-
PDF
- Split View
-
Views
-
Cite
Cite
J N Siewe Fodjo, F Mubiru, C Ukaga, M Y Logora, B P Mmbando, M Mandro, A K Njamnshi, R Colebunders, Low ivermectin use among 5- to 6-year-old children: observations from door-to-door surveys in onchocerciasis-endemic regions in Africa, International Health, Volume 12, Issue 1, January 2020, Pages 72–75, https://doi.org/10.1093/inthealth/ihz044
Close - Share Icon Share
Abstract
During door-to-door surveys in onchocerciasis-endemic regions in Africa, the age-specific ivermectin coverage in 29 722 individuals was assessed. Children 5–6 y of age had significantly lower coverage compared with older participants. Insufficient ivermectin intake among young children could prolong onchocerciasis elimination prospects, as they may serve as human reservoirs of Onchocerca volvulus; moreover, it increases the risk of developing onchocerciasis-associated epilepsy (OAE). The causes of the low ivermectin coverage observed among children 5–6 y of age need to be explored. Integrating ivermectin distribution into chemoprophylaxis strategies for other neglected diseases could increase coverage in a cost-effective manner.
Introduction
The World Health Organization (WHO) recommends mass drug administration (MDA) as a strategy for the control and/or elimination of several neglected tropical diseases (NTDs). Cohn et al.,1 in a study investigating gender equity during MDA in 16 countries, showed that male coverage was lower than female coverage for all diseases including onchocerciasis. Using the same statistical approach as Cohn et al., we report a similar gender imbalance for ivermectin MDA coverage in several onchocerciasis-endemic communities in six African countries. In addition, an investigation of ivermectin use by age showed an overall lower coverage among younger participants compared with older age groups.
Data sources and methods
Our data were obtained during door-to-door surveys performed within a multicountry project to investigate the link between onchocerciasis and epilepsy. Study sites were onchocerciasis-endemic regions located in the Bas Uélé province (Aketi2 and Titule3) and the Tshopo and Ituri provinces4 of the Democratic Republic of Congo; the Mahenge area in Tanzania5; Maridi county in South Sudan6; the Kitgum, Pader and Moyo districts in northern Uganda7; the Imo River Basin in Nigeria8 and the Sanaga Valley (Kelleng) and Mbam Valley (Bilomo) in Cameroon.9 During house visits, a research team collected sociodemographic information from every household member and asked whether he/she took ivermectin during the most recent MDA session. Parents were asked about the intake of ivermectin by their children. To calculate the gender-specific coverage, we proceeded like Cohn et al.1 by excluding pregnant women from the denominator, based on data obtained from recent demographic surveys in each country (see Supplementary material). Only data from participants ≥5 y of age were analysed. National MDA coverage data for the different countries and years were obtained from the WHO website (http://apps.who.int/gho/cabinet/pc.jsp). Ivermectin coverage in our study sites was compared with the age-disaggregated nationwide MDA coverage for the schistosomiasis and soil-transmitted helminths programmes in order to examine the trends of MDA coverage for different programmes among school-aged children. Proportions were compared using the χ2 test.
Results and discussion
We observed an overall low self-reported annual ivermectin intake that was significantly lower in children 5–10 y of age (2720/6457 [42.1%]) compared with older age groups (14 318/23 265 [61.5%]) (p<0.001). Site-specific data are presented in Table 1, which show that the coverage was generally lowest in children 5–10 y of age. Analyses within this age group further showed that ivermectin use among 5-year-olds (209/1052 [19.9%]) and 6 y olds (368/1073 [34.3%]) was much lower compared with children 7–10 y of age (2143/4332 [49.5%]) (p<0.001). Furthermore, ivermectin coverage in children 6–7 y of age (who were most likely 5–6 y of age during the previous MDA) was 862/2223 (38.8%), still considerably lower than in older age groups (p<0.001). Ivermectin coverage was high even among children 5–10 y of age in only Uganda and Nigeria, where MDA is done biannually.
