-
PDF
- Split View
-
Views
-
Cite
Cite
Clare Bambra, Debbie Fox, Alex Scott-Samuel, Towards a politics of health, Health Promotion International, Volume 20, Issue 2, June 2005, Pages 187–193, https://doi.org/10.1093/heapro/dah608
Close - Share Icon Share
Abstract
The importance of public policy as a determinant of health is routinely acknowledged, but there remains a continuing absence of mainstream debate about the ways in which the politics, power and ideology, which underpin public policy influence people's health. This paper explores the possible reasons behind the absence of a politics of health and demonstrates how explicit acknowledgement of the political nature of health will lead to more effective health promotion strategy and policy, and to more realistic and evidence-based public health and health promotion practice.
INTRODUCTION
It is profoundly paradoxical that, in a period when the importance of public policy as a determinant of health is routinely acknowledged, there remains a continuing absence of mainstream debate about the ways in which the politics, power and ideology, which underpin it influence people's health. For a rare example see Navarro and Shi (Navarro and Shi, 2001). While to some extent the unhealthy policies of the Reagan and Thatcher governments of 20 years ago acted as a stimulus to such debate, as early as the mid-1980s, the introduction of the World Health Organization's Health For All strategy (World Health Organization, 1985) created the illusion that these issues had finally—and adequately—been acknowledged. Experience since then suggests that such views can and very clearly should be challenged.
In this article we argue that health, and its promotion, are profoundly political. We explore the possible reasons behind the absence of a ‘politics of health’ in mainstream debate and demonstrate how an awareness of the political nature of health will lead to a more effective health promotion strategy and more evidence-based health promotion practice.
THE POLITICAL NATURE OF HEALTH
It is time that the implicit, and sometimes explicit but unstated politics within and surrounding health were more widely acknowledged. Health, like almost all other aspects of human life, is political in numerous ways:
Health is political because, like any other resource or commodity under a neo-liberal economic system, some social groups have more of it than others.
Health is political because its social determinants are amenable to political interventions and are thereby dependent on political action (or more usually, inaction).
Health is political because the right to ‘a standard of living adequate for health and well-being’ (United Nations, 1948) is, or should be, an aspect of citizenship and a human right.
Ultimately, health is political because power is exercised over it as part of a wider economic, social and political system. Changing this system requires political awareness and political struggle.
Health inequalities
Evidence that the most powerful determinants of health in modern populations are social, economic and cultural (Doyal and Pennell, 1979; Townsend and Davidson, 1992; Whitehead, 1992; Blane et al., 1996; Acheson, 1998) comes from a wide range of sources and is also, to some extent, acknowledged by governments and international agencies (Townsend and Davidson, 1992; Acheson, 1998; Department of Health, 1998; Social Exclusion Unit, 1998). Yet inequalities in health continue, within countries (on the basis of socio-economic class, gender or ethnicity) and between them (in terms of wealth and resources) (Davey Smith et al., 2002; Donkn et al., 2002).
How these inequalities in health are approached by society is highly political: are health inequalities to be accepted as ‘natural’ and inevitable results of individual differences both in respect of genetics and the silent hand of the economic market, or are they social and economic abhorrences that need to be tackled by a modern state and a humane society (Adams et al., 2002)? Underpinning these different approaches to health inequalities are not only divergent views of what is scientifically or economically possible, but also differing political and ideological opinions about what is desirable.
Health determinants
Causes of, and genetic predispositions to ill-health are becoming increasingly well understood. However, it is evident that in most cases, environmental triggers are equally if not more important and that the major determinants of health or ill-health are inextricably linked to social and economic context (Acheson, 1998; Marmot and Wilkinson, 2001). Factors such as housing, income and employment—indeed many of the issues that dominate political life—are key determinants of our health and well-being. Similarly, many of the major determinants of health inequalities lie outside the health sector and therefore require non-health sector policies to tackle them (Townsend and Davidson, 1992; Acheson, 1998; Whitehead et al., 2000). Recent acknowledgements of the importance of the social determinants of health are welcome but fail to seriously address the underlying political determinants of health and health inequity.
