Abstract
OBJECTIVE: To determine the incidence and variability of antibiotic use in facilities which provide chronic care and to determine how often clinical criteria for infection are met when antibiotics are prescribed in these facilities.
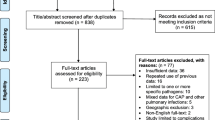
DESIGN: A prospective, 12-month, observational cohort study.
SETTING: Twenty-two facilities which provide chronic care in southwestern Ontario.
PARTICIPANTS: Patients who were treated with systemic antibiotics over the study period.
MEASUREMENTS: Characteristics of antibiotic prescriptions (name, dose, duration, and indication) and clinical features of randomly selected patients who were treated with antibiotics.
RESULTS: A total of 9,373 courses of antibiotics were prescribed for 2,408 patients (66% of the patients in study facilities). The incidence of antibiotic prescriptions in the facilities ranged from 2.9 to 13.9 antibiotic courses per 1,000 patient-days. Thirty-six percent of antibiotics were prescribed for respiratory tract infections, 33% for urinary infections, and 13% for skin and soft tissue infections. Standardized surveillance definitions of infection were met in 49% of the 1,602 randomly selected patients who were prescribed antibiotics. Diagnostic criteria for respiratory, urinary, and skin infection were met in 58%, 28%, and 65% of prescriptions, respectively. One third of antibiotic prescriptions for a urinary indication were for asymptomatic bacteriuria. Adverse reactions were noted in 6% of prescriptions for respiratory and urinary infections and 4% of prescriptions for skin infection.
CONCLUSIONS: Antibiotic use is frequent and highly variable amongst patients who receive chronic care. Reducing antibiotic prescriptions for asymptomatic bacteriuria represents an important way to optimize antibiotic use in this population.
Similar content being viewed by others
References
Mylotte JM. Measuring antibiotic use in a long-term care facility. Am J Infect Control. 1996;24:174–9.
Montgomery P, Semenchuk M, Nicolle LE. Antimicrobial use in nursing homes in Manitoba. J Geriatr Drug Ther. 1995;9:55–74.
Warren JW, Palumbo FB, Fitterman L, Speedie SM. Incidence and characteristics of antibiotic use in aged nursing home patients. J Am Geriatr Soc. 1991;39:963–72.
Katz PR, Beam TR, Brand F, Boyce K. Antibiotic use in the nursing home. Physician practice patterns. Arch Intern Med. 1990;150:1465–8.
Smith PW. Nursing home infection control: a status report. Infect Control Hosp Epidemiol. 1998;19:366–9.
Goldmann DA, Weinstein RA, Wenzel RP, et al. Strategies to prevent and control the emergence and spread of antimicrobial-resistant microorganisms in hospitals. A challenge to hospital leadership. JAMA. 1996;275:234–40.
Armstrong-Evans M, Litt M, McArthur MA, et al. Control of transmission of vancomycin-resistant Enterococcus faecium in a long-term-care facility. Infect Control Hosp Epidemiol. 1999;20:312–7.
Greenaway CA, Miller MA. Lack of transmission of vancomycin-resistant enterococci in three long-term-care facilities. Infect Control Hosp Epidemiol. 1999;20:341–3.
Wiener J, Quinn JP, Bradford PA, et al. Multiple antibiotic-resistant Klebsiella and Escherichia coli in nursing homes. JAMA. 1999;281:517–23.
Terpenning MS, Bradley SF, Yan JY, Chenoweth CE, Jorgensen KA, Kauffman CA. Colonization and infection with antibiotic-resistant bacteria in a long-term care facility. J Am Geriatr Soc. 1994;42:1062–9.
Wingard E, Shlaes JH, Mortimer EA, Shlaes DM. Colonization and cross-colonization of nursing home patients with trimethoprim-resistant gram-negative bacilli. Clin Infect Dis. 1993;16:75–81.
Chenoweth CE, Bradley SF, Terpenning MS, et al. Colonization and transmission of high-level gentamicin-resistant enterococci in a long-term care facility. Infect Control Hosp Epidemiol. 1994;15:703–9.
Gaynes RP, Weinstein RA, Chamberlin W, Kabins SA. Antibiotic-resistant flora in nursing home patients admitted to the hospital. Arch Intern Med. 1985;145:1804–7.