Ivermectin coverage in eight onchocerciasis-endemic study sites in Africa
| Study site (year of MDAa) . | Previous MDA . | Age-specific ivermectin coverage (%) . | |||||
|---|---|---|---|---|---|---|---|
| 5–10 y . | 11–20 y . | 21–30 y . | 31–40 y . | >40 y . | p-Value . | ||
| All sites (2013–2018) | 1–8 months ago | 2720/6457 (42.1) | 5173/8722 (59.3) | 3060/5217 (58.7) | 2328/3719 (62.6) | 3757/5607 (67.0) | <0.001 |
| Titule, DRC (2013) | 5 months ago | 259/544 (47.6) | 390/667 (58.5) | 239/428 (55.8) | 159/296 (53.7) | 244/469 (52.0) | |
| Tshopo/Ituri, DRC (2014) | 7 months ago | 254/580 (43.8) | 398/873 (45.6) | 220/484 (45.5) | 239/448 (53.3) | 416/708 (58.8) | |
| Tanzania (2016) | 8 months ago | 606/901 (67.3) | 934/1132 (82.5) | 524/692 (75.7) | 424/531 (79.8) | 891/1078 (82.7) | |
| Aketi, DRC (2017) | 4 months ago | 109/189 (57.7) | 121/158 (76.6) | 77/111 (69.4) | 79/107 (73.8) | 109/153 (71.2) | |
| Cameroon (2017) | 1–6 months ago | 175/295 (59.3) | 211/312 (67.6) | 124/200 (62.0) | 93/168 (55.4) | 214/323 (66.3) | |
| South Sudan (2017) | 5 months ago | 904/3484 (25.9) | 2450/4871 (50.3) | 1482/2871 (51.6) | 1053/1861 (56.6) | 1311/2227 (58.9) | |
| Uganda (2017) | 4 months ago | 360/400 (90.0) | 569/593 (96.0) | 280/305 (91.8) | 180/186 (96.8) | 296/316 (93.7) | |
| Nigeria (2018) | 1 month ago | 53/64 (82.8) | 100/116 (86.2) | 114/126 (90.5) | 101/122 (82.8) | 276/333 (82.9) | |
| Gender-specific ivermectin coverageb | |||||||
| Coverage among males: 8249/14 270 (57.8) | Coverage among females: 8733/13 086 (66.7)c | <0.001 | |||||
| Overall ivermectin coverage | |||||||
| Took ivermectin: 17 038/29 722 (57.3) | |||||||
| Study site (year of MDAa) . | Previous MDA . | Age-specific ivermectin coverage (%) . | |||||
|---|---|---|---|---|---|---|---|
| 5–10 y . | 11–20 y . | 21–30 y . | 31–40 y . | >40 y . | p-Value . | ||
| All sites (2013–2018) | 1–8 months ago | 2720/6457 (42.1) | 5173/8722 (59.3) | 3060/5217 (58.7) | 2328/3719 (62.6) | 3757/5607 (67.0) | <0.001 |
| Titule, DRC (2013) | 5 months ago | 259/544 (47.6) | 390/667 (58.5) | 239/428 (55.8) | 159/296 (53.7) | 244/469 (52.0) | |
| Tshopo/Ituri, DRC (2014) | 7 months ago | 254/580 (43.8) | 398/873 (45.6) | 220/484 (45.5) | 239/448 (53.3) | 416/708 (58.8) | |
| Tanzania (2016) | 8 months ago | 606/901 (67.3) | 934/1132 (82.5) | 524/692 (75.7) | 424/531 (79.8) | 891/1078 (82.7) | |
| Aketi, DRC (2017) | 4 months ago | 109/189 (57.7) | 121/158 (76.6) | 77/111 (69.4) | 79/107 (73.8) | 109/153 (71.2) | |
| Cameroon (2017) | 1–6 months ago | 175/295 (59.3) | 211/312 (67.6) | 124/200 (62.0) | 93/168 (55.4) | 214/323 (66.3) | |
| South Sudan (2017) | 5 months ago | 904/3484 (25.9) | 2450/4871 (50.3) | 1482/2871 (51.6) | 1053/1861 (56.6) | 1311/2227 (58.9) | |
| Uganda (2017) | 4 months ago | 360/400 (90.0) | 569/593 (96.0) | 280/305 (91.8) | 180/186 (96.8) | 296/316 (93.7) | |
| Nigeria (2018) | 1 month ago | 53/64 (82.8) | 100/116 (86.2) | 114/126 (90.5) | 101/122 (82.8) | 276/333 (82.9) | |
| Gender-specific ivermectin coverageb | |||||||
| Coverage among males: 8249/14 270 (57.8) | Coverage among females: 8733/13 086 (66.7)c | <0.001 | |||||
| Overall ivermectin coverage | |||||||
| Took ivermectin: 17 038/29 722 (57.3) | |||||||
Values presented as n/N (%).
DRC: Democratic Republic of Congo.
aYear of MDA: year for which the MDA coverage was assessed by our team.
b61 missing data.
cThe denominator excludes an estimated proportion of pregnant women, based on recent Demographic Health Surveys in each country.