Citizenship
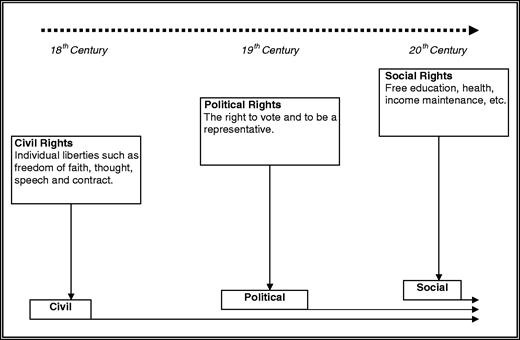
Citizenship is ‘a status bestowed on those who are full members of a community. All who possess the status are equal with respect to the rights and duties with which the status is endowed’ (Marshall, 1963). There are three types of citizenship rights: civil, political and social. Health, or the ‘right to a standard of living adequate for health and well-being’ (United Nations, 1948; International Forum for the Defense of the Health of People, 2002), is an important social citizenship right. These citizenship rights were only gained as a result of extensive political and social struggle during Western industrialization and the development of capitalism (Marshall, 1963). However, despite their parallel development (see Figure 1), the relationship between capitalism and citizenship is not an easy or ‘natural’ one (Marshall, 1963). Health is a strong example of this tense relationship as under a capitalist economic system health is, like everything else, commodified. Commodification is ‘the process whereby everything becomes identifiable and valued according to its relative desirability within the economic market (of production and consumption)’ (de Viggiani, 1997). Health became extensively commodified during the industrial revolution as workers became entirely dependent upon the market for their survival (Esping-Andersen, 1990). In the 20th century, the introduction of social citizenship, which entailed an entitlement to health and social welfare, brought about a ‘loosening’ of the pure commodity status of health. The welfare state decommodified health because certain health services and a certain standard of living became a right of citizenship.
The historical development of citizenship (adapted from Marshall, 1963).
In short, capitalism and citizenship represent very different values: the former, inequality and the latter, equality. This tension means that the implementation of the right to health, despite its position in social citizenship and in the UN Universal Declaration of Human Rights, will for the foreseeable future require continuing political struggle.
WHY HAS HEALTH BEEN APOLITICAL?
It is perhaps puzzling that despite its evident political nature, the politics of health has been underdeveloped and marginalized: it has not been widely considered or discussed as a political entity within academic debates or, more importantly, broader societal ones. There is no simple explanation for this omission; the treatment of health as apolitical is almost certainly the result of a complex interaction of issues. We describe some of these below, though we would not claim that our list is exhaustive.
Health = health care
Health is often reduced and misrepresented as health care (or in the UK, as the National Health Service). Consequently, the politics of health becomes significantly misconstructed as the politics of health care—see for example Freeman (Freeman, 2000). As an illustration, the majority of popular UK political discussions about health concern issues such as the ‘State or the market?’ debate about National Health Service (NHS) funding, organization and delivery, or the demographic pressures on the future provision of healthcare facilities (Rhodes, 1997). The same applies in most other—especially ‘developed’—countries.
The limited, one-dimensional (Carpenter, 1980) nature of this political discourse surrounding health can be traced back to two ideological issues: the definition of health and the definition of politics. The definition of health that has conventionally been operationalized under Western capitalism has two interrelated aspects to it: health is both considered as the absence of disease (biomedical definition) and as a commodity (economic definition). These both focus on individuals, as opposed to society, as the basis of health: health is seen as a product of individual factors such as genetic heritage or lifestyle choices, and as a commodity that individuals can access either via the market or the health system (Scott-Samuel, 1979). This remains the case despite our sophisticated understanding of health promotion—as is evident if one ignores the rhetoric of the governments of ‘developed’ nations and looks instead at their health policies.
Health in this sense is an individualized commodity that is produced and delivered by the market or the health service. Inequalities in the distribution of health are therefore either a result of the failings of individuals through, for example, their lifestyle choices; or of the way in which health care products are produced, distributed and delivered. In order to tackle these inequalities, political attention is directed towards the variable that is most amenable to manipulation—the healthcare system.
