Risk factors for implant-related fractures after proximal femoral osteotomy in children with developmental dysplasia of the hip: a case-control study
DOI:
https://doi.org/10.1080/17453674.2020.1848315Abstract
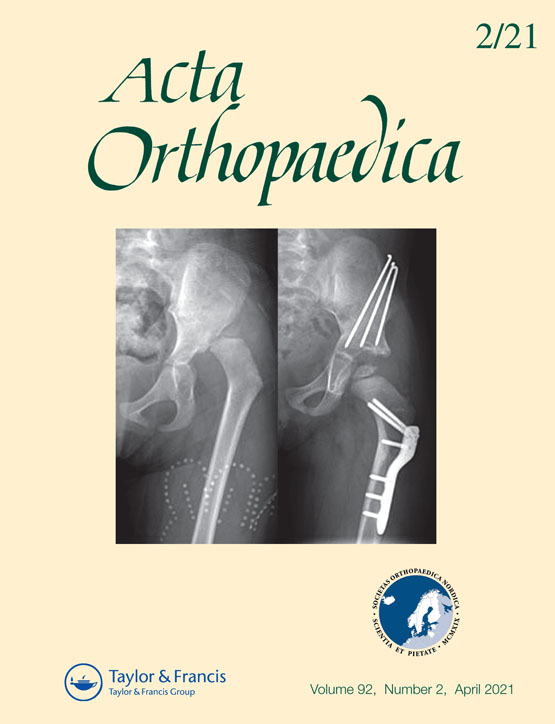
Background and purpose — Proximal femoral osteotomy (PFO) is commonly performed to treat children with developmental dysplasia of the hip (DDH). Implant-related femoral fractures after osteotomy are sometimes reported, but the potential risk factors for these fractures remain unclear. We investigated the association of implant-related fractures with PFO and potential risk factors for these fractures.
Patients and methods — We retrospectively reviewed 1,385 children undergoing PFO for DDH in our institution from 2009 to 2016 after obtaining institutional review board (IRB) approval and identified 27 children (28 hips, fracture group) with implant-related femoral fractures after PFO. We selected 137 children (218 hips, control group) without fractures who matched the children in the fracture group by age, weight, surgeon, and surgical period. Relevant clinical data were collected and compared between the 2 groups. Multiple analyses of risk factors for implant-related fractures were conducted by logistic regression with the stepwise regression
method.
Results — The occurrence rate of implant-related fractures was 1.9% (27/1,385). Compared with the control group, the fracture group more commonly exhibited bilateral involvement (74% vs. 53%, p = 0.04), used a spica orthosis for immobilization after osteotomy (43% vs 21%, p = 0.01) and exhibited mild remodeling at the osteotomy site (46% vs. 19%, p = 0.003), and less commonly required capsulotomy during osteotomy (61% vs. 79%, p = 0.03). According to the multiple regression analysis, the only factor identified as
an independent risk factor for implant-related fractures was mild remodeling at the osteotomy site (OR = 3.2, 95% CI 1.4–7.5). Remodeling at the osteotomy site was significantly associated with varus osteotomy (coefficient = 1.4, CI 1.03–1.8). The fracture occurred at a mean of 12 months (2.2–25) after osteotomy or 3.3 months (0–12) after implant removal. In children undergoing implant removal, the fractures mostlyoccurred at the osteotomy site (n = 13/15), while in those with the implant remaining, the fractures mostly occurred in the screw hole (n = 8/13).
Interpretation — The type of PFO performed is not associated with implant-related fractures in children with DDH. Children with mild remodeling at the osteotomy site should be closely followed up, regardless of whether the hardware is removed, and high-intensity activity should not be permitted until moderate or extensive remodeling is confirmed. After PFO, the implants should be removed when solid union is achieved at the osteotomy site.
Downloads
Downloads
Additional Files
Published
How to Cite
Issue
Section
License
Copyright (c) 2020 Jing Ding, Zhen-Zhen Dai, Zhu Liu, Zhen-Kai Wu, Zi-Ming Zhang, Hai Li

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.