Ivermectin coverage in eight onchocerciasis-endemic study sites in Africa
| Study site (year of MDAa) . | Previous MDA . | Age-specific ivermectin coverage (%) . | |||||
|---|---|---|---|---|---|---|---|
| 5–10 y . | 11–20 y . | 21–30 y . | 31–40 y . | >40 y . | p-Value . | ||
| All sites (2013–2018) | 1–8 months ago | 2720/6457 (42.1) | 5173/8722 (59.3) | 3060/5217 (58.7) | 2328/3719 (62.6) | 3757/5607 (67.0) | <0.001 |
| Titule, DRC (2013) | 5 months ago | 259/544 (47.6) | 390/667 (58.5) | 239/428 (55.8) | 159/296 (53.7) | 244/469 (52.0) | |
| Tshopo/Ituri, DRC (2014) | 7 months ago | 254/580 (43.8) | 398/873 (45.6) | 220/484 (45.5) | 239/448 (53.3) | 416/708 (58.8) | |
| Tanzania (2016) | 8 months ago | 606/901 (67.3) | 934/1132 (82.5) | 524/692 (75.7) | 424/531 (79.8) | 891/1078 (82.7) | |
| Aketi, DRC (2017) | 4 months ago | 109/189 (57.7) | 121/158 (76.6) | 77/111 (69.4) | 79/107 (73.8) | 109/153 (71.2) | |
| Cameroon (2017) | 1–6 months ago | 175/295 (59.3) | 211/312 (67.6) | 124/200 (62.0) | 93/168 (55.4) | 214/323 (66.3) | |
| South Sudan (2017) | 5 months ago | 904/3484 (25.9) | 2450/4871 (50.3) | 1482/2871 (51.6) | 1053/1861 (56.6) | 1311/2227 (58.9) | |
| Uganda (2017) | 4 months ago | 360/400 (90.0) | 569/593 (96.0) | 280/305 (91.8) | 180/186 (96.8) | 296/316 (93.7) | |
| Nigeria (2018) | 1 month ago | 53/64 (82.8) | 100/116 (86.2) | 114/126 (90.5) | 101/122 (82.8) | 276/333 (82.9) | |
| Gender-specific ivermectin coverageb | |||||||
| Coverage among males: 8249/14 270 (57.8) | Coverage among females: 8733/13 086 (66.7)c | <0.001 | |||||
| Overall ivermectin coverage | |||||||
| Took ivermectin: 17 038/29 722 (57.3) | |||||||
| Study site (year of MDAa) . | Previous MDA . | Age-specific ivermectin coverage (%) . | |||||
|---|---|---|---|---|---|---|---|
| 5–10 y . | 11–20 y . | 21–30 y . | 31–40 y . | >40 y . | p-Value . | ||
| All sites (2013–2018) | 1–8 months ago | 2720/6457 (42.1) | 5173/8722 (59.3) | 3060/5217 (58.7) | 2328/3719 (62.6) | 3757/5607 (67.0) | <0.001 |
| Titule, DRC (2013) | 5 months ago | 259/544 (47.6) | 390/667 (58.5) | 239/428 (55.8) | 159/296 (53.7) | 244/469 (52.0) | |
| Tshopo/Ituri, DRC (2014) | 7 months ago | 254/580 (43.8) | 398/873 (45.6) | 220/484 (45.5) | 239/448 (53.3) | 416/708 (58.8) | |
| Tanzania (2016) | 8 months ago | 606/901 (67.3) | 934/1132 (82.5) | 524/692 (75.7) | 424/531 (79.8) | 891/1078 (82.7) | |
| Aketi, DRC (2017) | 4 months ago | 109/189 (57.7) | 121/158 (76.6) | 77/111 (69.4) | 79/107 (73.8) | 109/153 (71.2) | |
| Cameroon (2017) | 1–6 months ago | 175/295 (59.3) | 211/312 (67.6) | 124/200 (62.0) | 93/168 (55.4) | 214/323 (66.3) | |
| South Sudan (2017) | 5 months ago | 904/3484 (25.9) | 2450/4871 (50.3) | 1482/2871 (51.6) | 1053/1861 (56.6) | 1311/2227 (58.9) | |
| Uganda (2017) | 4 months ago | 360/400 (90.0) | 569/593 (96.0) | 280/305 (91.8) | 180/186 (96.8) | 296/316 (93.7) | |
| Nigeria (2018) | 1 month ago | 53/64 (82.8) | 100/116 (86.2) | 114/126 (90.5) | 101/122 (82.8) | 276/333 (82.9) | |
| Gender-specific ivermectin coverageb | |||||||
| Coverage among males: 8249/14 270 (57.8) | Coverage among females: 8733/13 086 (66.7)c | <0.001 | |||||
| Overall ivermectin coverage | |||||||
| Took ivermectin: 17 038/29 722 (57.3) | |||||||
Values presented as n/N (%).