It is important to note that this limiting, one-dimensional view of health is common across the ideological spectrum, with left-wing versus right-wing health debates usually consisting of a more versus less state intervention dichotomy. Orthodox UK left-wing politics is guilty of placing health care and the NHS at the centre of its discussions and struggles about health. This ‘NHS illusion’ has resulted in the naive perspective amongst health activists that societal ill-health can be cured by more and better NHS services. At best, this perspective is slowly changing, as is shown by the enthusiasm of some in the UK for New Labour's emphasis on tackling health inequalities through the NHS—while it simultaneously widens them through its neo-liberal macroeconomic, trade and foreign policies (Bambra et al., 2003).
Health and politics
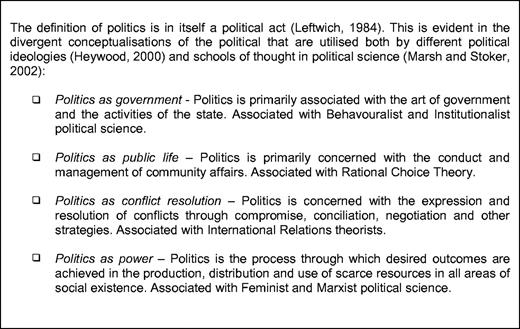
Figure 2 outlines four broad definitions of politics. The first concept, which is the most prevalent definition within mainstream political discourse, places very restrictive boundaries around what politics is—the activities of governments, elites and state agencies—and therefore also restricts who is political and who can engage in politics (i.e. the members of governments, state agencies and other elite organizations). It is a ‘top-down’ approach that essentially separates politics from the community. This should be contrasted with the last definition, which offers a much more encompassing view of politics: politics is everything; it is a term that can be used to describe any ‘power-structured relationship’ (Millett, 1969). This is a ‘bottom-up’ approach as any and every issue is political and likewise anyone and everyone can engage in a political act.
The dominance of the first conceptualization of politics, as the art of government and the activities of the state, influences which aspects of health are considered to be political. Health care, especially in countries like the UK where the state's role is significant, is an immediate subject for political discussion. Other aspects of health, such as health inequalities or health and citizenship, are excluded from this narrow popular definition of politics and are thereby seen as non-political. In order to increase which aspects of health are regarded as political, our understanding of politics needs to be contested and redefined.
Health and political science
Health has not been seriously studied within political science—nor for that matter, with a handful of exceptions (Signal, 1998; McGinnis et al., 2002; Navarro, 2002), has politics within health promotion. This has compounded its exclusion from the political realm. Health to a political scientist, in common with more widely held views, most often means only one thing: health care; and usually, only one minor aspect of health care: the health care system. Some political scientists will argue that they do study health as a political entity; however, what is actually under analysis is the politics of health care.
The roots of this focus on health care derive from the dominance of certain schools of thought within political science and of their corresponding definitions of the political. Figure 2 outlined the different schools of thought in political science and their respective conceptualizations of politics. These schools are not of equal weight within political science and the discipline is dominated, especially in the USA, by the behavouralist, institutionalist and rational choice strands. To adherents of these schools politics—and therefore political science—is concerned with the processes, conditions and institutions of mainstream politics and government. The politics of health care is therefore the politics of institutions, systems, funding and elite interactions. Health, in its broader sense, is therefore apolitical and should only be the concern of disciplines such as sociology, public health or medicine. In this way specified aspects of health, namely health care issues, are politically defined as political while all other aspects are not.
Responsibility and authority
The conceptualization of health as non-political is also in part due to medicalization—the transfer of power over and responsibility for health from individuals, the public and therefore political life, to powerful elites, namely the medical and health professions and the multinational pharmaceutical companies.
When we conceive of ill-health as episodes of disease manageable by the delivery of healthcare, we are … transferring the responsibility for health from society as a whole to an elite possessing what we define as the necessary professional and technical expertise for the management of disease (Scott-Samuel, 1979).
However, unlike the impression given in the above quote, this transfer of responsibility is not always voluntary. Drug companies and the medical profession have taken the power and responsibility for health for themselves (Illich, 1977). They have thus been able to determine what health is and therefore, how political it is (or, more usually, is not).
