9gwn0VO0bFTuvyNzV2-ZQ6xZv~2P2fCAb01AnSwTQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