DRC: Democratic Republic of Congo.
aYear of MDA: year for which the MDA coverage was assessed by our team.
b61 missing data.
cThe denominator excludes an estimated proportion of pregnant women, based on recent Demographic Health Surveys in each country.
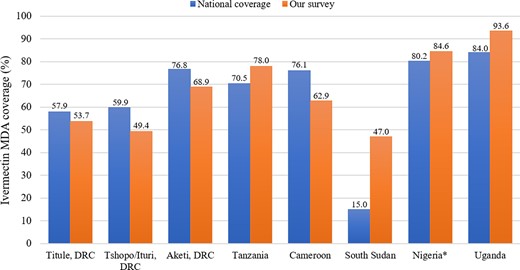
Our findings seemed comparable with national ivermectin coverage trends in the respective countries for the corresponding study years, except for a much higher coverage reported by our team in South Sudan (Figure 1). Considering the school-aged participants (5–14 y of age), the coverage for ivermectin-only MDA was generally lower in our study sites compared with the national ivermectin coverage achieved via an integrated approach (ivermectin distributed alongside other drugs for NTD chemoprophylaxis); our reported coverage also fell below the countrywide praziquantel MDA coverage for schistosomiasis control, suggesting that in most countries, poor MDA adherence by school-aged children may be more pronounced specifically for ivermectin monotherapy (Table 2).
Comparison of our findings with national ivermectin MDA coverage. *Nigeria national ivermectin coverage for the year 2017 was used.
Comparative MDA coverage among school-age children
| Study site (year of MDA)a . | MDA coverage among children 5–14 y of age (%) . | ||
|---|---|---|---|
| Ivermectin onlyb (for onchocerciasis) . | Ivermectin + albendazolec (for soil-transmitted helminthiasis) . | Praziquantelc (for schistosomiasis) . | |
| DRC (2013) | 52.0 | NA | NA |
| DRC (2014) | 44.3 | 77.7 | 74.6 |
| Tanzania (2016) | 74.9 | 81.0 | 97.6 |
| DRC (2017) | 63.5 | 93.9 | 79.6 |
| Cameroon (2017) | 64.0 | 88.1 | 100.0 |
| South Sudan (2017) | 33.6 | NA | NA |
| Uganda (2017) | 92.7 | 80.4 | 63.7 |
| Nigeria (2018) | 82.2 | 96.1* | 74.1* |
| Study site (year of MDA)a . | MDA coverage among children 5–14 y of age (%) . | ||
|---|---|---|---|
| Ivermectin onlyb (for onchocerciasis) . | Ivermectin + albendazolec (for soil-transmitted helminthiasis) . | Praziquantelc (for schistosomiasis) . | |
| DRC (2013) | 52.0 | NA | NA |
| DRC (2014) | 44.3 | 77.7 | 74.6 |
| Tanzania (2016) | 74.9 | 81.0 | 97.6 |
| DRC (2017) | 63.5 | 93.9 | 79.6 |
| Cameroon (2017) | 64.0 | 88.1 | 100.0 |
| South Sudan (2017) | 33.6 | NA | NA |
| Uganda (2017) | 92.7 | 80.4 | 63.7 |
| Nigeria (2018) | 82.2 | 96.1* | 74.1* |
DRC: Democratic Republic of Congo; NA: not available.
aYear of MDA: year for which the MDA coverage was assessed by our team.
bIvermectin coverage as reported by our door-to-door surveys.
cNational MDA coverage obtained from the WHO website (http://apps.who.int/gho/cabinet/pc.jsp).
*Reports for the year 2017, because 2018 findings were not available.