Rice LB, Willey SH, Papanicolaou GA, et al. Outbreak of ceftazidime resistance caused by extended-spectrum B-lactamases at a Massachusetts chronic-care facility. Antimicrob Agents Chemother. 1990;34:2193–9.
Muder RR, Brennen C, Goetz AM, Wagener MM, Rihs JD. Association with prior fluoroquinolone therapy of widespread ciprofloxacin resistance among gram-negative isolates in a Veterans Affairs medical center. Antimicrob Agents Chemother. 1991;35:256–8.
Nicolle LE, Bentley D, Garibaldi R, Neuhaus E, Smith P. Antimicrobial use in long-term care facilities. Infect Control Hosp Epidemiol. 1996;17:119–28.
Nicolle LE, Strausbaugh LJ, Garibaldi RA. Infections and antibiotic resistance in nursing homes. Clin Microbiol Rev. 1996;9:1–17.
Strausbaugh LJ, Joseph C. In: Mayhall CG, ed. Hospital Epidemiology and Infection Control. Baltimore, Md: Williams and Wilkins; 1996:1151–70.
Zimmer JG, Bentley DW, Valenti WM, Watson NM. Systemic antibiotic use in nursing homes. A quality assessment. J Am Geriatr Soc. 1986;34:703–10.
Jones SR, Parker DF, Liebow ES, Kimbrough RC, Frear RS. Appropriateness of antibiotic therapy in long-term care facilities. Am J Med. 1987;83:499–502.
McGeer A, Campbell B, Emori TG, et al. Definitions of infection for surveillance in long-term care facilities. Am J Infect Control. 1991;19:1–7.
Chambers LW, Labelle R, Gafni A, Goeree R. The Organization and Financing of Public and Private Sector Long Term Care Facilities for the Elderly in Canada, Chapter 6: Ontario Report. McMaster University Centre for Health Economics and Policy Analysis Working Paper 92-8; 1992.
Nicolle LE. Asymptomatic bacteriuria in the elderly. Infect Dis Clin North Am. 1997;11:647–62.
Nicolle LE, Bjornson J, Harding GK, MacDonnel JA. Bacteriuria in elderly institutionalized men. N Engl J Med. 1983;309:1420–5.
Nicolle LE, Mayhew JW, Bryan L. Prospective randomized comparison of therapy and no therapy for asymptomatic bacteriuria in institutionalized elderly women. Am J Med. 1987;83:27–33.
Ouslander JG, Schapira JF, Schnelle JF, et al. Dose eradicating bacteriuria affect the severity of chronic urinary incontinence in nursing home residents? Ann Intern Med. 1995;122:749–54.
Abrutyn E, Mossey J, Berlin JA, et al. Does asymptomatic bacteriuria predict mortality and does antimicrobial treatment reduce mortality in elderly ambulatory women. Ann Intern Med. 1994;120:827–33.
Garner JS, Bennett JV, Schechler WE, et al. Surveillance of nosocomial infections. In: Brachman PS, Eichhoff TC, eds. Proceedings of the International Conference on Nosocomial Infections. Chicago: American Hospital Association; 1971.
Muder RR. Pneumonia in residents of long-term care facilities: epidemiology, etiology, management, and prevention. Am J Med. 1998;105:319–30.
Scully BE. Therapy of respiratory tract infections with quinolone antimicrobial agents. In: Hooper DC, Wolfson JS, eds. Quinolone Antimicrobial Therapy. 2nd ed. Washington, DC: American Society for Microbiology; 1993.
Chen DK, McGeer A, de Azavedo JC, Low DE. Decreased susceptibility of Streptococcus pneumoniae to fluoroquinolones in Canada. N Engl J Med. 1999;341:233–9.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by a grant from the Physicians Services Incorporated Foundation.
Rights and permissions
About this article
Cite this article
Loeb, M., Simor, A.E., Landry, L. et al. Antibiotic use in ontario facilities that provide chronic care. J GEN INTERN MED 16, 376–383 (2001). https://doi.org/10.1046/j.1525-1497.2001.016006376.x
Issue Date:
DOI: https://doi.org/10.1046/j.1525-1497.2001.016006376.x