Their historic power over the definition and management of health has contributed substantially to its depoliticization: health is something that doctors are responsible for, they are the providers, and we are the recipients. Their authority and responsibility over health has further emphasized its commodity status—when ill, an individual visits a doctor and/or purchases drugs (commodity) to regain health (another, albeit less obvious commodity). Ill-health is a transient state caused by the presence of disease. It can be ended by the appropriate application of medical technology. This depoliticization of health, via the transfer of power and responsibility to these professional and/or commercial groups, means that we do not acknowledge our power over our own health or our autonomy over our own bodies.
Health policy
Health policy, as currently popularly conceptualized, is usually synonymous with policy content. Certainly, it is relatively unusual to find discussions of health policy that are not focused on the pros and cons of particular courses of action in relation to particular political parties. In reality, however, health policy is part of a broader public policy agenda, whose practical aspects are inextricably linked with power and politics. Given this, the reduction of ‘health policy’ to ‘the content of health policies’ diverts attention from, and renders invisible the political nature of the policy process. Policy is formulated within certain preset political parameters, which define what is, and what is not, possible or acceptable. For example, the fundamental requirement within Western neo-liberal economies for inequality (between those who labour and those who profit) makes the meaning of UK government policies to ‘tackle inequalities’ at best highly questionable—no modern government will support a policy process that permits the full implementation of radical equity policy. Government policy in this area therefore consists of (loudly trumpeted) minor reform; no policy connections are ever made with the macro-political causes of the major economic, social and health inequalities, such as macroeconomic policy, trade policy, defence policy, foreign policy and international development. For example, none of these featured in the UK Treasury's Cross Cutting Spending Review on Health Inequalities (HM Treasury and Department of Health, 2002), which was intended to examine the impact on health inequalities of the expenditure programmes of all government departments. Nor are the actions of the World Trade Organization, of trans-national corporations, or of the World Bank usually taken into account. One conclusion regarding this failure to see the wood for the trees is that there is an important need for awareness of how the political context limits how health policy is formulated. Another is that this failure does not occur by chance: both the masking of the political nature of health, and the forms of the social structures and processes that create, maintain and undermine health, are determined by the individuals and groups that wield the greatest political power.
TOWARDS A POLITICS OF HEALTH
What this all adds up to is nothing less than a challenge to a wide range of actors—health promotion and public health specialists, policy makers, politicians, health and political scientists—to emerge from the closet and to begin the long overdue task of elaborating the practice, policy and theory of a newly identified discipline—health politics, the political science of health. We believe that we have more than adequately justified the need for health politics to emerge as a discipline and field of practice no less important than medical sociology or health economics on the one hand, or than political sociology or political psychology on the other. We are confident that the practice of health promotion and public health will gain immeasurably from the explicit recognition of this key determinant of health and its incorporation into evidence-based strategies, policies and interventions.
We acknowledge the helpful comments of an anonymous referee.
REFERENCES
Acheson, D. (Chairman) (
Adams, L., Amos, M. and Munro, J. (eds) (
Bambra, C., Fox, D. and Scott-Samuel, A. (
Blane, D., Brunner, E. and Wilkinson, R. (eds) (
Davey Smith, G., Dorling, D., Mitchell, R. and Shaw, M. (
Donkn, A., Goldblatt, P. and Lynch, K. (
HM Treasury and Department of Health (
International Forum for the Defense of the Health of People (
Marmot, M. and Wilkinson, R. (
Marsh, D. and Stoker, G. (eds) (
Marshall, T. H. (
McGinnis, J. M., Williams-Russo, P. and Knickman, J. R. (
Navarro, V. (
Navarro, V. and Shi, L. (
Rhodes, M. (
Signal, L. (
Social Exclusion Unit (
Townsend, P. and Davidson, N. (
United Nations (
Whitehead, M. (
Whitehead, M., Diderichsen, F. and Burstrom, B. (
Author notes
1Department of Sociology and Social Policy, Sheffield Hallam University, Sheffield, UK and 2Department of Public Health, University of Liverpool, Liverpool, UK