Comparative MDA coverage among school-age children
| Study site (year of MDA)a . | MDA coverage among children 5–14 y of age (%) . | ||
|---|---|---|---|
| Ivermectin onlyb (for onchocerciasis) . | Ivermectin + albendazolec (for soil-transmitted helminthiasis) . | Praziquantelc (for schistosomiasis) . | |
| DRC (2013) | 52.0 | NA | NA |
| DRC (2014) | 44.3 | 77.7 | 74.6 |
| Tanzania (2016) | 74.9 | 81.0 | 97.6 |
| DRC (2017) | 63.5 | 93.9 | 79.6 |
| Cameroon (2017) | 64.0 | 88.1 | 100.0 |
| South Sudan (2017) | 33.6 | NA | NA |
| Uganda (2017) | 92.7 | 80.4 | 63.7 |
| Nigeria (2018) | 82.2 | 96.1* | 74.1* |
| Study site (year of MDA)a . | MDA coverage among children 5–14 y of age (%) . | ||
|---|---|---|---|
| Ivermectin onlyb (for onchocerciasis) . | Ivermectin + albendazolec (for soil-transmitted helminthiasis) . | Praziquantelc (for schistosomiasis) . | |
| DRC (2013) | 52.0 | NA | NA |
| DRC (2014) | 44.3 | 77.7 | 74.6 |
| Tanzania (2016) | 74.9 | 81.0 | 97.6 |
| DRC (2017) | 63.5 | 93.9 | 79.6 |
| Cameroon (2017) | 64.0 | 88.1 | 100.0 |
| South Sudan (2017) | 33.6 | NA | NA |
| Uganda (2017) | 92.7 | 80.4 | 63.7 |
| Nigeria (2018) | 82.2 | 96.1* | 74.1* |
DRC: Democratic Republic of Congo; NA: not available.
aYear of MDA: year for which the MDA coverage was assessed by our team.
bIvermectin coverage as reported by our door-to-door surveys.
cNational MDA coverage obtained from the WHO website (http://apps.who.int/gho/cabinet/pc.jsp).
*Reports for the year 2017, because 2018 findings were not available.
The very low ivermectin intake observed among children 5–10 y of age is a public health concern because this population may constitute human reservoirs for the parasite, thus disrupting onchocerciasis elimination prospects due to continued transmission. In addition, ivermectin could protect these children from developing onchocerciasis-related conditions, including onchocerciasis-associated epilepsy (OAE).10 The reasons for this low coverage need to be further investigated. However, we will suggest some of the factors that, in our opinion, may be contributing to the observed pattern. It is possible that, at the moment of the epilepsy surveys, some of the 5-year-old children were still 4 y old during the previous round of ivermectin distribution, considering that 5 y is the age at which children are eligible to take ivermectin. Another explanation could be that parents, due to the fear of side effects, are reluctant to have their 5- and 6-year-old children take a drug that is not recommended until the age of 5; they would rather play it safe and have them take the drug when a little older. Furthermore, we observed in our study sites that it is not uncommon for parents, particularly fathers, to underestimate the age of their children; thus they may report that a child is 4 y old and therefore not eligible to receive ivermectin, when in fact the child is 5.
Our findings can hardly be generalized to all onchocerciasis foci because all our study sites were purposefully selected from meso- or hyperendemic areas. In such settings with a history of high onchocerciasis transmission, children are exposed to Onchocerca volvulus from an early age. It is likely that early infection with high microfilarial densities predisposes children to OAE and subsequent blindness in the following decades if nothing is done. Although children generally develop OAE at >5 y of age, OAE onset has been reported even around the age of 3 y.4 Therefore we recommend that clinical trials be conducted to determine the safety of ivermectin/moxidectin when administered to children <5 y of age. Importantly, adopting an integrated MDA strategy and increasing ivermectin treatment frequency in areas with high onchocerciasis transmission would help increase coverage, curtail transmission and better protect this vulnerable age group.
Authors’ contributions: CR, SFJN, MF, LMY, UC, MBP, MM and NAK participated in protocol development and/or data collection. SFJN analysed the data. CR and SFJN wrote the first draft. All authors revised the initial draft and approved the final manuscript.
Acknowledgements: We thank all the local research teams and populations that participated in the surveys.
Funding: CR received funding from the European Research Council (grant ERC 671055).
Competing interests: None declared.
Ethical approval: All participating households and individuals provided a signed/thumb-printed written informed consent. Ethical approval was obtained for all the studies mentioned in this article from the ethical committee of the University of Antwerp and from the following local ethical committees: Titule, 2013: Institutional Review Board of the University of Kisangani, DRC; Tshop/Ituri, 2014: Institutional Review Board of Ngaliema Hospital, Kinshasa, DRC; Mahenge, 2016: ethics committee of the National Institute for Medical Research, Tanzania; Aketi, 2017: Ethics Review Board of the School of Public Health of the University of Kinshasa, DRC; Cameroon, 2017: National Ethics Committee, Yaoundé, Cameroon; South Sudan, 2017: ethics committee of the Ministry of Health, South Sudan; Uganda, 2017: ethical committee of Lacor Hospital, Gulu, Uganda; and Nigeria, 2018: ethical committee of Imo State University, Nigeria.




Comments